Long-Term Results of Mini-Monoka Monocanalicular Intubation in the Repair of Canalicular Lacerations
Armida L. Suller, MD and Alexander D. Tan, MD
Canalicular injuries may occur following blunt or penetrating trauma to the eyelids.1, 2
Numerous techniques of canalicular laceration repair have been described in the literature but opinions differ on the best method of managing canalicular injuries. Most authors agree on the following points: identification of the transected ends of the canaliculus, mucosal or pericanalicular suturing, and temporary stent placement to prevent blockage in the healing phase.1, 3-9
Canalicular lacerations are traditionally managed by bicanalicular nasal silicone intubation and annular stenting using a pigtail probe. However,these methods are often technically demanding and carry the risk of iatrogenic injury to the normal fellow canaliculus especially in inexperienced hands.1 The challenges that accompany these methods have led to a robust interest in developing a simpler and less invasive means of stenting the laceratedcanaliculus.
Monocanalicular intubation using the Mini-Monoka® (FCI Ophthalmics, Issy-les- Moulineaux, Cedex, France) was introduced by Fayet and Bernard in 1989.15, 16 A major advantage of this procedure is the prevention of damaging the uninvolved canaliculus during surgery. Recent studies have shown promising results with regard to anatomic and functional success when used for canalicularlacerations.
Although the use of Mini-Monoka® has gained popularity, few researchers have addressed the long-term outcomes of its use in monocanalicular lacerations. In this study, we aim to report our experience with the Mini-Monoka stent in canalicular laceration repair in terms of anatomic and functional outcomes. This study also aims to report the epidemiological aspects and clinical profiles of patients with canalicular lacerations who underwent Mini-Monoka® stenting.
MATERIALS AND METHODS
Institutional Review Board Approval
This study was carried out after obtaining approval from the University of the Philippines Manila Research Ethics Board. The study was Ophthalmologyconducted in accordance with the guidelines of the Declaration of Helsinki of 1964, as revised in 2013.
Study Design
This is a retrospective interventional case series.
Patient Selection
The medical records of patients who underwent repair of canalicular laceration with Mini-Monoka® intubation from 2010 to 2015 at the University of the Philippines Manila – Philippine General Hospital were reviewed.
Patients with canalicular lacerations who underwent bicanalicular silicone intubation or those with bicanalicular (i.e., combined upper and lower canalicular) transections were excluded from the study. Patients with incomplete medical records or those who did not return for follow-up were excluded from the study (7 out of the 21 identified patients). The following data were collected: age, gender, canaliculus affected, distance of transection from the punctum, mechanism of injury, associated ocular and periocular injuries, time from injury to repair, surgeon, duration of stent in situ, complications, duration of follow-up, lacrimal apparatus evaluation results (irrigation, probing, and dye disappearance tests), and presence of tearing.
Surgical Procedure
The procedure was done under local anesthesia after obtaining informed consent from the patient.
Proparacaine hydrochloride 0.5% solution was instilled in the conjunctival cul-de-sac followed by infiltration of 1 to 2 mL of 50:50 mixture of bupivacaine 0.5% and lidocaine 2% with 1:100,000 units of epinephrine in the eyelid. Once the medial cut end of the canaliculus was identified, the Mini-Monoka® was inserted in the punctum and out of the lateral cut end of the canaliculus. Them Mini-Monoka® was pulled medially until its collarette securely rests on the punctum. The distal end of the Mini-Monoka® was introduced to the medial cut end of the canaliculus until it passes to the level of the lacrimal sac. Mucosal anastomosis was performed using 6-0 VICRYL® (Ethicon, Somerville, NJ, USA) suture. The eyelid margin and skin were sutured in layers using 6-0 silk. (Fig. 1A-D)
Postoperatively, the patients were given topical antibiotics and steroids. On follow-up, the patients were asked for subjective symptoms of epiphora. The Mini-Monoka® was removed after a period of 3 to 6 months. Dye disappearance test, lacrimal apparatus irrigation, and canalicular probing were performed after stent removal.

Fig. 1. Steps in canalicular laceration repair (surgeon’s view). A, The Mini-Monoka® was gently pulled medially to fixate the circular collarette on the left lower punctum. B, The Mini-Monoka® was inserted into the medial end of the lacerated canaliculus. C, Canalicular mucosal anastomosis was done using 6-0 VICRYL®. D, The eyelid margin and skin were sutured using 6-0 silk.
Outcome and Outcome Measurements
Anatomic success was defined as patent canaliculus on probing (“hard stop”). Functional success was defined as the absence of epiphora or a score of 0 on the Munk scale. A Munk score of 0 corresponds to the absence of epiphora, 1 is occasional epiphora requiring drying or dabbing less than twice a day, 2 is epiphora requiring dabbing two to four times per day, 3 is epiphora requiring dabbing five to ten times per day, 4 is epiphora requiring dabbing more than ten times daily, and 5 corresponds to constanttearing.25
Treatment failure was defined as “soft stop” on lacrimal probing and persistence of epiphora or a Munk score greater than 0.
Data and Statistical Analysis
Means and ranges were used to summarize continuous data while counts and percentages were used to present nominal data. Anatomic and functional success rates were calculated with a 95% exact confidence interval using Clopper-Pearson method.
Data analysis and statistical tests were performed using EpiTools epidemiological calculators (2018).
RESULTS
Complete medical records were obtainable in 14 (12 males and 2 females) out of the 21 identified patients who underwent canalicular laceration repair with Mini-Monoka® intubation. The mean age at the time of surgery was 27 years (range, 16-47 years). Details on the clinical profile and outcomes for each patient are listed on Table 1.
The most common etiology was blunt injury to the face secondary to assault (29%). The other causes of indirect injuries were falls (21%) and facial trauma from a metal bar (21%). The causes of sharp injuries were fingernails (7%), broken glass (7%), scissors (7%), and metal hook (7%).
Lower canalicular injuries comprised 64% of the cases (9 out of 14 patients); 36% of patients had upper canalicular involvement. Nine out of 14 patients (64%) had lacerations located in the proximal canaliculus (within 3 mm from the punctum) while 5 (36%) had midcanalicular injuries (4-8 mm from the punctum). No patient had distal canalicular involvement (≥9 mm from the punctum).
The most common associated injury was periorbital hematoma which occurred in 9 out of the 14 cases (64%). The other accompanying injuries were subconjunctival hemorrhage (21%), orbital fractures (7%), and vitreous hemorrhage (7%).
The mean time from injury to repair was 4 days (range, 1-10 days). Eight surgeries were performed by an oculoplastics fellow (57%), 5 by an ophthalmology resident (36%), and 1 by an oculoplastics consultant (7%). Surgeries performed by the ophthalmology resident were done with the assistance of an oculoplastics fellow. The Mini-Monoka® remained in place for an average of 15.22 months (range, 0.53 to 70.98 months). The mean duration of follow-up was 2.92 years (range,1.28-6.15 years).

Anatomic success or canalicular patency was achieved in 12 out of the 14 patients (86%) (Table 2). None of the 12 patients experienced epiphora resulting in a functional success rate of 100% following re-establishment of anatomical patency after the initial trauma (Table 2).
Two out of the 14 patients (14%) had canalicular obstruction following surgical repair.
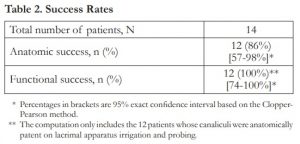
* Percentages in brackets are 95% exact confidence interval based on the Clopper- Pearson method.
** The computation only includes the 12 patients whose canaliculi were anatomically patent on lacrimal apparatus irrigation and probing.
The post-operative eyelid appearance was cosmetically acceptable in all patients with no cases of ectropion or entropion. Two out of the 14 patients had punctal slitting (14%). Premature stent loss at less than 3 months occurred in 2 out of the 14 patients (14%), one occurred at 16 days post-operatively and the other one at 42 days. There were no documented cases of granuloma, infection, or canaliculitis.
DISCUSSION
Bicanalicular nasal silicone intubation has been considered the gold standard in the repair of canalicular injuries, but there is still a debate among oculoplastic surgeons on which method provides the most favorable outcome in terms of canalicular patency and functional outcomes.3 Prior to the introduction of the Mini-Monoka®, it is a common practice to repair canalicular transections by bicanalicular silicone intubation or annular stenting. However, the challenges that accompany these traditional methods of repair have led to an increase in the popularity of monocanalicular intubation. Despite its availability for almost three decades, only a handful of reports have been published on the effectiveness of Mini-Monoka® monocanalicular intubation in maintaining canalicular patency and controlling epiphora after canalicular laceration repair.
The Mini-Monoka® is a solid silicone stent which measures 40 mm with an outer diameter of 0.64 mm. It is secured to the punctum without the need of an additional suture through its plug which has a diameter of 2 mm.19 The stent provides a framework for epithelial growth during the healing phase of the injured canaliculus. This theoretically maintains canalicular patency and prevents scarring of the lumen when kept in place for a minimum of 3 months.
The largest series of patients who underwent repair of canalicular laceration with Mini-Monoka® stent placement was reported by Murchison and Bilyk. Out of the 137 patients with canalicular injury, 118 underwent canalicular repair with Mini-Monoka®. Their patients were mostly males (72.3%) with a mean age of 29.6 years (range, 1.1-74.4 years).24 In our subset of patients, 86% were males in their late twenties (mean, 27 years; range, 16-47 years). A male preponderance was also seen in other studies with most subjects presenting in their twenties to thirties.
Most of our patients had canalicular injury secondary to blunt trauma. This finding is consistent with previous studies that show indirect injuries are a more common cause of canalicular laceration than direct, penetrating injuries.2 Based on the cadaver studies by Wulc and Arterberry, canalicular lacerations caused by indirect diffuse trauma are secondary to eyelid distention to the point of rupture specifically at the segment medial to the punctum – the lacrimal portion of the eyelid.2 Similar to other reports, we found that lower canalicular injuries outnumber those that involve the upper canaliculus. Although one study described the use of 2 Mini-Monoka® stents in bicanalicular lacerations,28 we reserve its use in single-lacerated canaliculus.
Most authors suggest repair of canalicular injuries within 24 to 48 hours. In our study, the mean time from injury to repair was 4 days (range, 1-10 days). Although some patients failed to consult at an earlier date for surgical repair, our study demonstrated that Mini-Monoka® stenting can still produce acceptable outcomes provided that the medial cut end of the injured canaliculus was successfully identified prior to canalicular intubation. One of our patients who underwent repair at 10 days post-injury (Patient 10) maintained canalicular patency and was symptom-free at 2 years post-operatively.
The timing of stent removal varies among oculoplastic surgeons. Most surgeons leave the tubes in situ for 3 months while others perform stent removal after 6-12 months. In an animal study, Conlon et al determined the influence of the timing of silicone stent removal at 4, 8, and 12 weeks on canalicular patency. They concluded that the ideal time for stent removal was at 12 weeks. In our practice, we also maintain the tube for at least 3 to 6 months to increase the canalicular patency rate post-repair. One of our patients (Patient 2) who had an early tube loss at 42 days demonstrated canalicular blockage when evaluated at 5 years post-operatively.
Lacerations involving both the superior and inferior canaliculi carry a poorer prognosis than monocanalicular injuries in terms of the occurrence of post-traumatic epiphora. While most surgeons agree on performing silicone intubation for bicanalicular injuries, there have been different views on the repair of single-lacerated canaliculus especially those which are superiorly located.3 Some surgeons believe that the lower canaliculus plays a major role in tear drainage, while the upper canaliculus has almost no importance in this function.13-14 Because of this viewpoint, some authors do not perform endocanalicular anastomosis in patients with superior canalicular lacerations.25 However, other studies have confirmed that the upper and lower canaliculus play an equivalent role in tear drainage.31-33 In a survey by Ho and Lee, 43% (38 out of 89) of surgeons in the United Kingdom would perform surgical repair if only the inferior canaliculus was lacerated while 40% (36 out of 89) would always repair a monocanalicular injury regardless of its superior or inferior location.3 In our study, we performed Mini-Monoka® intubation in all patients who presented with upper or lower canalicular transection. Two out of our 14 patients (Patients 2 and 12) who developed total canalicular obstruction post-stent removal did not experience epiphora. Both patients had upper canalicular involvement. Patency of the uninjured lower canaliculus in these 2 patients was confirmed by lacrimal apparatus irrigation and complete clearance of fluorescein dye after 5 minutes. The results of our study reinforce the findings of other authors that a solitary functioning canaliculus may be adequate to prevent post-traumatic epiphora.1, 7, 10 Therefore, it is judicious to attempt repair and intubation of a singly lacerated canaliculus, whether superiorly or inferiorly located, because the risk of future injury to the normal functioning canaliculus cannot be predicted.
We achieved an 86% percent anatomical success rate with the use of Mini-Monoka® after a mean follow-up period of 2.92 years post-operatively. Other studies achieved a canalicular patency rate between 79-100%. This is comparable to the reported success rate of bicanalicular nasal intubation in the repair of canalicular lacerations which is between 78%-94%.12, 34 However, a disadvantage of bicanalicular nasal intubation is that it requires general anesthesia. Annular stenting with the use of the pigtail probe has also been described. The reported success rate of this procedure in terms of canalicular patency post-repair is between 36.6-98.5%.4, 11, 13 Although the use of the pigtail probe in canalicular repair can be done under local anesthesia, intubation may be technically difficult to perform in patients who lack a true common canaliculus. Saunders et al reported a 10% incidence rate of iatrogenic damage to the uninjured canaliculus following the use of a pigtail probe.13 This incidence rate may reflect the fact that in 10% of the population, the superior and inferior canaliculi drain directly into the lacrimal sac without joining together in a common canaliculus.35 Mini-Monoka® intubation is a relatively simpler and less technically challenging procedure than bicanalicular nasal intubation and pigtail probe-assisted annular stenting. Unlike the other two procedures, it does not require manipulation of the intact or uninjured canaliculus.1, 7, 20, 22-24
Most of the canalicular repairs (13 out of 14 cases) in our study were done by trainees (ophthalmology resident and oculoplastics fellow). When the procedure performed by the oculoplastics consultant was excluded, the anatomical success rate is 85% (11 out of the 13 cases); this is within the reported success rate of Mini-Monoka® stenting, which is between 79-100%. Murchison and Bilyk stated that the level of training correlates with the surgical outcome of canalicular laceration repair, with the oculoplastics consultant achieving the highest surgical success rate compared to that of the oculoplastics fellow and ophthalmology resident.24 In our series, we found that trainees were able to produce good surgical outcomes. It should be noted, however, that all procedures performed by the ophthalmology resident were done under the supervision of the oculoplastics fellow. Given the small number of patients in our study, we cannot compare the success rates of the oculoplastics consultant versus the oculoplastics fellow.
All patients in this study had lacerations located in the proximal and middle thirds of the canaliculus. For more distal injuries (at least 9 mm medial to the punctum) or those that are close to the lacrimal sac, we prefer the use of bicanalicular nasal intubation. We agree with Murchison and Bilyk that Mini-Monoka® might not be able to sustain the distal tension during canalicular laceration repair especially if a medial canthal tendon injury is present.24
One of the main problems encountered with the use of Mini-Monoka® is premature stent loss which is reported between 7-29%. In our series, two out of the 14 patients (14%) had accidental early tube removal; one was at 16 days (Patient 4) and the other one at 42 days post-repair (Patient 2). Leibovitch et al, however, did not encounter premature stent loss in their series of 19 patients.20 Several studies described the use of Mini-Monoka® in younger patients. We generally avoid its use in this group of patients because of the higher incidence of premature extrusion in the pediatric population. We did, however, perform Mini-Monoka® intubation in a 16-year-old male since the patient was cooperative enough to undergo the surgery and follow post-operative instructions.
Punctal slitting is also one of the uncommon complications associated with Mini-Minoka®. Two of our 14 patients (Patients 4 and 6) had punctal slitting post-operatively but canalicular patency was still achieved and none complained of epiphora. One of the patients who had a punctal slit also experienced early stent loss at 2 weeks post-repair after accidentally pulling out the tube (Patient 4). It has been stated earlier that stent loss before 3 months is associated with high anatomical failure rate. Interestingly, his canaliculus remained patent at more than 2 years post-stent extrusion. In this patient, the canalicular laceration was located 1 mm medial to the punctum. Since the area of transection was very near the punctum, the punctal slit may have inadvertently “marsupialized” or exposed the normal intact part of the canaliculus medial to the area of the laceration, therefore, facilitating tear drainage.
None of our patients experienced eyelid malposition, granuloma formation, or infection. Even though there were patients who failed to return at the clinic for stent removal at 3 months, they remained asymptomatic and did not experience any of the complications mentioned above. In our study, 3 patients (Patients 8, 9, and 10) had their stents removed at a mean of 2.41 years post-operatively and in one patient (Patient 1), the Mini-Monoka® remained in situ for 5.91 years. As far as we know, we have documented the largest series of patients with the longest Mini-Monoka® retention period in the literature. Anastas et al reported one patient with retained Mini-Monoka® for 3.83 years who remained symptom-free despite failing to return at the scheduled follow-up.
Our present study is limited by the small number of patients. This is attributable to the inconsistent availability of the Mini-Monoka® in our country in the previous years; therefore, most of the canalicular lacerations that we encountered were repaired with bicanalicular nasal silicone intubation. Even though our study population is small, our results reinforce previous findings that the Mini-Monoka® can be successfully used for monocanalicular injuries. Our study also represents the largest series of patients who underwent Mini-Monoka® monocanalicular intubation in the Philippines. Our results are promising and should be validated by a larger sample size. A prospective, randomized study needs to be carried out to compare the long-term outcomes of monocanalicular versus bicanalicular intubation in the repair of canalicular lacerations.
We recommend the use of the Mini-Monoka® stent in lacerations involving the proximal and middle segments of the canaliculus. For transections close to the lacrimal sac (i.e., distal canaliculus) or those involving both upper and lower canaliculi, we perform bicanalicular silicone intubation to maintain distal support which cannot be adequately addressed by monocanalicular stenting. Mini-Monoka® monocanalicular intubation is a relatively simpler procedure compared to the traditional methods of repair since it does not require additional sophisticated instrumentation during canalicular repair such as the Crawford hook for tube retrieval in bicanalicular intubation and the pigtail probe in annular stenting. A major advantage of Mini-Monoka® monocanalicular intubation is that it can be performed in the minor operating room or office with local infiltration of anesthetics and avoids the possible side effects of general anesthesia especially in high-risk or elderly patients. The Mini-Monoka® can be easily removed by pulling the punctal fixation device with forceps. This is faster, simpler, and produces less patient discomfort than locating and retrieving the ends of the bicanalicular stent in the nose during tube removal. Chronic nasal irritation, which may occur with bicanalicular silicone intubation, is also avoided with the use of the Mini-Monoka® since it only traverses the transected ends of the canaliculus and does not reach the nasal cavity. While early intervention is recommended in canalicular injuries, it is still prudent to attempt locating the medial cut end of the canaliculus in patients who present later than 1-2
days post-injury since successful intubation could still prevent canalicular obstruction in the long term. We wait for at least 3 months before tube removal but as long as there are no signs of irritation, infection, or punctal slitting, we leave the Mini-Monoka® in place for as long as 6 months. Most of the patients in this study failed to adhere to the scheduled date of follow-up at the clinic which explained why some tubes were retained at 1, 2, and even at almost 6 years post-repair. We assume that the tendency of the patients to delay their follow-up is related to the absence of symptoms while the Mini-Monoka® remained in situ. This suggests that the Mini-Monoka® is safe and well-tolerated even if inadvertently left in place beyond the intended removal time at 3-6 months.
In this study, Mini-Monoka® monocanalicular intubation has been shown to be effective in maintaining the long-term patency of the injured canaliculus with the anatomic and functional success rates comparable to that of the gold standard. The simplicity, tolerability, and safety profile of this minimally invasive procedure makes it a viable alternative to the conventional methods of canalicular repair in carefully selected patients.
ACKNOWLEDGEMENT
The authors would like to thank Dr. Septemius A. Pansacola for his technical assistance.
REFERENCES
1. Naik MN, Kelapure A, Rath S, et al. Management of canalicular lacerations: epidemiological aspects and experience with Mini-Monoka canalicular stent. Am J Ophthalmol 2008;145:375-380.
2. Wulc AE, Arterberry JF. The pathogenesis of canalicular laceration. Ophthalmology 1991;98:1243-1249.
3. Ho T, Lee V. National survey on the management of lacrimal canalicular injury in the United Kingdom. Clin Exp Ophthalmol 2006;34:39-43.
4. Jordan DR, Nerad JA, Tse DT. The pigtail probe, revisited. Ophthalmology 1990;97:512-519.
5. Kersten RC, Kulwin DR. “One-stitch” canalicular repair. A simplified approach for canalicular laceration. Ophthal-mology 1996:103:785-789.
6. Neuhaus RW. Silicone intubation of traumatic canalicular lacerations. Ophthal Plast Reconstr Surg 1989;5:256-260.
7. Anastas CN, Potts MJ, Raiter J. Mini Monoka silicone monocanalicular lacrimal stents: subjective and objective outcomes. Orbit 2001;20:189-200.
8. Forbes BJ, Katowitz WR, Binenbaum G. Pediatric canalicular tear repairs – revisiting the pigtail probe. J AAPOS 2008;12:518-520.
9. Kennedy RH, May J, Dailey J, et al. Canalicular laceration: an 11-year epidemiologic and clinical study. Ophthal Plast Reconstr Surg 1990;6:46-53.
10. Worst JG. Method for reconstructing torn lacrimal canaliculus. Am J Ophthalmol 1962;53:520-522.
11. Jordan DR, Gilberg S, Mawn LA. The round-tipped, eyed pigtail probe for canalicular intubation: a review of 228 patients. Ophthal Plast Reconstr Surg 2008;24:176-180.
12. Wu SY, Ma L, Chen RJ et al. Analysis of bicanalicular nasal intubation in the repair of canalicular lacerations. Jpn J Ophthalmol 2010;54:24-31.
13. Saunders DH, Shannon GM, Flanagan JC. The effectiveness of the pigtail probe method of repairing canalicular lacerations. Ophthalmic Surg 1978;9:33-40.
14. Walter WL. The use of the pigtail probe for silicone intubation of the injured canaliculus. Ophthalmic Surg 1982;13:488-492.
15. Fayet B, Bernard JA, Pouliquen Y. Repair of recent canalicular wounds using a monocanalicular stent (in French). Bull Soc Ophthalmol 1989;89:819-825.
16. Fayet B, Bernard JA. A monocanalicular stent with self-stabilizing meatic fixation in surgery of excretory lacrimal ducts. Initial results. Ophtalmologie 1990;4:351-357.
17. Chowdhury HR, Rose GE, Ezra DG. Long-term outcomes of monocanalicular repair of canalicular lacerations. Ophthalmology 2014;121:1665-1666.
18. Nam SM. Microscope-assisted reconstruction of canalicular laceration using mini-Monoka. J Craniofac Surg 2013;24:2056-2058.
19. Eo S, Park J, Cho S, et al. Microsurgical reconstruction for canalicular laceration using Monostent and Mini-Monoka. Ann Plast Surg 2010;64:421-427.
20. Leibovitch I, Kakizaki H, Prabhakaran V. et al. Canalicular lacerations repair with the Mini-Monoka monocanalicular intubation stent. Ophthalmic Surg Lasers Imaging 2010;41:472-477.
21. Lee H, Chi M, Park M, et al. Effectiveness of canalicular laceration repair using monocanalicular intubation with Monoka tubes. Acta Ophthalmol 2009;87:793-796.
22. Sendul SY, Cagatay HH, Dirim G, et al. Reconstructions of traumatic lacrimal canalicular lacerations: a 5 years experience. The Open Access. J Sci Technology 2015;3. Available at: http://www.agialpress.com/journals/oajost/2015/101121/. Accessed: November 7, 2015.
23. Biradar SG, Kansara DU. Minimonoka stent for canalicular reconstruction. JKIMSU 2015;4:65-69.
24. Murchison AP, Bilyk JR. Canalicular laceration repair: an analysis of variables affecting success. Ophthal Plast Reconstr Surg 2014;30:410-414.
25. Munk PL, Lin DT, Morris DC. Epiphora: treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiology 1990;177:687-690.
26. Sergeant ESG. EpiTools epidemiological calculators. Ausvet Pty Ltd. Available at: http://epitools.ausvet.com.au. Accessed: March 4, 2018.
27. Conlon MR, Smith KD, Cadera W et al. An animal model studying reconstruction techniques and histopathological changes in repair of canalicular lacerations. Can J Ophthalmol 1994;29:3-8.
28. Naik MN, Gupta R, Honavar SG. Bicanalicular laceration managed with two Mini-Monoka monocanalicular stents. Orbit 2008;27:135-137.
29. Reifler DM. Management of canalicular laceration. Surv Ophthalmol 1991;36:113-132.
30. Long J, Tann T. Adnexal trauma. Ophthalmol Clin North Am 2002;15:179-184.
31. Jones LT, Marquis MM, Vincent NJ. Lacrimal function. Am J Ophthalmol 1972;73:658-659.
32. Lemp MA, Weiler HH. How do tears exist? Invest Ophthalmol Vis Sci 1983;24:619-622.
33. Linberg JV, Moore CA. Symptoms of canalicular obstruction. Ophthalmology 1988;95:177-179.
34. Dortzbach RK, Angrist RA. Silicone intubation for lacerated lacrimal canaliculi. Ophthalmic Surg 1985;16:639-642.
35. Kikkawa DO, Lemke BN. Orbital and eyelid anatomy. In: Dortzbach RK, editor. Ophthalmic Plastic Surgery: Prevention and Management of Complications. New York, (NY): Raven Press; 1994. pp 1-29.

