Recalcitrant Gram-Positive Bacterial Keratitis Treated with Intrastromal Levofloxacin 1.5% Ophthalmic Solution: A Case Report and Review of Literature
Bobbie Marie M. Santos, MD, PhD1, Josept Mari S. Poblete, MD, PhD1, George Michael N. Sosuan, MD1, Pablito F. Sandoval Jr., MD1, Billie Jean T. Cordero MD1, David Ammiel R. Tirol V, MD1, Ruben Lim Bon Siong, MD1,2
1Department of Ophthalmology and Visual Sciences, University of the Philippines – Philippine General Hospital, Manila, Philippines
2Eye Institute, St. Luke’s Medical Center, Quezon City, Philippines
Correspondence: Bobbie Marie M. Santos, MD, PhD
Office Address: Department of Ophthalmology and Visual Sciences, Sentro Oftalmologico Jose Rizal, Philippine General Hospital, Taft Avenue, Ermita, Manila
Office Phone Number: +63285548400
Email Address: bobbiemariesantos@gmail.com
Disclosures: Dr. Ruben Lim Bon Siong is in the advisory board and is a speaker for Santen. Dr. Tirol and Dr. Cordero were also speakers for Santen. The rest of the authors do not have conflicts of interest to disclose. This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Infectious keratitis is a leading cause of corneal blindness in both developed and developing countries, particularly in South, South-East, and East Asia.1,2 Bacterial keratitis, one of the most common types of infectious keratitis, is typically managed with topical antibiotics because of their excellent bioavailability and ease of administration. However, with the rising problem of antibiotic resistance, cases may become severe and unresponsive to treatment, leading to complications such as descemetocele formation, corneal thinning, melting, and perforation.3-5 Tissue adhesive, amniotic membrane transplantation, platelet-rich fibrin membrane grafting, conjunctival flaps, corneal patch grafts, penetrating keratoplasty, and lamellar keratoplasty are among the treatment options for recalcitrant cases.5,6 However, these are restricted by availability and cost.
Intrastromal injection is a technique for delivering a higher concentration of antibiotics directly to the site of infection, particularly in cases of deep stromal disease refractory to topical therapy.4 While this approach is currently being used for fungal keratitis, there is paucity of data regarding the use of intrastromal antibiotics for bacterial keratitis. While there are a few case reports on this approach for infectious crystalline keratopathy, phacoemulsification wound abscess, and polymicrobial keratitis, the intrastromal antibiotics used in these cases were limited to cefuroxime, tobramycin, or moxifloxacin.7-11 To our knowledge, intrastromal injection of levofloxacin has not yet been documented in literature. In this report, we present two cases of Gram-positive recalcitrant bacterial keratitis complicated by risk of perforation that were successfully treated by incorporating repeated intrastromal injections of levofloxacin 1.5% ophthalmic solution in the medical management.
CASE PRESENTATION
Case 1
A previously healthy 39-year-old Filipino female consulted for corneal opacity on the left eye. Three weeks prior to consult, she developed foreign body sensation and redness on the left eye after riding a motorcycle without eye protection. She self-medicated with tetrahydrozoline hydrochloride eyedrops which only offered partial relief. One week later, she noted a corneal opacity on the left eye, prompting consult with a local ophthalmologist. She was prescribed gatifloxacin 0.3% eyedrops four times a day, which was instilled with good compliance. There was an increase in the size of the corneal opacity and development of photophobia and blurring of vision. She consulted at another ophthalmic clinic, where she was assessed to have a corneal ulcer on the left eye and was started on ofloxacin 0.3% eyedrops four times a day and dexpanthenol eye gel three times a day. The patient was then referred to our institution for further management. She had no history of contact lens use, ocular trauma, or surgery. She did not have co-morbidities or allergies.
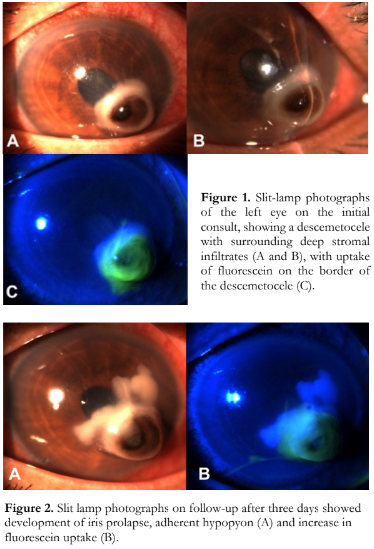
On initial consult, ocular examination revealed that the right eye had an uncorrected visual acuity (UCVA) of 20/20 and essentially unremarkable findings. The best-corrected visual acuity (BCVA) was 20/100 on the left eye. The pupil was 3 millimeters (mm), slightly corectopic and sluggishly reactive to light, without a relative afferent pupillary defect. The conjunctiva was hyperemic but there were no collarettes, discharge, lid abnormalities, lagophthalmos, and foreign bodies. Rebound tonometry showed intraocular pressure (IOP) of 10 mm Hg. Slit-lamp examination showed a 4.0 x 3.5 mm descemetocele at the inferonasal paracentral cornea. The descemetocele had surrounding stromal infiltrates and fluorescein dye uptake on its borders (Figure 1). The anterior chamber was formed, and Seidel’s test was negative. There was moderate anterior chamber activity of +3 cells but no hypopyon was seen. Gram stain of the corneal scrapings showed a few polymorphonuclear neutrophils and occasional Gram-positive cocci in pairs. There were no hyphal elements on Giemsa stain. There was no growth on culture. The patient was assessed to have Gram-positive bacterial keratitis with descemetocele on the left eye. The topical antibiotic was shifted from ofloxacin 0.3% to levofloxacin 1.5% every two hours on the left eye. After three days, there was a decrease in BCVA to 16/200, with a minimal increase of the corneal defect to 4.0 x 4.0 mm and iris prolapse (Figure 2). There was slight shallowing of the anterior chamber and minimal leak on Seidel’s test, however rebound tonometry on the left eye still showed IOP of 10 mm Hg. Anterior chamber activity decreased to +2 cells but an adherent hypopyon had developed. With worsening of the patient’s condition, the frequency of topical instillation of levofloxacin 1.5% was increased to every hour. In addition, intrastromal injection of levofloxacin 1.5% (Oftaquix 15 mg/ml ophthalmic solution, Santen Pharmaceutical Co., Ltd., Ishikawa, Japan) was done. Informed consent was obtained from the patient prior to delivering the antibiotic via an off-label route of administration. Under topical anesthesia, a total of approximately 0.1 ml of levofloxacin 1.5% was injected using a 30- gauge needle with the bevel up until the stroma appeared hydrated. Intrastromal injection was done at twelve, two, and nine clock hours of the descemetocele near the adherent hypopyon, avoiding the visual axis and areas of thinning.
On the 7th day of follow-up, the BCVA improved to 20/150 on the left eye. There was a noticeable decrease in the stromal infiltrates and adherent hypopyon. Seidel’s test was negative (Figure 3). The size of the defect, anterior chamber depth and activity, and IOP remained stable. Topical levofloxacin 1.5% was maintained hourly and a second round of intrastromal injection was done for the remaining stromal infiltrates. The patient was scheduled to follow-up after two days; however, she was unable to come back. The patient was compliant with hourly topical application for ten more days until the eyedrops were consumed.

On the 31st day of follow-up, the visual acuity had improved to 20/50 and there were no longer any infiltrates or hypopyon (Figure 4). With the resolution of the infiltrates, the antibiotic was shifted to topical levofloxacin 0.5% four times a day. On her last follow-up after two weeks, the iris was no longer prolapsed and there was no recurrence of the infiltrates (Figure 5).

On telemedicine follow-up seven months after the last intrastromal injection, the patient still noted blurring of vision on the left eye, but this was resolved by spectacles. She did not complain of recurrence of foreign body sensation, redness, or photophobia.
Case 2
A previously healthy 41-year-old Filipino female consulted for redness and burning sensation on her right eye. Six months prior to consult, while the patient was on her bed, a cat jumped on her face and scratched her right eye. She immediately noted eye pain, burning sensation, blurring of vision, and photophobia on the right eye. She consulted a local clinic and was given anti-rabies and tetanus vaccines, but no topical and oral medications were prescribed. After one month, she noted the development of a corneal opacity on her right eye which prompted her to consult a local ophthalmologist. She was given topical gatifloxacin every two hours and prednisolone acetate 1% four times a day for the right eye for one week, as well as oral cloxacillin 500 mg three times a day for five days, affording slight improvement in symptoms. The medications were shifted to tobramycin and dexamethasone drops every four hours for the next two weeks. Four months prior to consult, she reported a recurrence of eye redness and blurring of vision, for which prednisolone acetate 1% four times a day was prescribed for two weeks. She opted to consult another ophthalmologist due to the persistence of her eye symptoms. Erythromycin ointment three times a day on the right eye was prescribed. Nonetheless, there was no improvement of symptoms, prompting consult at our institution.
On initial consult, the left eye was unremarkable. Visual acuity was counting fingers at 6 inches for the right eye. There was no crusting, matting of lashes, or discharge. Slit-lamp examination revealed +3 diffuse conjunctival injection and a 5.0 mm x 5.0 mm round opacity on the central to inferonasal paracentral cornea. There was fluorescein staining with dense focal stromal infiltrates having well-defined borders with more than 50% stromal tissue loss (Figure 6). A 1.0 mm hypopyon was also noted. Gram stain of corneal scraping revealed encapsulated Gram-positive bacilli as well as encapsulated Gram-positive cocci in chains (Figure 7). Microbiological cultures yielded no growth. The patient was diagnosed to have chronic, indolent, bacterial keratitis on the right eye.

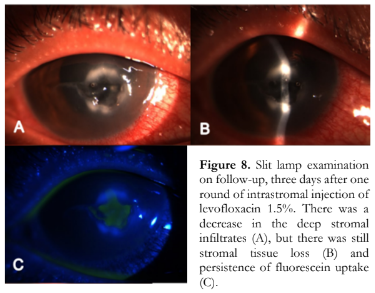
The patient was started on topical levofloxacin 1.5% 6 times day on the right eye, atropine 1% three times a day on the right eye, and oral doxycycline 100 mg twice a day. In addition, intrastromal injection of levofloxacin 1.5% was done with the patient’s consent. Under topical anesthesia, a total of approximately 0.1 ml of levofloxacin 1.5% was injected using a 30-gauge needle with the bevel up until the stroma appeared hydrated around the stromal infiltrates at twelve, three, and six clock hours. The topical steroid was discontinued. Three days later, she reported a decrease in redness and photophobia. Her visual acuity remained the same but there was a decrease in the stromal infiltrates and resolution of the hypopyon (Figure 8).
A repeat intrastromal injection of levofloxacin 1.5% was done on the same sites and the other medications were continued. One week later, vision improved to counting fingers at 3 feet. There was further decrease in the stromal infiltrates and resolution of the fluorescein uptake (Figure 9).

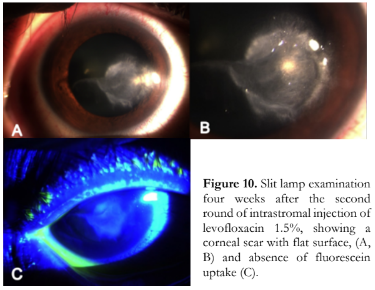
Topical levofloxacin 1.5% six times a day was continued, atropine 1% was tapered to once a day, and oral doxycycline was discontinued. The patient was started on prednisolone acetate 1% drops three times a day. The patient’s condition was continuously monitored. At 1 month, BCVA eventually improved to 20/22. Scarring and flattening of the previous excavation were noted (Figure 10), and the occurrence of corneal perforation was prevented.
DISCUSSION
In this paper, we report two cases of medically recalcitrant bacterial keratitis treated with off-label use of intrastromal levofloxacin 1.5% injection in addition to topical therapy. Several therapeutic challenges were identified in the management of these patients, including selection of an appropriate antibiotic to prevent development of bacterial resistance, impede progression and corneal perforation, and improve the outcomes of surgical interventions, if necessary. However, both cases of Gram-positive bacterial keratitis had become unresponsive even to a fourth-generation fluoroquinolone (FQ) like gatifloxacin which has improved Gram-positive coverage. Both patients received inconsistent treatment regimens administered by different physicians which may have contributed to the development of recalcitrant disease. In addition, the second patient received topical steroids early in the course which would have suppressed the immune response and contributed to the indolent nature of the infection. She also harbored a polybacterial infection consisting of Gram-positive bacilli and Gram-positive cocci which may have variable antibiotic susceptibilities.
Apart from FQs, fortified topical antibiotics such as cefazolin, vancomycin, and bacitracin are recommended as treatment for Gram-positive bacterial keratitis.6 However, another FQ in the form of levofloxacin at a higher concentration of 1.5% was chosen as adjunct therapy for these cases. Levofloxacin 1.5% has a better bioavailability with a reported 2-fold greater concentration in rabbit cornea and aqueous humor compared to 0.5% moxifloxacin and 0.3% gatifloxacin.12 Levofloxacin 1.5% also has significantly greater concentration in tears up to 24 hours after topical administration; the bactericidal activity of which remained above the 90% minimal inhibitory concentrations (MIC90) levels for common ocular pathogens including Staphylococcus and Streptococcus species.12 A recent meta-analysis also showed that levofloxacin 1.5% has shorter cure time and similar efficacy compared to fortified antibiotics.13 Despite reports of decreasing susceptibility of Gram-positive cocci to FQs since 2010, not all FQs have the same resistance rate.3 In a study conducted at the Philippine General Hospital, the resistance rate of Gram-positive cocci like S. aureus to levofloxacin was lower compared to gatifloxacin (MDB Padilla, personal communication, June 23, 2021). Moreover, in an in vitro study on human corneal endothelial cells and keratocytes, levofloxacin was found to be less cytotoxic than other FQs.14 Levofloxacin 1.5% administered topically in multiple daily doses also did not exhibit structural damage to treated rabbit corneas.15 Levofloxacin 1.5% was also found to be clinically well-tolerated and safe, with only 1-2% of patients reporting irritation at the site of instillation.12 Lastly, the standard doses of FQs are readily accessible as they are commercially available, whereas the other fortified antibiotics need to be compounded.
Despite initial topical administration with levofloxacin 1.5%, stromal keratitis progressed in Case 1, signifying a deep stromal disease. Both cases were complicated by a high risk for perforation, which required more aggressive management in the form of intrastromal drug delivery. Intrastromal injection of an antibiotic is not commonly used, because a high MIC can be achieved in the corneal stroma with topical administration alone, such as in the case of levofloxacin 1.5%.12 However, advantages of intrastromal injection include the ability to directly target the nidus of infection in deep stromal locations, reduction of bacterial load, and a shorter duration of treatment compared to a purely topical regimen.10,16 The literature on successful treatment of bacterial keratitis with intrastromal antibiotic injection is limited to only a handful of case reports. Cases of infectious crystalline keratopathy, which may be difficult to treat due to the presence of a biofilm that prevents antibiotics from reaching therapeutic levels, were successfully treated with intrastromal cefuroxime or moxifloxacin.7–9 Intrastromal tobramycin 0.3% has also been reported to treat a chronic deep stromal phacoemulsification wound-related bacterial keratitis.10 There was also a case of polymicrobial keratitis (penicillin-resistant S. aureus, pan-sensitive S. epidermidis, and Achromobactin species) which dramatically improved after 2 rounds of intrastromal injection of moxifloxacin 2 weeks apart.11 In our patients who had high-risk features for corneal rupture, we had a more aggressive approach employing a shorter interval of 3 days between injections. Additional considerations for this route of administration were patient non- compliance to eyedrops and poor follow-up.
In both cases, we did not observe any adverse events. Corneal scarring is common following an infection as a part of corneal healing. We also did not observe any crystalline deposits which has been reported following treatment with gatifloxacin and ciprofloxacin.17 This could be due to the less acidic pH of levofloxacin 1.5% at 6.5.18 Other possible adverse effects of intrastromal injection include Descemet membrane detachment, corneal perforation, endothelial decompensation, intrastromal bleeding, hyphema, and endophthalmitis.4,10 Patients must always be informed of the risks and the procedure must be performed with caution.
Despite promising results, more studies are needed to determine the minimum dose, injection volume, as well as specific bacteria for which intrastromal levofloxacin can be used effectively and safely.
In conclusion, the addition of intrastromal injection to topical administration of levofloxacin 1.5% was effective in treating deep recalcitrant bacterial keratitis caused by Gram-positive bacteria. Successful medical management of the keratitis was made possible by initially identifying the etiologic agent through Gram staining. This allowed targeted delivery of antibiotics to the site of infection, which provided greater coverage for Gram-positive bacteria, including resistant strains. The addition of intrastromal antibiotic injection led to faster resolution of the keratitis and eliminated the need for surgery.
REFERENCES
- Ting DSJ, Ho CS, Deshmukh R, et al. Infectious keratitis: An update on epidemiology, causative microorganisms, risk factors, and antimicrobial resistance. Eye. 2021;35(4):1084-1101.
- Ung L, Bispo PJM, Shanbhag SS, et al. The persistent dilemma of microbial keratitis: Global burden, diagnosis, and antimicrobial resistance. Surv Ophthalmol. 2019;64(3):255-271.
- Zhang Z, Cao K, Liu J, et al. Pathogens and antibiotic susceptibilities of global bacterial Keratitis: A Meta- Analysis. Antibiotics. 2022;11(2).
- Zemba M, Radu M, Istrate S, et al. Intrastromal injections in the management of infectious keratitis. Pharmaceutics. 2023;15(4):1-13.
- Agarwal R, Nagpal R, Todi V, Sharma N. Descemetocele. Surv Ophthalmol. 2020;66(1):2-19.
- Lin A, Rhee MK, Akpek EK, et al. Bacterial Keratitis Preferred Practice Pattern®. Ophthalmology. 2019;126(1):P1-P55.
- Khan IJ, Hamada S, Rauz S. Infectious crystalline keratopathy treated with intrastromal antibiotics. Cornea. 2010;29(10):1186-1188.
- Agahan A, Regalado R. Infectious crystalline keratopathy caused by diphtheroids treated with intrastromal antibiotics in a post-corneal transplant patient. Ophthalmol Res An Int J. 2016;5(2):1-5.
- Martinez-Velazquez L, Ma KK, Patel NS, Luo ZK. Successful management of infectious crystalline keratopathy with intrastromal antibiotic injections. Case Rep Ophthalmol Med. 2022;2022:1-6.
- Liang SYW, Lee GA. Intrastromal injection of antibiotic agent in the management of recalcitrant bacterial keratitis. J Cataract Refract Surg. 2011;37(5):960-962.
- Pak CM, Savage DE, Plotnik R, Wozniak RAF. Intrastromal antibiotic injection in polymicrobial keratitis: Case report and literature review. Case Rep Ophthalmol. 2022;13(2):550-555.
- McDonald MB. Research review and update: IQUIX (levofloxacin 1.5%). Int Ophthalmol Clin. 2006;46(4):47- 60.
- Zhou R, Wang Q, Yuan L, et al. Safety and efficacy of fortified antibiotics and fluoroquinolones for the treatment of bacterial keratitis: A meta-analysis. J Fr Ophtalmol. 2023;(xxxx):1-8.
- Skelnik DL, Clark LA, Bezwada P. Effect of drug concentration and exposure time of levofloxacin, ofloxacin, ciprofloxacin, gatifloxacin, and moxifloxacin on human corneal endothelial cells and keratocytes. Invest Ophthalmol Vis Sci. 2003;44(4739).
- Healy DP, Holland EJ, Nordlund ML, et al. Concentrations of levofloxacin, ofloxacin, and ciprofloxacin in human corneal stromal tissue and aqueous humor after topical administration. Cornea. 2004;23(3):255-263.
- Ucgul AY, Ucgul RK, Behcet M. Intrastromal administration of vancomycin to maximize its early effect on methicillin-resistant staphylococcus aureus keratitis: A rabbit study. Ocul Immunol Inflamm. 2021;30(6):1430-1435.
- Awwad ST, Haddad W, Wang MX, et al. Corneal intrastromal gatifloxacin crystal deposits after penetrating keratoplasty. Eye Contact Lens. 2004;30(3):169-172.
- Food and Drug Administration. IQUIX® (levofloxacin ophthalmic solution) 1.5%. February 2004:https://www.accessdata.fda.gov/drugsatfda_do cs/label/2004/21571_iquix_lbl.pdf (accessed October 12, 2023).

