Implementation and Pilot Data on Diabetic Retinopathy in a Teleophthalmology Program at a Multispecialty Primary Care Clinic
Joanne B. Tayapad, MD, Alfonso U. Bengzon, MD, Sherman O. Valero, MD, Milagros H. Arroyo, MD, Ricardo Tobias M. Papa, MD, Egidio Jose S. Fortuna, MD, Jocelyn G. Erni, BS, Myra Alisa J. Reyes, RN, Jerry D. Cavallerano, OD PhD, Lloyd Paul Aiello, MD PhD, Paolo S. Silva, MD
The International Diabetes Federation estimates that 382 million people or 8.3% of adults have diabetes worldwide.1 If trends continue, it is projected that by 2035, 592 million people, or 1 adult in 10, will have diabetes, equating to approximately 3 new cases every 10 seconds, or almost 10 million per year. The largest increases will take place in the regions of developing economies. In the Philippines, 3.3 million or 6.01% of adults (20 to 79 years old) have diabetes.1
Approximately one-third of people with diabetes develop diabetic retinal disease.2 Diabetic retinopathy (DR) is one of the leading causes of vision loss in working-age adults.1 As the global prevalence of diabetes increases, so will the numbers of people with diabetes-related complications.1
Detection and treatment of DR in its initial stages can prevent severe visual loss and eventual blindness in diabetic patients, as shown by the Diabetic Retinopathy Study and the Early Treatment Diabetic Retinopathy Study (ETDRS).2,3
Current recommendations for dilated retinal examination have been developed to identify early stages of DR prior to the development of visual complications, and to reduce the risk of visual loss. At the minimum, a dilated retinal examination is suggested annually for all patients with diabetes.4 However, the rates of adherence to regular eye examination in those with DR consistently fall below the recommended rate, and are as low as 17% in some studies.5 Data on rates of adherence to dilated retinal examination in Filipino diabetic patients are lacking.
Appropriately performed, standardized retinal imaging has been shown to compare favorably to a dilated retinal evaluation and standard ETDRS 7-field photography for determining DR severity.6 Ocular telemedicine programs for DR are an established method for population-based evaluation of DR.7,8 The utilization of teleophthalmology by obtaining standardized digital retinal images is an efficient and cost-effective method in the early diagnosis and treatment of retinal complications in diabetic patients.
This study determined the prevalence of diabetic retinal complications among Filipino patients in an urban primary care clinic using a validated teleophthalmology program.
METHODOLOGY
This was a retrospective, cross-sectional pilot survey of diabetic patients seen at a multispecialty primary care clinic (TMC-Fairview) from November 26, 2012 to August 31, 2013 and participated in the telemedicine program of The Medical City (TMC). Diabetic patients were referred for retinal imaging by primary health care physicians, internists, endocrinologists, and general ophthalmologists at the multispecialty clinic. Retinal imaging was obtained using the Visucam 200 Digital Fundus Camera (Carl Zeiss Meditec AG, Jena, Germany) and followed the validated program of the Joslin Vision Network nonmydriatic fundus photography for diabetic retinopathy evaluation. It was taken by a designated telemedicine nurse who had been trained and certified for retinal imaging. Stereoscopic pairs of three 450 fields and two 300 fields were acquired according to a prescribed protocol that has been previously validated to compare favorably with mydriatic ETDRS 7standard fields.6 Twenty-two images (11 for each eye) were obtained from each patient. Selective mydriasis, by instilling mydriatic eye drops (1.0% tropicamide) in eyes where poor image quality were obtained based on the decision of the imager, was employed to achieve a low rate of ungradable images. All patients with ungradable images due to media opacities (e.g., corneal scarring, cataracts, or vitreous hemorrhage) were referred to an ophthalmologist for a comprehensive eye evaluation.
All images were securely sent electronically to the Teleophthalmology Image Reading Center of The Medical City, through a virtual private network (FortiClient, Fortinet, Inc., Sunnyvale, CA, USA). All images were evaluated using dual monitor reading stations where retinal field images were displayed on 27-inch, color-calibrated, high definition, liquid crystal display monitors (model VG278H Asus, Taipei, Taiwan) with Quadro K600 video cards (Nvidia, Santa Clara, CA, USA), and a secondary 20-inch monitor to display patient records. Image archiving, management and retrieval were performed using the Forum Archive and Viewer (version 3.2, Carl Zeiss Meditec AG, Jena, Germany). All patient information was securely recorded in a customized, centralized, electronic patient records system that is compliant with international regulations.
Four retina specialists evaluated the retinal images using a standardized protocol for assessing diabetic retinal disease and the presence of other retinal findings. Continuous quality control and assurance was ensured by following a standard protocol to measure agreement between retinal specialists.
Retinal findings were recorded on customized electronic templates and retrieved using electronic search queries. A report containing the diagnostic comments, suggested treatment plans, additional diagnostic evaluation, follow-up recommendations, and referral for in-person consultation when necessary, was entered electronically.
RESULTS
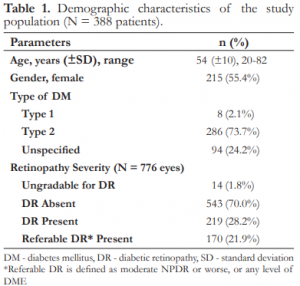
A total of 776 eyes of 388 diabetic patients was evaluated with the telemedicine program. The mean age was 54 years ± 10 (range 20 to 82), and 215 (55.4%) were females. Majority (91.5%) had type 2 diabetes based on either the patient’s report, physician diagnosis, or the use of oral hypoglycemic agents. The demographic characteristics of the population evaluated are presented in Table 1.

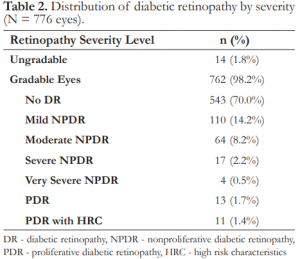
The prevalence of DR in this population was 28.22% (219 eyes), with 25.13% (195 eyes) having nonproliferative diabetic retinopathy (NPDR). 14.2% had mild, 8.2% moderate, 2.2% severe, and 0.5% very severe NPDR. 1.68% had proliferative DR (PDR) and 1.41% PDR with high-risk characteristics (Table 2).

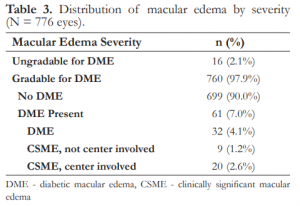
The prevalence of diabetic macular edema (DME) was 4.1% (32 eyes) and clinically significant macular edema (CSME) 3.74% (29 eyes), of which 68.97% (20 eyes) involved the center of the macula (Table 3). The rate of referable retinopathy (moderate NPDR or worse, any level of DME, or ungradable images) was 21.90% (170 eyes).

DISCUSSION
In the Philippines alone, over 9 million individuals will have diabetes by 2030.1 This prevalence roughly translates to a time investment of over 4.5 million hours per year by 1,200 ophthalmologist in the Philippines to conduct annual eye examination for each person. This clearly represents an insurmountable task. One of the benefits of using a teleophthalmology program, particularly in patients with no or mild DR, is the provision of alternative methods of eye care that can potentially reach a broader population.8
Overall, based on standardized retinal imaging, no referable DR was seen in 78% (n=606) of eyes. Patient education on the importance of retinal imaging or eye examination was conducted for all patients. Annual repeat retinal imaging was requested in the absence of referable DR or clinically evident nondiabetic retinal findings or optic nerve changes. In this group of patients, a significant benefit was realized by obviating the need for an in-person dilated retinal examination that would have otherwise overburdened the healthcare system, required a separate appointment for the patients, and contributed to increased healthcare cost.
In the primary care setting, teleophthalmology can effectively identify patients with diabetic retinal complications and potentially refer these patients to appropriate levels of eye care. Retinopathy was present in over 28% of patients evaluated. Over 21% of patients had referable disease that may potentially lead to visual complications if timely retinal evaluation is not performed. Teleophthalmology for DR in this setting allows early detection of potentially sight threatening disease and may prevent visual loss and complications.
REFERENCES
1. International Diabetes Federation. IDF Diabetes Atlas, 6th ed. Brussels, Belgium: International Diabetes Federation, 2013. Available at: www.idf.org/diabetesatlas.
2. Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology 1981;88:583-600.
3. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol 1985;103:1796-1806.
4. American Academy of Ophthalmology Retina Panel. Preferred P r a c tic e P a tt e r n ® G uid elin e s. Dia b e tic R e tin o p a t h y. San Francisco, CA: American Academy of Ophthalmology; 2008. (4th printing 2012). Available at: www.aao.org/ppp.
5. Adriono G, Wang D, Octavianus C, Congdon N. Use of eye care services among diabetic patients in urban Indonesia. Arch Ophthalmol 2011;129:930-935.
6. Silva PS, Walia S, Cavallerano JD, et al. Comparison of lowlight nonmydriatic digital imaging with 35-mm ETDRS sevenstandard field stereo color fundus photographs and clinical examination. Telemed J E Health 2012;18:492-499.
7. Gómez-Ulla F, Fernandez MI, Gonzalez F, et al. Digital retinal images and teleophthalmology for detecting and grading diabetic retinopathy. Diabetes Care 2002; 25:1384-9.
8. Cavallerano JD, Aiello LP, Cavallerano AA, et al. Nonmydriatic digital imaging alternative for annual retinal examination in persons with previously documented no or mild diabetic retinopathy. Am J Ophthalmol 2005;140:667-673

