A Case Report of a Transorbital Penetrating Intracranial Injury from a Motorcycle Side Mirror Metal Bar
Kia Charisse D. de Asis MD1, Mark Anthony T. Imperial MD DPBO1,2
1University of the East Ramon Magsaysay Memorial Medical Center, Quezon City
2Asian Hospital and Medical Center, Muntinlupa City
Correspondence: Kia Charisse D. de Asis, MD
Clinic Address: University of the East Ramon Magsaysay Memorial Medical Center
Clinic Phone Number: (02) 8715-0861
Email Address: kcdeasis@gmail.com
Disclosure: The authors have no financial disclosures or conflicts of interest to declare in relation to this case report.
Transorbital penetrating intracranial injuries caused by foreign bodies are extremely uncommon, accounting for 0.04% of all cases of penetrating head trauma. However, they are associated with high mortality rate.1 In cases of transorbital penetrating intracranial injuries, it is crucial to establish an appropriate surgical plan requiring a multidisciplinary approach from neurosurgeons, ophthalmologists, and otolaryngologists.2 The choice of surgical technique for removing foreign bodies depends on the nature of foreign body, its location, and associated complications. This can either be through a transorbital or transcranial approach.1,3 In this report, we present a case of transorbital penetrating intracranial injury that was successfully managed using a stepwise multispecialty approach, resulting in good visual outcome.
CASE REPORT
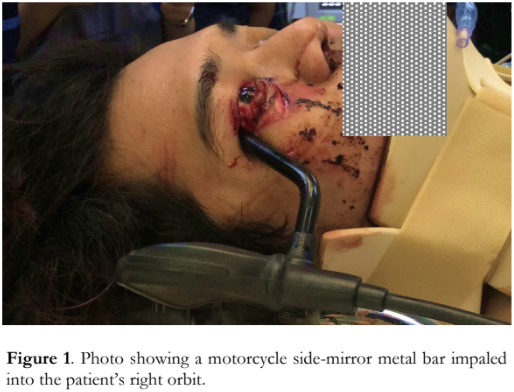
A 26-year-old Filipino male presented to the emergency room after sustaining a transorbital penetrating intracranial injury after being struck by an oncoming motorcycle. Past medical history of the patient was unremarkable. On physical examination, he had a Glasgow Coma Scale score of 12 (E4V3M5) and his vital signs were stable. The motorcycle side-mirror metal bar was impaled into his right orbit at the lateral canthus (Figure 1). Ophthalmic examination revealed upper eyelid avulsion, detachment of the lower eyelid from the lateral canthus, and upper and lower canalicular system transection. The pupil of the right eye was round, dilated and non-reactive to light. The visual acuity could not be properly assessed due to poor verbal response of the patient. The examination of the left eye revealed no abnormalities.
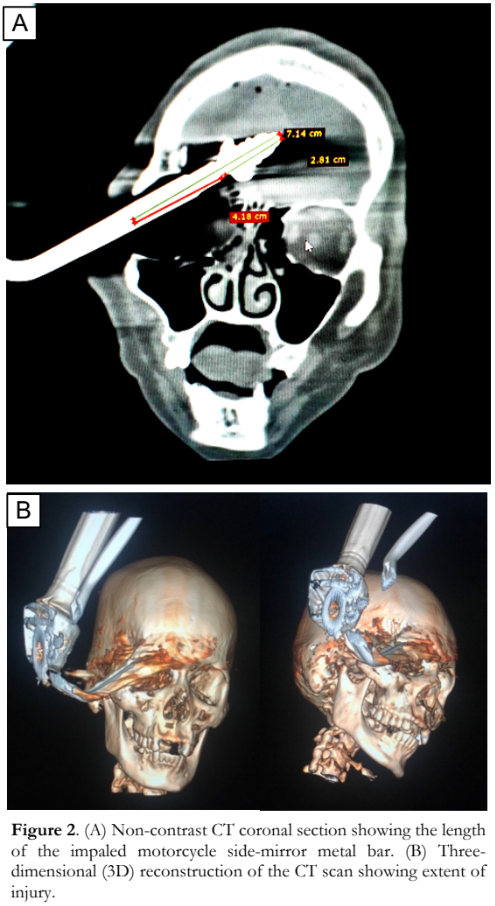
Plain computed tomography (CT) scan demonstrated the motorcycle side-mirror metal bar traversing the right orbit and extending into the right frontal lobe substance with its tip within the anterior cranial fossa (Figure 2). The penetrating segment of the metal spanned 7.14 centimeters (cm), while its distal 2.81 cm exhibited a distinctive bulbous threaded configuration, puncturing the right frontal lobe. There was an ill-defined appearance of the right globe suggestive of rupture. Multiple fractures were seen in the posterior wall of the right frontal sinus and right lamina papyracea, and there were comminuted fractures involving the right orbital roof and floor. There were no other fractures or dislocation in the calvarium and basal skull structures. There were also hyperdense foci in the bilateral frontal lobe parenchyma, bilateral fronto-parietal cortical sulci as well as along the interhemispheric fissure consistent with contusion hemorrhages of bilateral frontal lobes and subdural hemorrhages in the interhemispheric fissures. Air pockets were seen along the bilateral frontal convexities and anterior interhemispheric fissure. There was no brain edema nor hemorrhage. The patient was started on intravenous broad-spectrum antibiotics for pre-operative prophylaxis.
A coordinated multidisciplinary surgical intervention by the neurosurgical, orbit and oculoplastic teams was immediately carried out. On examination under general anesthesia, the following injuries were noted: right upper eyelid medial canthal transection with canalicular involvement, upper eyelid lateral canthal transection, lower eyelid medial canthal transection with canalicular involvement, and lower eyelid lateral canthal transection and full-thickness margin laceration. The motorcycle side-mirror metal bar was found firmly lodged in the orbital area (Figure 3). A transorbital approach was employed to extract the motorcycle side-mirror metal bar. The foreign object was maneuvered and removed, following the trajectory of its penetration from the inlet in the lateral canthus. Continued pull on the handlebar resulted in bradycardia from oculocardiac reflex prompting the surgeons to stop briefly. When the side-mirror metal bar was extracted, there was a rush of blood and tissue fragments. The right globe was found intact. Repair of multiple eyelid lacerations and canthoplasty were then done. Repair of the canalicular transection was deferred to give way for neorosurgical intervention.
Pterional craniotomy, contusectomy, debridement and duraplasty were done to address the subarachnoid hemorrhage in the bilateral fronto- parietal cortical foci and contusion hemorrhages of bilateral frontal lobes.
On the first post-operative day, visual acuity of the right eye was counting fingers at 2 feet. The patient had complete ptosis, a 5-mm fixed pupil, and complete ophthalmoplegia of the right eye. Anterior and posterior segments were normal. The left eye was unremarkable.
Four months after the surgery, visual acuity of the right eye improved to 20/50 while ocular motility showed very minimal improvement on left gaze (Figure 4). The right upper eyelid remained ptotic and the right pupil was still 5 mm dilated, without relative afferent pupillary defect (RAPD) noted. The rest of the eye findings remained unchanged.


DISCUSSION
To our knowledge, this is the first documented case in the Philippines of a transorbital penetrating intracranial injury by a large foreign body that was successfully extracted without resulting in mortality or blindness.
Transorbital penetrating intracranial injuries from foreign bodies account for 4.5% of all cases of orbital pathology and comprise 24% of penetrating head trauma incidents in adults.1 The occurrence of a large metallic foreign body deeply penetrating the orbit, such as in this case report, is uncommon.3
Resembling a horizontal pyramid with a postero-medial axis, the orbit tends to deflect objects towards its apex, potentially leading them intracranially through passages like the superior orbital fissure or the optic canal. Transorbital penetrating injuries can follow the course of the superior orbital fissure towards the cavernous sinus to reach the brainstem, or through the optic canal to the optic nerve and internal carotid artery.4 Penetration of the orbital roof is not uncommon due to the fragility of the frontal bone, and often results in frontal lobe contusion.4 Mismanagement of these fractures can have devastating consequences due to the proximity of the frontal bone to intracranial structures.5
Complications of transorbital penetrating intracranial injuries depend on the path taken by the penetrating object upon exiting the orbit, and these may include intracerebral hematoma, cerebral contusion, intraventricular hemorrhage, pneumocephalus, cranial nerve damage, permanent neurological impairment, brain stem injury, and cerebrovascular injury.4
Depending on the location of the intraorbital foreign body, a transorbital or transcranial approach on its removal can be selected.4 There is no standardized management algorithm for transorbital penetrating intracranial injuries. Assessment, surgical intervention, and post-operative care should be individualized. A comprehensive clinical history and thorough eye examination are essential to identify the foreign body’s location, size, type, and extent of injuries. Stabilization precedes assessment and subsequent removal of the foreign body. Removal of foreign body should be deferred until after full physical examination and radiological evaluation have been done because its premature removal outside the controlled environment of the operating room may lead to fatal hemorrhage.2 Imaging studies are done to identify the foreign body’s size, location, and trajectory as well as the extent of bone and soft tissue injuries. This medical information is crucial in formulating an appropriate surgical plan. Non-contrast CT scan is the recommended primary imaging modality for transorbital penetrating intracranial injury as it can help determine the trajectory of the penetrating object, assess the extent of bone and tissue damage, and evaluate globe integrity.1,4,5,6 In cases involving organic, non-metallic, foreign bodies, MRI is the preferred initial imaging method as it provides enhanced visualization of soft tissues.3
Optimal surgical approach is determined in collaboration with neurosurgeons, otolaryngologists, and maxillofacial surgery specialists. The choice of surgical approach for removal depends on the nature and location of the foreign body within the orbit (anterior or posterior), associated complications such as infections, optic nerve injury, potential damage to ocular motor nerves or intraorbital blood vessels, and patient’s overall health status.3,
Minor asymptomatic foreign bodies are conservatively managed with close monitoring and regular follow-ups. In contrast, large foreign bodies, as in our case, causing significant complications require surgical intervention.3 The optimal treatment timeframe for intraorbital metallic foreign bodies varies. However, generally, early intervention within the initial 24 to 48 hours is advised to reduce complications and enhance the likelihood of successful removal.3 Removal of intraorbital foreign bodies can be done via transorbital or transcranial approach. In our case, a transcranial approach was deemed inappropriate due to the complex and time-consuming procedure of initially severing the solid metal bar of the side- mirror, which remained connected to the motorcycle handlebar. The decision was to mitigate the potential risk of causing further tissue damage.
Since extraction of a large intraorbital foreign body can cause anterior displacement of the right globe and traction on the extraocular muscles, it is crucial to monitor for oculocardiac reflex (OCR). Bradycardia is the most common response to OCR but other outcomes include potentially fatal arrhythmias, asystole, and cardiac arrest. Immediate discontinuation of the triggering stimulus to relieve pressure from the eye and surrounding orbital tissues is recommended.8
The complete right upper eyelid ptosis, diminished visual acuity, fixed-dilated pupil, and total ophthalmoplegia on postoperative day 1 may be attributed to the substantial damage to structures within the lateral orbital wall such as the check ligament of the lateral rectus muscle, the lateral horn of the levator aponeurosis, palpebral ligament, and ciliary ganglion which is situated between the lateral rectus muscle and optic nerve. The patient was followed up for potential complications associated with repairing penetrating orbital injuries, such as CSF leak, meningitis, cerebral abscess, carotid cavernous fistula, traumatic aneurysm, and intravascular thrombosis. All were absent in our case.
In conclusion, transorbital penetrating intracranial injuries are rare and result in vision- and life-threatening complications. A transorbital approach in removing a penetrating foreign body was used since injury to cerebral tissues was imminent. Individualizing the management and employing a multispecialty approach can lead to favorable outcomes.
REFERENCES
- Arslan M, Eseoğlu M, Güdü BO, Demir I. Transorbital orbitocranial penetrating injury caused by a metal bar. J Neurosci Rural Pract. 2012;3(2):178-181.
- Schreckinger M, Orringer D, Thompson BG, La Marca F, Sagher O. Transorbital penetrating injury: case series, review of the literature, and proposed management algorithm. J Neurosurg. 2011;114(1):53-61.
- Elseyoufi M, Abdel-Ghany H. Penetrating orbital trauma by a large metallic foreign body: A case report. Oral and Maxillofacial Surgery Cases. 2023;9(2):100307.
- Shin TH, Kim JH, Kwak KW, Kim SH. Transorbital penetrating intracranial injury by a chopstick. J Korean Neurosurg Soc. 2012;52(4):414-416.
- Jeyaraj P. Frontal Bone Fractures and Frontal Sinus Injuries: Treatment Paradigms. Ann Maxillofac Surg. 2019;9(2):261-282.
- Leal I, Caldeira I, Sousa R, Pinto F. Exceptional penetrating orbital injury that spared the eye globe. BMJ Case Rep. 2015;2015:bcr2014209053.
- Jabang JN, Dampha L, Sanyang B, et al. Management of a large intraorbital wooden foreign body: Case report. Surg Neurol Int. 2020;11:158.
- Dunville LM, Sood G, Kramer J. Oculocardiac Reflex. [Updated 2022 Sep 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan- . Available from: https://www.ncbi.nlm.nih.gov/books/NBK499832/

