Treatment of juxtapapillary toxoplasmic retinochoroiditiswith intravitreal clindamycin and dexamethasone injection
Edmin Michael G. Santos, MD
TOXOPLASMOSIS is the most common identifiable cause of posterior uveitis in immunocompetent patients.
Young children may present with reduced visual acuity, strabismus, leukocoria, and nystagmus while older individuals complain of decreased vision, floaters, photophobia, pain, and hyperemia.
CASE REPORT
We report a case of a 34-year-old woman who presented with sudden onset of decreased vision in the left eye associated with floaters. There was no underlying systemic disease or recent health change and no family history of unusual eye disease. She recalled experiencing floaters, which resolved spontaneously. On examination, visual acuity was 20/20 in the right eye (OD) and 20/50 in the left (OS).
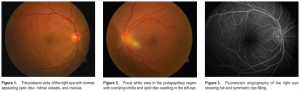
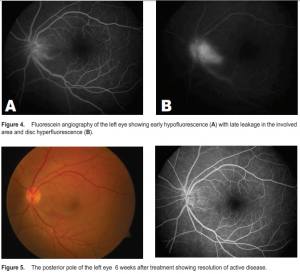
Intraocular pressure (IOP) was 14 mm Hg in both eyes. The anterior chamber was formed and clear with clear lens and cornea for both eyes. There was a clear view of the posterior pole in OD with normal-appearing optic disc, retinal vessels, and macula (Figure 1). The vitreous in OS had 1+ anterior vitreal cells (more cells in the posterior vitreous) and macular edema. There was a focal white area in the juxtapapillary region with overlying vitritis and optic-disc swelling (Figure 2). Fluorescein angiography showed full and symmetric dye filling with normal optic-disc fluorescence in OD (Figure 3). OS showed early hypofluorescence with late leakage in the involved area and disc hyperfluorescence (Figure 4). VDRL and ANA testing showed negative results. Complete blood count was within normal limits. Toxoplasma IgG testing was reactive and IgM levels were within normal limits. The toxoplasma IgG results, combined with the patient’s history of having pet cats at home, led to a diagnosis of ocular toxoplasmosis. Treatment was immediately initiated, consisting of twice-daily oral regimen of trimethoprim/sulfamethoxazole 160/800 mg and once-daily 50 mg of prednisone. The patient, however, returned the following day with worsening vision. The decision was made to immediately give an intravitreal injection of clindamycin 1 mg in 0.1 mL and dexamethasone 4 mg in 0.1 mL The oral antibiotic regimen was continued for 6 weeks and the steroid for 2 weeks. The patient’s condition improved in the following days with vision returning to 20/20. Photographs taken after the sixth week of treatment showed the resolution of active disease (Figure 5). Eye examination at this time revealed no active inflammation and the patient was taken off all oral medications.
DISCUSSION
Toxoplasmic retinochoroiditis typically affects the posterior pole with either solitary or multiple lesions. Active lesions are gray to white foci of retinal necrosis with adjacent choroiditis, vasculitis, hemorrhage, and vitritis. Lesions close to or on the optic nerve can also lead to optic neuropathy. Other atypical presentations include punctate outer retinitis, neuroretinitis, pseudo-multiple retinochoroiditis, intraocular inflammation without retinochoroiditis, unilateral pigmentary retinopathy, Fuchs’-like anterior uveitis, scleritis, and multifocal or diffuse necrotizing retinitis. The initial decision on whether to treat a toxoplasmainduced retinal lesion would generally be made if it is within the temporal arcade, abutting the optic nerve or threatening a large retinal vessel, when the lesion has induced a large degree of hemorrhage, or if there is a substantial two-line drop from the visual acuity before the acute infection. The lesion in the case presented was located in the juxtapapillary area causing optic neuropathy as well as substantial vitritis; thus, the need for immediate treatment. Ocular toxoplasmosis has classically been treated with a combination of pyrimethamine, sulfadiazine, and prednisone; sometimes clindamycin is added (quadruple therapy). However, there have been very few randomized trials, and there is, in fact, no consensus regarding the best treatment regimen. Furthermore, concerns have been raised on the safety profile of the classic triple and quadruple therapy.
In this case, the initial treatment was oral trimethoprim/ sulfamethoxazole 160/800 mg twice a day combined with oral prednisone 50 mg per day, following the protocol described by Soheilan and colleagues in their study, which found no significant difference in response rates between the 2 treatment groups.
With the patient’s vision rapidly worsening despite oral antimicrobial therapy and the juxtapapillary location of the lesion threatening the optic nerve, the decision was made to immediately administer intravitreal clindamycin and dexamethasone while continuing the oral antibiotic and steroid regimen. The patient’s condition subsequently improved dramatically, with vision returning to 20/20 over the next few days. Kishore and associates reported success in treating 4 patients with clindamycin 1.0 mg in 0.1 mL but with a lower dose of dexamethasone at 1.0 mg in 0.1 mL in their case series.
This is the first reported use of intravitreal clindamycin 1.0 mg in 0.1 mL and dexamethasone at a higher dose of 4.0 mg in 0.1 mL, resulting in the resolution of the optic neuropathy and the retinochoroiditis. In summary, intravitreal injection of clindamycin 1.0 mg/0.1 mL and dexamethasone 4.0 mg/0.1 mL was shown to be effective in treating toxoplasmic retinochoroiditis which progressed despite systemic therapy. It may also be offered to patients who cannot afford or tolerate systemic therapy.
1. Hol land GN, Lewis KG, O’Connor GR. Ocular toxoplasmosis: A 50th anniversary tribute to the
contributions of Helenor Campbell Wilder Foerster. Arch Ophthalmol 2002; 120: 1081-1084.

