Inflammatory pigment epithelial detachment associated with Blastocystis hominis
Ellen N. Yu-Keh, MD, Felipe I. Tolentino MD, Amadeo A.S. Veloso Jr., MD
INTESTINAL parasites are an uncommon cause of retinal disease. We report a case of inflammatory pigment
epithelial detachment (PED) presumed to be secondary to the amoeba Blastocystis hominis.
CASE REPORT
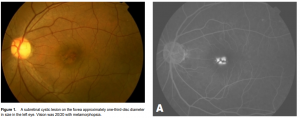
A 46-year-old Filipino male presented with visual distortion of the left eye for 7 months. Uncorrected
visual acuity was 20/20 but with metamorphopsia on amsler grid testing. Examination revealed the presence
of a subretinal cystic lesion on the fovea, approximately one-third-disc diameter in size (Figure 1). Optical
coherence tomography (OCT) showed PED with a hyperreflective lesion over the detached RPE (Figure 2A). The lesion demonstrated early hyperfluorescence with late staining on fluorescein angiography (FA)
(Figure 3A) and indocyanine green angiography (ICG) (Figure 3B). Work-up included a fecalysis which revealed the presence of Blastocystis hominis. The patient was treated with oral metronidazole 500 mg 3 times a day for 1 week. Fecalysis was normal after treatment. OCT performed 1 and 3 months after treatment remained unchanged. At 5 months, the PED resolved with return of the normal foveal contour by OCT (Figure 2B). Visual acuity was maintained at 20/20, and no recurrence was noted in 30 months follow-up.
DISCUSSION
B. hominis, currently classified as an amoeba, is transmitted by the fecal-oral route. Although its clinical
significance is controversial, it is generally believed to cause intestinal disease.1 Symptoms are nonspecific and include

diarrhea, nausea, abdominal pain and discomfort. Asymptomatic infections are not uncommon,2
with detection of B. hominis in the stool as an incidental finding as in this case. The average size of B. hominis is 4 to 15 mm in diameter2 and can only be seen under microscopy. Its common form is nonmotile, which may explain the absence of a destructive retinitis found when a motile parasite invades the retina such as in diffuse unilateral subacute neuroretinitis (DUSN). Instead, its presence in the RPE produces a local inflammatory response with subretinal-fluid accumulation and subsequent RPE detachment. OCT before treatment revealed an appearance characteristic of a PED with concave, dome-shaped, smooth elevation of the RPE with an optically quiet zone within.3 Common causes of PEDs include a coexisting choroidal neovascularization (CNV) and central serous chorioretinopathy (CSR). Further studies with FA and ICG ruled out the presence of CNV, which presents with late leakage of a hot spot. The typical “smokestack” or “inkblot” appearance noted on FA in eyes with CSR due to dye leakage under the detached neurosensory retina was also absent. The presence of a hyperreflective lesion over the detached RPE led us to suspect an infectious etiology for the PED, which was confirmed by fecalysis, and its resolution with oral antihelminthic therapy. In conclusion, intestinal parasitic infection may be associated with retinal disease, and should be included in the differential diagnosis of RPE detachment when OCT reveals a hyperreflective lesion.
References
1. Forbes B, Sahm D, Weissfeld A. Laboratory methods for diagnosis of parasitic infections. In: Bailey and Scott’s Diagnostic Microbiology 12th ed. Missouri: Mosby, 2007; 543-629.
2. Stenzel DJ, Boreham PF. Blastocystis hominis revisited. Clin Microbiol Rev 1996; 9: 563-584.
3. Mavrofrides EC, Villate N, Rosenfeld PJ, et al. Optical coherence tomography of ocular diseases. In: Schuman JS, Puliafito CA, Fujimoto JG, eds. Optical Coherence Tomography of Ocular Diseases. Thorofare, NJ: SLACK Inc., 2004; 243-343.

