Demodex sp. infestation in anterior blepharitis, meibomian-gland dysfunction, and mixed blepharitis
Angelito Braulio Flores de Venecia III, MD, Ruben Lim Bon Siong, MD
BELONGING to Phylum Arthropoda, Class Arachnida, Order Acarina, Demodex mite is an external parasite that can infest the meibomian and sebaceous glands. Although they normally inhabit the hair and eyelash follicles in low numbers, their over proliferation may lead to lid-margin infection causing ocular-surface irritation and symptoms of ocular discomfort like itching, foreign-body or stinging sensation. It may also exacerbate coexisting lid-margin diseases like anterior blepharitis (staphylococcal and sebaceous) and posterior blepharitis (meibomian-gland dysfunction). Demodex infestation is an often-overlooked differential diagnosis in the clinical investigation of blepharitis and may be a cause of treatment failure when not specifically addressed. The exact relationship of Demodex and blepharitis, however, is yet to be fully explained. The adult Demodex is cigar-shaped, with several pairs of legs, and has a mouth with a biting apparatus. It measures about 280 to 440 microns. Two distinct species have been found on human skin: Demodex folliculorum and Demodex brevis.1 Diagnosis of Demodex infestation is made by identification of the parasite at the root of the lashes using light microscopy. Alejo and Valenton described Demodex folliculorum in the lids of 50% of randomly chosen Filipino patients at the Philippine General Hospital.2 Patients diagnosed with blepharitis had Demodex in 88% of cases. The authors, however, did not classify blepharitis according to anatomic involvement or specific diagnosis of blepharitis, and did not associate age, sex, ocular symptomatology and clinical findings with the incidence and severity of Demodex infestation. Such correlation will be useful to the clinician in the diagnosis and treatment of blepharitis in general and Demodex-related blepharitis in particular. This study determined the incidence and density of Demodex species found on the eyelashes of subjects with normal eyelids, anterior blepharitis, meibomian gland dysfunction, and mixed blepharitis. Specifically, it determined the relationship of the incidence and density of Demodex with age and sex, ocular symptoms related to blepharitis, and clinical lid-margin findings (dandrufflike material, collarette or cylindrical dandruff, scurf, plugged meibomian gland orifices, crust).
METHODOLOGY
Consecutive patients who consulted at the General Clinic and the External Disease Clinic of a tertiary public hospital over a period of 3 months with the diagnosis of meibomian-gland dysfunction (MGD), anterior blepharitis (AB), or mixed blepharitis (MB) were recruited into the study. One of the authors (ABDV) established the diagnosis based on preset criteria of clinical findings (Table 1) using a single slit lamp biomicroscope (Topcon Slitlamp SLD7, Japan).
The diagnosis was confirmed by one of the consultants of the External Disease Clinic (RLBS included) using the same slitlamp biomicroscope. Patients who were on topical ophthalmic medications over the past 3 months, except for artificial tears; with history of ocular or eyelid trauma and surgery; with previous diagnosis of chemical burns; Steven-Johnson syndrome, ocular cicatricial pemphigoid, and other similar conditions; with eyelid malpositions like entropion, ectropion, and dystrichiasis; or with signs of active ocular infection or inflammation other than blepharitis were excluded from the study. After the recruitment period for MGD, AB, and MB, 50 age-matched patients who consulted at the General Clinic for other eye complaints were recruited to serve as controls (normal).
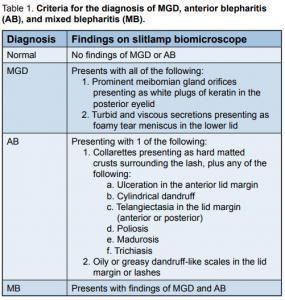
Table 1. Criteria for the diagnosis of MGD, anterior blepharitis (AB), and mixed blepharitis (MB). All patients underwent standard eye examinations. Data gathered included demographics, ocular symptomatology, and clinical findings. Digital photographs of the lid margins were taken using the digital camera of the same slitlamp biomicroscope. Lash sampling was done using the Modified Coston Method for epilating lashes.6-7 The collected lashes were checked for Demodex based on morphology (Figure 1) using a light microscope (Nikon YS100) and the total number of Demodex identified were tabulated for each eye. Patients in groups AB and MB underwent eyelid culture using a standard procedure. Each eye was swabbed with a sterile cotton tip applicator on the upper and lower lid margins. Blood agar was used as the culture medium. The cotton-tip applicators
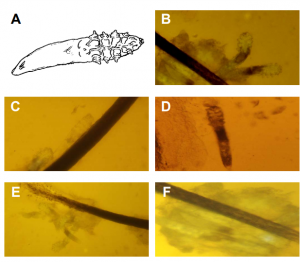
were applied to the blood agar plates. Specimen from the right eye Figure 1. Appearance of Demodex folliculorum under the light microscope. The diagnosis of Demodex infestation is made by identification of the parasite under light microscopy. Diagram of a typical parasite that is cigar-shaped and has 4 pairs of short legs on the right half and a mouth with a biting apparatus on the extreme right (A). The parasite frequently appears in pairs and has an obvious head-neck part and body-tail part (B). The parasite is covered by a cuticle surface, and the body is mostly semi-transparent (C). The body-tail part may show numerous striations, while the head-neck part contain 4 pairs of short legs (D). Demodex follicullorum in clusters in a single hair follicle (E). Demodex embedded in dandruff-like debris (F). was applied in the form of “R” and that of the left eye in the form of “L”. Each plate was labeled with the patient’s name and date of collection and sent to the Microbiology Department of UP-PGH for incubation and identification. All patients were referred back to either the General Clinic or the External Disease Clinic for further treatment and follow-up. The main outcome measures were:
1. Incidence of Demodex infestation, taken as the percentage of patients per group (Normal, MGD, AB, MB) that had lashes with mites identified using the light microscope, and
2. Mean Demodex count (MDC), taken as total number of mites counted from both right and left eyes of all patients of each group divided by the total number of patients per group. Data were tabulated using Microsoft Excel ver. 2008 (Microsoft Corporation, Redmond, WA, USA). They were subjected to statistical analyses using one-way analysis of variance, Dunnett’s method of comparison (comparison with a control, p < 0.01), Tukey-Kramer HSD method, chi-square analysis, and t-test. The study was reviewed and approved by the Ethics Review Board of the University of the Philippines-Philippine General Hospital. Informed consent was obtained from all participants.
RESULTS
A total of 167 participants (334 eyes) were included, 22% males and 78% females with a mean age of 53.7 years (range, 20 to 85). Of the total, 50 (30%, 100 eyes) were normal; 65 (40%, 130 eyes) had MGD; 20 (12%, 40 eyes) had anterior blepharitis; and 32 (19%, 64 eyes) had mixed blepharitis. Incidence of Demodex infestation
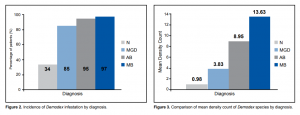
A total of 122 participants (73%) had Demodex infestation. The incidence of Demodex infestation was as follows: 34% (17/50) in normal participants, 85% (55/65) in MGD patients, 95% (19/20) in AB patients, and 97% (31/32) in MB patients (Figure 2). Using one-way ANOVA, there was a significant difference in the number of patients with Demodex infestation in MGD, AB, and MB compared to the normal group (p < 0.01). There was a strong association between anterior and posterior blepharitis and Demodex infestation. The incidence was highest when both anterior and posterior blepharitis were present (MB), followed by posterior blepharitis (PB) and anterior blepharitis (AB). Mean Demodex Count (MDC)
Patients with MB had the highest density of Demodex infestation, with MDC of 13.63 (range, 0 to 27), followed by AB with MDC of 8.95 (range, 0 to 22), and by MGD with MDC of 3.83 (range, 0 to 11). The normal group had the least density with MDC of 0.98 (range, 0 to 5) (Figure 3). The MDCs of MGD, AB, and MB were significantly different from the MDC of the normal group using the Dunnett’s method of comparison (p < 0.01). The MDCs of MGD, AB, and MB were also statistically different from each other. The degree of blepharitis was directly proportional to the density count of Demodex. Mixed blepharitis with involvement of both anterior and posterior lid margins had the highest density counts. Comparing the incidence and MDC per diagnosis, it also showed a directly proportional relationship.
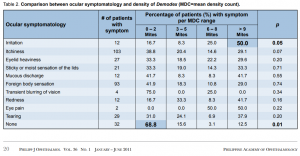
Figure 2. Incidence of Demodex infestation by diagnosis.
Relationship with Age
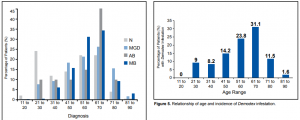
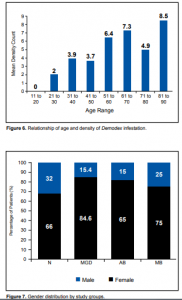
Majority of patients were between 41 and 70 years old (Figure 4). 58% of normal, 66% with MGD, 70% with AB, and 82% with MB were within this age range. The highest incidence of Demodex infestation was seen in the 61 to 70 age group (31%), followed by the 51 to 60 age group (24%) (Figure 5). One-way ANOVA test, however, showed no significant difference in the incidence of Demodex infestation among the different age groups. There was, likewise, a trend towards increasing density of Demodex (MDC) with increasing age (Figure 6). Using the Tukey-Kramer HSD Method, however, there was also no significant difference in density of Demodex among age groups.
Figure 3. Comparison of mean density count of Demodex species by diagnosis.
Figure 4. Age distribution of patients by diagnosis.
Figure 5. Relationship of age and incidence of Demodex infestation.
Figure 6. Relationship of age and density of Demodex infestation.
Figure 7. Gender distribution by study groups.
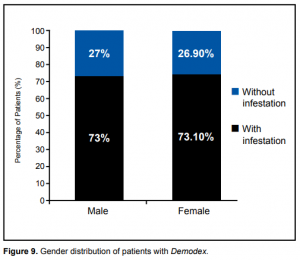
Figure 8. Gender distribution of patients with Demodex.
These results showed possible direct relationship between age and incidence of Demodex infestation and between age and density of Demodex. Relationship with sex
In all 4 groups, there were more female than male patients. The male: female ratio was 1:2 for normal, 1:5 for MGD, 1:5 for AB, and 1:3 for MB (Figure 7). The incidence of Demodex infestation was expectedly higher in females. However, taken as a percentage of patients of the same sex, there were 27 out of the total 37 males (73%) in the study found to be positive for Demodex. In females, 95 out of the 130 females (73.10%) were found to be positive for Demodex (Figure 8). Result of the one-way ANOVA test showed that the difference in the incidence of Demodex infestation between genders was not statistically significant. Similarly, one-way ANOVA test comparing MDC in males (5.65) and MDC in females (5.33) showed no significant difference. These results showed that males and females, regardless of type of blepharitis, were equally at risk for Demodex infestation. Relationship with ocular symptomatology
The most common eye symptoms were itchiness and foreign-body sensation (Table 2). These and other symptoms were nonspecific, appearing in all study groups. Ocular symptomatology was compared with density of Demodex infestation (MDC) divided into four density ranges based on the data from Figure 3 (Table 2). Chisquare analysis was used to test if there was a difference in frequency of occurrence of symptom between the MDC ranges. Analysis showed that 50% of the patients with irritation had a MDC >9 mites (p = 0.05) and that 68.8% of patients with no symptoms had a MDC of 0 to 2 mites (p = 0.01). Other symptoms were similar in terms of their distribution in each of the MDC subgroups. The results showed that:
1. Severe Demodex infestation, defined as presence of more than 9 mites, will probably result in lid irritation. Presence of Demodex usually did not present with any specific symptoms unless infestation was severe.
2. Individuals who were asymptomatic had no or very mild Demodex infestation.
3. Symptoms in Demodex-related blepharitis was not reflective of the severity of Demodex infestation. Relationship with clinical findings on slitlamp examination
Among the 3 groups of patients with diagnosis of blepharitis or MGD, the top 3 slitlamp lid-margin findings were collarettes/cylindrical dandruff, plugged meibomian gland orifices, and dandruff-like or scale-like materials. Clinical findings of collarettes/cylindrical dandruff had the highest association with the severity of the MDC, followed by plugged meibomian gland orifices (also seen in low MDC), while dandruff-like material was not associated with the severity of the density count (Table 3). Chi-square analysis showed that 68% of the patients with collarettes/cylindrical dandruff (p < 0.001) and 36.1% of plugged meibomian glands had a MDC > 9 mites (p < 0.001), and that 82.7% of patients with no clinical findings had a MDC of 0 – 2 mites (p < 0.001). Other clinical findings were similar in terms of their distribution in each of the MDC subgroups.
These results showed that:
1. Patients with clinical findings of collarettes/cylindrical dandruff or plugged meibomian gland orifices will probably have severe Demodex infestation.
2. Individuals with no clinical findings will have no or very mild Demodex infestation.
3. Clinical findings of dandruff-like materials are not reflective of the severity of Demodex infestation.
Culture Studies
Over 90% of cases in the AB and MB groups were positive for Staphylococcus aureus and epidermidis (Table 4). These findings supported the clinical diagnoses of anterior and mixed blepharitis among these patients.
DISCUSSION
The general incidence rate of Demodex infestation in this study was 73%, significantly higher than the 50% in the study by Alejo and Valenton.2 This could be partly due to the bigger sample size and the larger number of patients with anterior and posterior blepharitis included in the sampling. Among normal patients, the incidence was lower at 34%. In patients diagnosed with blepharitis, Alejo and Valenton found Demodex in 88% of cases, which is consistent with our study (85 to 97%). Their study, however, neither classified blepharitis according to anatomic involvement nor determined the density of the Demodex. This study demonstrated the highest incidence and density in patients with mixed blepharitis, followed by anterior blepharitis. MGD patients have the lowest incidence and density among the three. This can be explained by the fact that patients with mixed and anterior blepharitis have involvement of the eyelashes because Demodex mites tend to be clustered to the roots of lashes.
Table 2. Comparison between ocular symptomatology and density of Demodex (MDC=mean density count). Demodex infestation in humans was once thought to be of no clinical significance due to its nonpathogenic nature. Several authors, however, have concluded that Demodex infestation or demodecosis is related to blepharitis.3,8-11 But the exact pathogenic potential of Demodex mites remains unclear because a low number of Demodex can be found in the skin and lashes of asymptomatic individuals. It is thought that Demodex becomes pathogenic when it multiplies to cause or exacerbate ocular symptoms and lid-margin changes. No prior research has convincingly demonstrated whether a minimal number of mites must be present to produce symptoms. Of the ocular symptoms investigated, only lid irritation correlated with a high Demodex count. The etiology of lid irritation in Demodex infestation is an interplay of different factors. First, the biting apparatus of the parasite alone may cause lid irritation. Second, lid irritation is also caused by the lipolytic enzymes produced by the parasite to digest sebum, and by the accumulation of parasite excreta, resulting in the blockage of sebaceous glands that may lead to infection or the stimulation of the host’s humoral responses and cell-mediated reaction. Third, secondary or concomitant microbial blepharitis is common in Demodex infestation, as the microorganisms may cling to the integuments of the parasites.4 The incidence and density of Demodex infestation tend to steadily increase with the individual’s age. This is consistent with the increasing incidence of mixed blepharitis and MGD in the older age groups. Similar to the results of our study, Özlem et al. reported no significant difference between mite positivity and negativity between genders.5 Gao, et al. noted that Demodex infestation was more prevalent in patients with clinically evident cylindrical dandruff, which was seen in anterior blepharitis.1 The severity of Demodex infestation correlated well with the clinical finding of cylindrical dandruff. The Demodex count was higher in lashes with cylindrical dandruff compared to those without. English proposed that instead of just randomly choosing non-adjacent lashes, as done in the conventional Coston Method, lashes with dandruff-like material should be picked over those without.6 This modification in the Coston Method was applied in this study. The conventional Coston method of determining Demodex infestation carried certain errors of under detection: (1) Random epilation of lashes may result in a lower count if lashes without cylindrical dandruff were epilated; (2) Demodex mites were more adherent to cylindrical dandruff and the non-adherent mites in lashes without cylindrical dandruff may get dislodge during mounting, resulting in undercounting. The conventional Coston method of Demodex collection proposed in 1967 also advocated the use of peanut oil in mounting the specimen prior to microscopic evaluation and counting.3 Placing oil did not promote instant breakdown of debris and cuffs, resulting in undercounting of embedded mites. The use of fluorescein in our study improved the microscopic visibility and counting of Demodex by dissolution and expansion of cuffs. The yellowish contrast provided by the fluorescein also helped detect Demodex embedded in compact and opaque cuffs of epilated lashes, resulting in a more accurate Demodex count.7
Table 3. Comparison between clinical findings and density of Demodex. *MDC = mean density count
Table 4. Culture results of anterior blepharitis (AB) and mixed blepharitis (MB) groups. The modified Coston method may still result in some under-counting especially in patients with MGD because it may not detect Demodex brevis since they burrow deep into the sebaceous and meibomian glands. Expressing sebum from plugged meibomian glands, and detecting Demodex microscopically, is a method to diagnose demodecosis in posterior blepharitis, although there are no previous studies to prove its efficacy. Biopsy of the lid margin is still the gold standard in detecting demodecosis, but this is an invasive procedure and not warranted for all forms of blepharitis unless malignancy is a strong consideration. Epilation of lashes is still a useful adjunctive tool to detect Demodex when the clinical presentation may not warrant the biopsy. The incidence and density of Demodex infestation were highest among patients with both anterior blepharitis and meibomian-gland dysfunction. Symptom of lid irritation and presence of cylindrical dandruff are indicative of high density count. These diagnoses and eye findings should alert the clinician about Demodex infestation of the eyelashes, especially in the elderly. Patients with recurrent blepharitis not responsive to current blepharitis treatment regimen should be investigated and treated for Demodex infestation.
Gao Y, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Inves Ophthalmol Vis Sci 2005; 46: 3089-3094.
Alejo RLT, Valenton MJ, Abendanio R. Demodex folliculorum infestation of the lids in Filipinos. Philipp J Ophthalmol 1972; 4: 110-113.
Pena GP, de Souza J, Filho A. Is Demodex really non-pathogenic? Rev Ins Med Trop S Paulo 2000; 42: 171-173.
English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol 1981; 91: 362-372.
Özlem M, Aycan G, Otlu H, et al. Frequency of Demodicosis in various patients and age groups. Türkiye Parazitoloji Dergisi 2007; 31: 115-118.
English FP. Demodex follicullorum and edema of the eyelash. Br J Ophthalmol 1971; 55: 742.
Kheirkhah A, Blanco G, Casas V, et al. Fluorescein dye improves microscopic evaluation and counting of Demodex in blepharitis with cylindrical dandruff. Cornea 2007; 26: 697-700.
Liu J, Sheha H, Fu Y, Tseng SCG. Demodex blepharitis. Advanced Ocular Care May/June 2010: 37-39.
Türk M, Özturk I, Sener AG, et al. Comparison of incidence of Demodex folliculorum on the eyelash follicle in normal people and blepharitis patients. Türkiye Parazitoloji Dergisi 2007; 31: 296-297.
Norn MS. Demodex folliculorum: Incidence and possible pathogenic role in the human eyelid. Acta Ophthalmol (Suppl) 1970; 108: 7–85.
Czeptia D, Kuzna-Grgiel W, Czepita M, Grobelmy A. Demodex folliculorum and Demodex brevis as a cause of chronic marginal blepharitis. Ann Acad Meu Stein 2007; 53: 63-67.
Gutgesel VJ, Stern G, Hood I. Histopathology of MGD. Am J Ophthalmol 1982; 94: 383-387.

