Diabetic-Retinopathy progression following phacoemulsification, A metaanalysis
Paolo Antonio S. Silva, MD, Claudine Baduria Yap, MD, Felice Katrina Trio, MD, Romulo N. Aguilar, MD
THE GLOBAL prevalence of diabetes is increasing rapidly, estimated at 110 million in 1994 and projected to
reach 221 million by 2010.1 The risk of developing a visually significant cataract is significantly increased in
diabetic patients, in whom surgical management is disproportionately more problematic compared with
nondiabetic patients.2 Both the postoperative progression of diabetic retinopathy and macular edema are considered common causes of poor visual acuity in diabetic patients after uncomplicated cataract surgery,3, 4 and whether these represent the natural course of the disease or are direct effects of the surgery is still uncertain. Cataract surgery in diabetic patients has been marked with a high incidence of intraoperative and postoperative complications, which have been implicated in postoperative progression of diabetic retinopathy.5 Studies point to retinopathy severity and macular edema as the principal determinants of postoperative visual acuity, and link improved visual outcomes to the shift from conservative management to earlier surgical intervention.6 The degree of diabetic retinopathy has been correlated with visual outcome in a metaanalysis of extracapsular cataract extractions (ECCE) that analyzed proportions of eyes achieving 20/40 or better central acuity.7 Earlier cataract extraction in diabetic patients has been proposed to improve visualization and monitoring of the fundus, which would allow prompt treatment and increase longterm visual outcome.8 Postoperative progression has also been related to the presence and stage of retinopathy at
baseline. However, the postulated risk factors have not been consistent; the presence of background retinopathy has been implicated in some reports and active proliferative retinopathy in others. A more favorable visual outcome has been observed with preoperative treatment of retinopathy when indicated and the use of newer, smallincision cataract-surgery techniques such as phacoemulsification. An evidence-based approach to the practice of medicine is becoming more important in the face of increasing pressure on health-care professionals to deliver quality and cost-effective care. The decision to surgically remove cataracts in patients with diabetic retinopathy to improve visualization of the fundus and allow monitoring and treatment must outweigh the risk of possible progression of the retinopathy. The conflicting conclusions in studies investigating the progression of diabetic retinopathy after phacoemulsification prompt a systematic review of the best available evidence on the effect of phacoemulsification on the postoperative progression of diabetic retinopathy. This review was done to determine the effect of phacoemulsification on the progression of diabetic retinopathy.
METHODOLOGY
Criteria for inclusion of studies in this review
Types of studies. This review intended to include randomized controlled trials. However, none was found,
and the results of 5 prospective, case-controlled trials comparing the progression of diabetic retinopathy after
phacoemulsification versus no surgery were included.
Types of participants.
Study participants were patients diagnosed clinically with diabetes mellitus who have
undergone phacoemulsification in 1 eye and no surgery in the fellow eye.
Types of interventions.
Unilateral phacoemulsification and implantation of an intraocular lens compared with no surgery in the fellow eye among diabetic patients.
Types of outcome measures.
The primary outcome measure was the occurrence or progression of any type of diabetic retinopathy for at least 6 months following phacoemulsification.
Search strategy for identification of studies
Two independent searches of PubMed and Cochrane Central Register of Controlled Trials (CENTRAL) (which
contains the Cochrane Eyes and Vision Group trials register) on The Cochrane Library (Issue 1, 2005) were
conducted to identify all published articles on the progression of diabetic retinopathy following phacoemulsification. Clinical queries focusing on phacoemulsification, cataract surgery, and diabetic retinopathy were used to provide a broad search of all available clinical trials. There were no date or language restrictions in the electronic searches. Manual searches of the reference lists of included studies, other reviews, and book chapters on surgery for cataracts and diabetic retinopathy to find additional trials were conducted. Trial investigators and experts in the field were contacted to identify additional published and unpublished studies. Manual searches of journals or conference proceedings were not done.
Methods of the review
Selection of trials. Two reviewers independently assessed the titles and abstracts resulting from the electronic
searches. Full copies of potentially relevant reports were obtained. No studies fulfilled the criteria for randomized, controlled trials. We then proceeded to look for other types of studies pertinent to our search queries. Assessment of methodological quality. Assessment of methodological quality was based on the methods in section 6 of the Cochrane Reviewers’ Handbook. Four parameters were considered:
1. Allocation concealment and method of allocation to treatment
2. Masking of providers and recipients of care
3. Masking of outcome assessment
4. Completeness of follow-up. Each parameter was graded as follows: A = adequate,
B = unclear, or C = inadequate. Data extraction and synthesis. Data from studies were summarized collecting similar outcomes and using similar follow-up times after testing for heterogeneity between trial results using a standard chi-square test. For dichotomous data, results were expressed as odds-ratio estimates
(95% confidence interval). For continuous data, the mean and standard deviations were obtained. Standard errors were converted to standard deviations and summarized as weighted mean differences (95% confidence intervals).
Description of studies
The electronic searches identified 49 reports of studies on progression of diabetic retinopathy after cataract
surgery. There were no randomized controlled clinical trials assessing the progression of diabetic retinopathy after phacoemulsification. Five nonrandomized, prospective, case-controlled studies of similar study design were identified as follows:
• Krepler K, Biowski R, Schrey S, Jandrasits K, Wedrich A. Cataract surgery in patients with diabetic retinopathy:
visual outcome, progression of diabetic retinopathy, and incidence of diabetic macular oedema. Graefes Arch Clin Exp Ophthalmol 2002; 240: 735-738.
• Squirrell D, Bhola R, Bush J, Winder S, Tabot JF. A prospective, case-controlled study of the natural history of diabetic retinopathy and maculopathy after uncomplicated phacoemulsification cataract surgery in patients with type 2 diabetes. Br J Ophthalmol 2002; 86: 565-571.
• Flesner P, Sander B, Henning V, Parving HH, de la Cour MD, Lund-Andersen H. Cataract surgery on diabetic
patients. A prospective evaluation of risk factors and complications. Acta Ophthalmol Scand 2002: 80: 19-24.
• Kato S, Fukada Y, Hori S, et al. Influence of phacoemulsification and intraocular lens implantation on the course of diabetic retinopathy. J Cataract Refract Surg 1999; 25: 788-793.
• Wagner T, Knaflic D, Rauber M, Mester U. Influence of cataract surgery on the diabetic eye: a prospective study. Ger J Ophthalmol 1996; 5: 79–83.
Methodological quality
No assessment of quality was undertaken for the 5 prospective nonrandomized, case-controlled studies because they were different in study design from the criteria set in the Cochrane Reviewers’ Handbook. All 5 studies investigated the effect of the progression of diabetic retinopathy among patients undergoing monocular phacoemulsification using the fellow eye as control. The subjects were followed up for at least 6 months after the surger y. The characteristics of the 5 studies are summarized in Table 1.
RESULTS
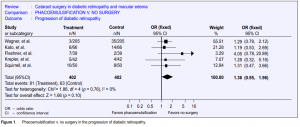
The data of the 5 case-controlled studies were pooled and analyzed based on a fixed-effect model as shown in
the Forest plot (Figure 1). Analysis was based on a total sample size of 804 eyes with the weight of each study on the overall effect as follows: Wagner et al. 55.51%, Kato et al. 21.28%, Flesner et al. 3.29%, Krepler et al. 7.07%, and Squirrell et al. 12.84%. Tests for heterogeneity (chi-quare)

showed homogenous results. The overall event rate showed that 81 of the 363 eyes that underwent phacoemulsification and 63 of the 363 control eyes had progression of diabetic retinopathy. The relative risk point estimate was 1.36, which was not statistically significant (95% confidence interval, 0.95–1.96).
DISCUSSION
There is a large body of literature on the progression of diabetic retinopathy after phacoemulsification, but it
consists mainly of retrospective studies, cohort studies, or case series. This review found no randomized, controlled trials on the subject. Five nonrandomized, prospective, case-controlled studies of similar study design were found dealing with the topic. The results of the 5 studies show that uncomplicated phacoemulsification and in-the-bag placement of an intraocular lens (IOL) did not result in increased progression and is, therefore, not contraindicated in patients with diabetic retinopathy. The observed progression after the surgical invasion is postulated to be a part of the natural course of the disease and not a result of the surgery. In all studies, improvement in visual acuity and the ability to better visualize the fundus to monitor and treat the retinopathy outweighed the risks of the surgical procedure and the possibility of later progression. There is growing evidence to support a more interventional approach to the management of cataract in patients with diabetes mellitus. This refinement in the approach to the timing of cataract surgery in diabetic patients seems to be the most important development in this field. However, it must be emphasized that the studies cited in this review are subject to methodological variation. The definition of retinopathy and determining its severity may vary due to inherent difficulties in grading retinopathy in eyes with cataract. The surgical techniques employed may vary among centers, likewise the indications for laser therapy. Grading the progression of retinopathy and follow-up monitoring can be different among the studies. Thus, the need is apparent for a well-designed, randomized, controlled clinical trial that will assess the progression of diabetic retinopathy after phacoemulsification. Implications on practice There are no randomized controlled trials to strongly support conclusions regarding the progression of diabetic retinopathy after phacoemulsification. The available studies reviewed have methodological flaws inherent in a nonrandomized or uncontrolled study design. Nonetheless, it seems that modern, uncomplicated, small-incision cataract surgery has minimal influence on the progression of diabetic retinopathy. Meticulous follow-ups are still needed for early detection and treatment of the retinopathy should it progress as a natural course of the disease in order to preserve the visual improvement gained from the cataract surgery.
Implications on research
Prospective randomized controlled trials should be conducted in eyes with nonproliferative and proliferative
diabetic retinopathy undergoing unilateral phacoemulsification to determine the risk factors for progression of the retinopathy. A well-designed study with adequate sample size, blinded outcome assessment, and long-term follow-up will surely provide statistically significant results to show whether phacoemulsification and any attendant complications are risk factors for progression of diabetic retinopathy.
References
1. Amos AF, McCarty DJ, Zimmet P: The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diab Med 1997; 14: S1- S85.
2. Klein BEK, Klein R, Moss SE. Incidence of cataract surgery in the Wisconsin epidemiologic study of diabetic retinopathy. Am J Ophthalmol 1995; 119: 295-300.
3. Benson WE, Brown GC, Tasman W, et al. Extracapsular cataract extraction with placement of a posterior-chamber lens in patients with diabetic retinopathy. Ophthalmology 1993; 100: 730-738.
4. Pollack A, Leiba H, Bukelman A, Oliver M. Cystoid macular oedema following cataract extraction in patients with diabetes. Br J Ophthalmol 1992; 76: 221-224.
5. Tsujikawa A, Otani A, Takanashi T, Ogura Y. Long-term prognosis of extracapsular cataract extraction and intraocular-lens implantation in diabetic patients. Jpn J Ophthalmol 1997; 41: 319-323.
6. Dowler JGF, Hykin PG. Cataract surgery in diabetes. Curr Opin Ophthalmol 2001; 12: 175-178.
7. Dowler JGF, Hykin PG, Lightman SL, Hamilton AMP: Visual acuity following extracapsular cataract extraction in diabetes: a metaanalysis. Eye 1995; 9: 313- 17.
8. Dowler JGF, Sehmi KS, Hykin PG, Hamilton AMP. The natural history of macular edema after cataract surgery in diabetes. Ophthalmology 1999; 106: 663-668.
9. Chung J, Kim MY, Kim HS, et al. Effect of cataract surgery on the progression of diabetic retinopathy. J Cataract Refract Surg 2002; 25: 626-630.
10. Kato S, Fukada Y, Hori S, et al. Influence of phacoemulsification and intraocular lens implantation on the course of diabetic retinopathy. J Cataract Refract Surg 1999; 25: 788-793.
11. Dowler JGF, Hykin PG, Hamilton AMP. Phacoemulsification versus extracapsular cataract extraction in patients with diabetes. Ophthalmology 2000; 107: 457-462.
12. Wagner T, Knaflic D, Rauber M, Mester U. Influence of cataract surgery on the diabetic eye: a prospective study. Ger J Ophthalmol 1996; 5: 79-83.

