Serial endothelial-cell-density and corneal-thickness measurements in corneas preserved in Optisol GS
Melville M. Martires, MD, Santiago Antonio B. Sibayan, MD, PhD, Ma. Elizabeth T. Concepcion, MD, Ma. Dominga B. Padilla, MD
MILLIONS of people worldwide suffer from opacities and deformities of the cornea, resulting in deficient light
transmission and blindness. Penetrating keratoplasty (PKP) is an operation that has enabled cornea-blind individuals to improve or regain their vision. In this procedure, diseased corneal tissue is removed and replaced by cadaveric donor corneal material. These donor corneas are harvested from the eyes of recently deceased individuals and transferred to nutrient solution until transplanted to a recipient. Endothelial cells line the inner surface of the cornea and are responsible for corneal nutrition and clarity. These cells do not divide and have a finite population. As a general rule, the lower the endothelial-cell density (ECD), the less viable is the cornea. ECD is, therefore, used as an indicator of corneal viability.
Although there is no established relationship between corneal thickness (CT) and graft survival, minimization
of corneal swelling following preservation is ideal. This allows for better immediate postoperative visual results.
Optisol GS (Bausch & Lomb, Irvine, CA, USA) is a corneal storage medium supplemented with dehydrating agents (dextran and chondroitin sulfate) that lessen swelling and maintain corneal clarity.
Corneas remain viable in a storage medium for a finite period due to endothelial-cell loss over time. A recent
literature search showed no available studies on the daily rate of ECD loss of donor corneas. Such data would be helpful in prognosticating the outcomes of those who underwent PKP. Thus, this study determined the daily
ECD change in Filipino donor corneas stored in Optisol GS. The change in CT was also evaluated.
METHODS
This is a prospective cohort study. A total of 28 donor corneas from 15 donors (mean age, 38 ± 13.78 years;
range, 4 to 78 years) were evaluated at the Santa Lucia International Eye Bank of Manila. All donor tissues met
the inclusion and exclusion criteria for human corneal transplantation (Table 1).
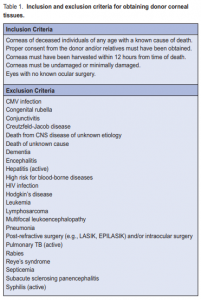

Figure 2. Serial photographs showing the absence of endothelial-cell-density changes over time.
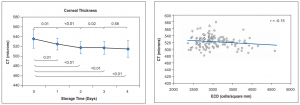
Figure 3. Line graph representing corneal thickness (CT) at various periods following Figure 4. Scatter plot correlating CT with ECD. corneal harvest. There were statistically significant decreases in CT compared to baseline on days 1 to 4 (p values indicated below line). When compared to the previous day’s readings, there were statistically significant decreases in CT on days 1 and 2. No further changes were observed on days 3 and 4 (p values indicated above line). Error bars = 1 standard error of the mean.
Figure 4. Scatter plot correlating CT with ECD.
After obtaining consent from the donor’s family, corneal tissue was retrieved by trained eye-bank personnel either by whole-globe enucleation or by in situ removal. Corneoscleral rims were then transferred to Optisol GS. Specular microscopy and pachymetry of the central corneal endothelium was performed daily in triplicate from preservation time to day 4 using a Konan Keratoanalyzer (Konan Medical, Hyogo, Japan). These readings were then averaged and subjected to statistical analysis. All measurements were performed by a single examiner (MMM). As corneas are generally shipped for use by the fifth day, no further readings were performed. Statistical analysis of ECD and CT was performed using student’s t-test. P values ≤ 0.05 were considered statistically significant. The relationship between CT and ECD was determined using Pearson’s correlation coefficient (r).
RESULTS
Endothelial-Cell Density and Storage Time There were no statistically significant changes in ECD
compared with baseline or the previous day’s readings (all p values > 0.05) (Figure 1). Serial photographs illustrate the absence of ECD changes over time (Figure 2).
Corneal Thickness and Storage Time There were statistically significant decreases in CT compared with baseline on days 1 to 4 (all p values < 0.05). Compared to the previous day’s readings, there were statistically significant decreases in CT on days 1 and 2 (all p values ≤ 0.01). No further changes were observed on days 3 and 4 (all p values > 0.05) (Figure 3). Corneal Thickness and Endothelial Cell Density Pearson’s correlation coefficient (r) measured –0.15, indicating a weak negative relationship between CT and ECD (Figure 4).
DISCUSSION
For donor corneas to remain viable after harvest, they must be preserved in a nutrient medium such as Optisol
GS. ECD determination using specular microscopic analysis serves as a measurement of the functional status of the endothelial cells and can serve as a measure of corneal button viability. A critical cell density is necessary to maintain corneal qualities necessary for successful transplantation. 7-8 Our study showed that ECD remains unchanged following preservation in Optisol GS at least up to 4 days following harvest. This suggests that the corneal endothelium is adequately preserved in Optisol GS and that the graft may remain suitable for transplantation for at least this length of time. CT was noted to decrease significantly over time. This
may be attributed to dehydrating agents (dextran and chondroitin sulfate) present in the medium. While there
is no established relationship between CT and graft survival, minimization of corneal swelling following preservation is ideal, as this allows better postoperative visual results. 9-11 Based on the correlation analysis, no definite relationship could be established between ECD and CT. This implies that ECD and CT are independent of each other.
In conclusion, over a period of 4 days of storage in Optisol GS, ECD remained stable and CT decreased.
These findings suggest that corneas preserved in Optisol GS remain viable and do not deteriorate for at least this length of time.
1. Thuret G, Chiquet C, Bernal F, el al. Prospective, randomized clinical and
endothelial evaluation of 2 storage times for corneal donor tissue in organ culture
at 31 degrees centigrade. Arch Ophthalmol 2003; 121: 442-450.

