Translation and validation of a Filipino version of the glaucoma quality-of-life questionnaire
Carlo Josemaria D Rubio, MD; M B Agulto, MD
Glaucoma causes characteristic visual-field loss and optic neuropathy. If severe enough, it can lead to significant visual disability1-2 and affect quality of life. A patient’s ability to enjoy normal life activities can be compromised. This can be assessed through specific validated tools, such as the different health-related qualityof-life questionnaires (HRQoL). The use of a HRQoL allows the patient’s perspective to be included in the methodological framework of evidence-based medicine. These questionnaires have shown usefulness in assessing various life-threatening, progressive, or chronic illnesses, such as glaucoma.3
Some of these quality-of-life assessment tools have been used to assess the quality of life of glaucoma patients. Several of the questionnaires are not disease-state specific, such as the Medical Outcomes Study Short Form 36 (SF-36) and the Sickness Impact Profile (SIP). SF 36 is an easy-to-use questionnaire known as a multipurpose medical-health survey. Despite being considered reliable, it has not been shown to correlate well with vision-related ailments, such as glaucoma. The SIP is considered a valid and reliable tool for assessing quality of life in disease states, but is deemed impractical in clinical setting due to the length of time it takes to complete the questionnaire. 4
Other questionnaires are vision specific, but not necessarily specific for glaucoma. Examples are the Visual Function Index-14 (VF-14), the National Eye Institute Visual Function Questionnaire (NEI-VFQ), and the NEIVFQ 25. The VF-14 was originally developed to assess quality of life of cataract patients and has only moderate relevance to assessing impact of visual acuity on quality of life among glaucoma patients. Since it failed to take into consideration the effects of visual field and color vision defects, two important indicators of optic-nerve damage, it has proved inadequate in measuring quality of life in glaucoma.
The NEI-VFQ, a well-validated tool in assessing vision-dependent tasks, is more sensitive than the SF-36 in differentiating patients with glaucoma, but is difficult to use. The NEI-VFQ 25 is an improved version of the NEI-VFQ. Despite being easy to use, well validated, and reliable, its lack of emphasis on visual-field effect on quality of life has lessened its test value in glaucoma. In spite of its shortcomings, it is one of the more widely used (and translated) visual-field-function questionnaires. Along with the NEI-VFQ, it has become the benchmark for quality-of-life questionnaires specific to glaucoma.4 There have been various attempts in the past decade to create a glaucoma-specific HRQoL. Rouland and colleagues of the Hôpital Claude Huriez in Lille, France, noted a lack of HRQoLs for ophthalmologists. They created the first glaucoma-specific quality of life scale to provide researchers and physicians a comprehensive, practical, and validated tool for assessing patients with glaucoma.3
The Glaucoma Quality-of-Life Questionnaire (GQL 15) was designed by Nelson and colleagues in 2003.5 They attempted “to explore patients self-reported visual disability resulting from glaucoma by means of a questionnaire developed for this purpose; identify activities strongly associated with a measure of visual-field loss; quantify different psychophysical aspects of visual function; and assess the relationship between objective measures of visual function and patients’ perception of their vision-related quality of life.” Of the 50 questions used in the study, 15 were noted to have a strong and significant relationship with a measure of visual-field loss, which comprise now the GQL 15. The perceived visual disability relating to dark adaptation, disability glare, activities demanding functional peripheral vision was highly associated with the severity of binocular visual-field loss. The GQL 15 was developed to include 5 key activity groups in daily living, namely central and near vision, peripheral vision, dark adaptation and glare, personal care, and outdoor mobility.
The GQL 15 has been used in various studies. Goldberg and associates used the GQL 15 to quantify difficulty in the performance of daily activities in patients with openangle glaucoma (OAG). They demonstrated that patients with OAG had a significant deterioration in quality of life which correlated strongly with reduced visual acuity, severity of visual-field defects, and presence of binocular field defects.6
Country-specific quality-of-life questionnaires were also developed. Toit and colleagues developed and validated a vision-specific quality-of-life questionnaire of East Timorese.7 Krochik et al. translated the National Eye Institute Visual Function Questionnaires into Spanish in Buenos Aires, Argentina.8 Currently, there is no validated Filipino glaucoma quality of life questionnaire. This study aimed to develop and validate a vision- and language- or vernacular-specific GQL–15 adapted to Filipino glaucoma patients, which could reveal peculiar self-proclaimed insights into the debilitating effects of glaucoma on vision and life itself. We translated the Glaucoma Quality of Life Questionnaire 15 (GQL–15) into Filipino, determined its value, and validated its usefulness among patients.
METHODOLOGY
After assessment of the different vision-specific qualityof-life questionnaires, the Glaucoma Quality of Life Questionnaire–15 (GQL–15) was used as basis for the Filipino questionnaire. The translation procedure involved translation, reconciliation, pretesting, and small-group discussion based on the Kidscreen group Translation and Validation procedure. 9 Modifications to the translation and validation procedure were suggested and approved by an expert. The GQL–15 was translated into a Filipino version using the forward-backward-forward method. The questionnaire was first translated into Filipino by one independent translator (forward translation) who was a native speaker Filipino speaker, proficient in both English and Filipino, and familiar with the cultures of both the English-speaking countries and the Philippines. The forward translation was translated back into English by a second translator, who had not worked with the original GQL–15. Members of the research group with good knowledge of English and Filipino, as well as the forward translators, compared the backward translation with the original GQL–15.
The group compared the backward translation with the original GQL–15 item by item, eventually suggesting a version for the final forward translation. The back-translated and original questionnaire should have been very similar. The discrepancies between the two questionnaires were identified and resolved. The reconciliation process was confirmed for certain translations and an alternative suggestion was given to other translations which were not confirmed. The end product was the final forward translation, which was expected to not have any conceptual discrepancies with the English original. The entire process of translation was documented appropriately. Additional questions specific for the Filipino way of life were generated as necessary by interviews with diagnosed glaucoma patients, additional literature review, and consultation with experts in the field of glaucoma. Patients from the Sentro Oftalmoligico Jose Rizal of the University of the Philippines–Philippine General Hospital (UP–PGH), diagnosed to have glaucoma, made up the study population. Included were patients who:
• had been diagnosed with primary glaucoma, whether open-angle or angle-closure, and had been seen by at least one consultant;
• were more than 20 years old and can read, write, and speak in conversational Filipino;
• had best-corrected distance visual acuity of 20/40 or better;
• had undergone at least 2 automated visual-field tests since the time of diagnosis (the perimetry tests should be reliable, with less than three fixation losses and both false-negative and false-positive responses less than 10% each and the tests should have been officially read by a consultant);
• were deemed to be neurologically capable of answering the questionnaire (i.e. those oriented to time/place/person, those with intact sensorium);
• who have had at least one photo of the optic nerves officially read by a consultant;
• may or may not have undergone glaucoma-related surgery (filter, valve, or laser surgery) or cataract surgery; and
• had been regularly consulting (at least 4 follow-ups) at the UP–PGH Glaucoma Clinic within the past calendar year.
Excluded were patients who:
• had eye diseases other than glaucoma (retinal pathologies, non-glaucomatous optic-nerve pathologies) or glaucoma secondary to an underlying eye disease;
• had undergone eye surgery not directly related to the primary glaucomatous pathology (i.e. retina surgery, penetrating keratoplasty, panretinal photocoagulation, etc.);
• were unable to read, write and converse in conversational Filipino. A control group of patients with no known eye disease affecting vision to below 20/40 for distance vision with appropriate correction (i.e. correctible error of refraction) was recruited from the general clinic. Patients were asked to fill up a consent form indicating their willingness to participate in the study. The patients’ name, age, sex, educational attainment and diagnosis were noted.
Pretesting
The translated questionnaire was pretested vis-à-vis the original questionnaire to determine its functionality (whether it was too hard to understand, confusing, inadequate, or there were other issues the interviewees wanted addressed) and whether or not there is a need for a Filipino version of the glaucoma quality-of-life questionnaire in the first place. The questionnaire was intervieweradministered. The patients were asked to score themselves on a scale of 1 to 10 regarding their self-assessed proficiency in English and Filipino. They were interviewed with both questionnaires (English and Filipino). The selection of the first questionnaire to be used was done randomly (flip of a coin). After the scores were taken, the patients were asked regarding their comments on both questionnaires and whether they understood better and preferred the questionnaire in Filipino or English. Small-group discussion The pretesting results were discussed by the researchers along with another individual familiar with the use of screening tools in the health social sciences in a small-group discussion (SGD) to determine whether the translated questionnaire could be adequately understood and answered by the patients (based on their comments given during the pretesting phase). The SGD also took into consideration the comments of the patients regarding the content of the questionnaire. Specific items in the questionnaire were modified or altogether removed depending on the patients’ comments and the SGD analysis. The SGD also determined whether or not a Filipino questionnaire was necessary based on the difference of the patient’s scores (or lack thereof) in the English vs. the Filipino questionnaire and on the understanding and preferences of the patients. The SGD came up with the final Filipino Glaucoma Quality of Life Questionnaire.
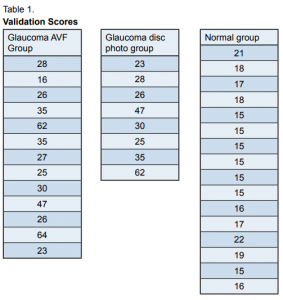
Validation of questionnaire as a glaucoma-screening tool Time-based sampling was used to select the patients to be screened during the testing period (patients who qualified for either group, whether the glaucoma group or the control group, who came in during a one-week period at the clinics.) The patients underwent a comprehensive interview and ophthalmologic examination. A researcher associate administered the questionnaire to the patients through an interview. Any comments from the patients regarding the questionnaires and mode of administration were noted. The glaucoma patients were divided into two subgroups: those with primarily visual field defects (glaucomatous-visual- field group or GVF) and those with large glaucomatousdisc- photo or GDF. The mean scores of each subgroup were computed and compared with those of the normal group using independent t-test. The level of significance was set at p = 0.05.
RESULTS
Selection of questionnaire The SF–36, NEI VFQ–25, and the GQL–15 were considered for use in the study. Studies assessing the different quality-of-life questionnaires showed that the GQL–15 has good correlation with the clinical indices of glaucoma.3-6 It was, therefore, selected for translation. Translation procedure The research group discussed the results of the translation process, paying attention to the similarity or dissimilarity of the forward translation to the original GQL–15. The main discrepancy between the two involved the grading of the severity of difficulty. The original choices in the GQL 15 The forward translation’s choices 0 – do not perform for nonvisual reasons 0 – does not involve vision to perform task.
1 – none 1 – no difficulty
2 – a little bit 2 – some degree of difficulty
3 – some 3 – frequently experiencing difficulty
4 – quite a lot 4 – difficult to perform task due to blurred vision
5 – severe 5 – cannot perform task due to no vision The first two (1 and 2) were similar to the original versions but not the last four. The discrepancy was traced to the forward translation. The back translation was similar to the forward translation in terms of the different possible answers regarding severity of difficulty. However, it was the forward translation that was noted to be significantly dissimilar to the original, with the item “3 – some” being translated into “3 – madalas,” “4 – quite a lot” being translated into “4 – hirap nang makakita,” and “5 – severe” being translated into “5 – wala nang makita.” It was agreed upon by the research group that the forward translation needed to be rectified, with the final forward translation of the different answers for severity being “1 – kung ang sagot ay hindi, 2 – kung medyo nahihirapan nang kaunti, 3 – kung medyo madalas mahirapan, 4 – kung may malaking hirap, and 5 – kung may matinding hirap.” The vernacular translation was made more faithful with regard to quantification. Most of the 15 items that represented daily activities were deemed to have been adequately translated. Item 2, originally “walking after dark” was eventually back-translated into “walking in dark alleys.”
The forward translation was similar to the original text, and it was agreed upon that the problem was with the forward translation and not the backward translation. Item 3, originally “seeing at night” was eventually translated into “finding objects in the dark.” The backward translation was deemed responsible for the discrepancy, having translated the original item into “pagtingin-tingin o paghahanap ng bagay sa dilim.” This item was agreed upon to be translated to Filipino as “pagkita sa gabi,” in the final forward translation. Item 9, originally “seeing objects coming from the side” was translated in the back translation into “looking at objects around you.” The forward translation was deemed to be adequate. The discrepancy was agreed upon to be in the back translation and thus the original forward translation “nakikita ang bagay sa paligid” was maintained. Item 13, originally “judging distance of foot to step/curb” was eventually translated into “depth perception in stepping” in the back translation. The forward translation, “pagtantya ng distansya ng paa papunta sa bangketa” was deemed to be adequate, and the problem was with the backward translation and so the original forward translation was maintained. A final forward translation was agreed upon. The different translations are in the appendix.
Pretesting
The final forward translation was used in a pretest: 5 glaucoma and 4 normal patients were interviewed. The patients with glaucoma had educational attainment ranging from grade school to college undergraduate. The patients’ self-rating on English proficiency averaged 4.6, with the lowest score 2, and the highest score 8. The patients’ self-rating on Filipino proficiency averaged 9, with the lowest score 7 and the highest score 10 (3 patients). There was a difference in the average scores of the English and Filipino questionnaires of 4.4, the lowest 2 and the highest 8. The absolute value of the difference of the scores per item was also totaled, with an average of 15. The biggest absolute value difference between the two scores was 31. There were also scores with small differences of between 2 and 9. The control population had educational attainment ranging from grade school to high school. They had an average rating for English proficiency of 6.25 with the highest score 8 and the lowest 5. They had an average Filipino proficiency of 9, with the lowest 8 and the highest 10. The average difference in scores was 7.25. The average difference in the absolute values of the differences in scores per item was 7.75. All in all, 6 out of 9 patients had a self-proficiency rating in English at least 5 points lower than in Filipino. Three of these patients were responsible for the scores that had a large difference in the sum of absolute values of differences in scores per item. The average self-rating was 5.3/10 in English proficiency and 9/10 Filipino proficiency. Seven out of /9 commented that they found the Filipino questionnaire easier to understand and answer compared to the English questionnaire, with the rest commenting the opposite. None of the respondents found the need for additional questions.
Small-group discussion
The results of the pretest were discussed by the research group along with an expert. It was deemed that although not all participants had a large difference in the scores obtained from using the English vs. the Filipino questionnaire, the presence of individuals with large differences of answers of the English vs. the Filipino questionnaire was enough reason to have a Filipino questionnaire. This was validated by the preference of all but 2 patients to answer the Filipino questionnaire. Based on the results of the pretest, none of the items in the translated questionnaire were modified and no items were added. It was a agreed upon that there was enough reason warrant the need for the use of a Filipino version of the GQL–15, and that the final forward translation of the questionnaire could be used as is.
Validation
The final forward translation was administered to patients fulfilling the inclusion criteria. Time-based sampling (1 week or 5 clinic days) was used. A total of 13 patients with glaucomatous-visual-field findings and 8 patients with glaucomatous-disc-photo findings qualified for the study. The scores of patients with glaucomatous visual fields ranged from 16 to 64, with an average of 34.15/75. The scores of patients with glaucomatous-discphoto findings ranged from 23 to 62, with an average of 34.5/75 (Table 1). The final forward translation was also administered to normal population composed of 16 patients. Their scores ranged from 15 to 21, with an average score of 16.81 (Table 1). The average score of the group with glaucomatousvisual- field findings was compared to the average score of the control group using an independent t-test. The null hypotheses were there was no significant difference between the groups with glaucoma and the normal/ control group. The computed t-value of the group with glaucomatous visual fields was 2.66. The computed t-value of the group with glaucomatous disc photos was 2.54. With a p value of 0.05, it was noted that the t values of the glaucomatous visual field group and the glaucomatous optic disc group were higher than the t-values for their respective degrees of freedom based on sample size. Both null hypotheses were rejected and the alternative hypotheses were accepted. There was a significant difference between the group with glaucomatous visual fields and the normal/control group. There was also a significant difference between the group with glaucomatous disc photos and the normal/control group.

DISCUSSION
The GQL–15 was chosen since it was shown to have good correlation with clinical indices of glaucoma. It should be noted that the GQL–15 is just a vision-related quality-of-life questionnaire. The other vision-related quality-of-life questionnaires were not disease-specific. The GQL–15 includes questions on central and near vision (questions 1, 14 and 15), peripheral vision (questions 8, 9, 11, 12), dark adaptation and glare (questions 2, 3, 5, 6 and 7), personal care (14) and outdoor mobility (questions 4, 10 and 13). The translation procedure was straightforward, with the two translators producing the required output. It was noted during evaluation of the translations that the most difficult part for both translators was translating the scale of the answers to the questionnaire, as described in the results. The research group carefully reconciled the differences between the two translations and compared them to the original questionnaire to produce the final translation. The difficulty in translation was attributed to the lack of a definite translation in Filipino of the English scale used in the original GQL–15 Questionnaire. The rest of the discrepancies as discussed in the results were agreed upon to be minor differences, with the discrepancies rectified in the final forward translation. The results of the pretest convinced the members of the small group discussion that a Filipino version of the GQL–15 Questionnaire was needed. Out of the 9 pretested individuals, 7 remarked that they had an easier time answering the Filipino version of the questionnaire.
The average of the self-rating in English proficiency of the pretested patients was 5.33/10 as against 9/10 in Filipino proficiency, which the researchers deemed to be a significant difference. Six out of the 9 pretested individuals had a self-rating in English proficiency 5 points (out of 10) lower than in Filipino proficiency, which the group also found to be significant. What was even more significant were the 3 patients whose sum of the absolute value of the differences of scores answered for each question in Filipino and English were 23, 29 and 31, representing a large difference in the answers given when the patients were asked the same question in English and in Filipino. These patients had self-rating in English proficiency at least 5 points out of 10 lower than in Filipino proficiency. These same patients were also part of the group which remarked that they had an easier time and preferred answering the Filipino questions.
Subjectively, it was noted during the interview that these same patients had a difficult time understanding the English questions, but had an easier time answering the Filipino questions. Given all these data, the group assessed that these patients had a difficult time understanding and answering the English questionnaire. Majority of the respondents also preferred answering the Filipino questionnaire. All these data and observations showed that the there was enough reason to produce a Filipino version of the GQL–15. The validation showed that the scores of the groups with glaucoma were around double that of the normal population. Based on the independent t-test, there was a statistically significant difference between the scores of the glaucoma patients and the normal population, using the final forward translation of the GQL–15 (p = 0.05). Since, like the English version of the questionnaire, the Filipino version was able to have significantly different scores between the two groups, the research group determined that the final forward translation was a valid version of the GQL–15.
In summary, the GQL–15 was successfully translated into Filipino.
The English version of the GQL–15 will not suffice for measuring quality of life in most Filipino patients. Filipino version of the GQL–15 is necessary to meaningfully monitor Filipino patients with glaucoma, and seems superior to the English version in doing so. The final forward translation of the Filipino Glaucoma Quality of Life Questionnaire is a valid tool in assessing quality of life in patients with glaucoma. A larger population may be used in both the normal and glaucoma groups to more strongly validate the Filipino version of the questionnaire as a valid tool in assessing quality of life among glaucoma patients. The questionnaire may be used to determine whether there is increasingly poorer quality of life in patients with increasingly more severe glaucoma, with regard to both structure and function.
References
1. South East Asia Glaucoma Interest Group Asia Pacific Guidelines, Second Edition
2. American Academy of Ophthalmology Basic and Clinical Science Course, Glaucoma, 2004-2005.
3. Rouland JF, Denis P, Béchetoille A, et al. Du Groupe D’étude Glaucome Et Qualité De Vie. Creating a specific quality-of-life questionnaire in patients with glaucoma: item generation. J Fr Ophthalmol 2002; 25: 785-794.
4. Severn P, Fraser S, Finch T, May C. Which quality-of-life score is best for glaucoma patients and why? BMC Ophthalmology 2008 Jan 23: http://www.biomedcentral. com/1471-2415/8/2 (accessed October 21, 2009).
5. Nelson P, Aspinal P, Papasouliotis O, et al. Quality of life in glaucoma and its relationship with visual function. J Glaucoma 2003; 12: 139-150.
6. Goldberg I, Clement CI, Chiang TH, et al. Assessing quality of life in glaucoma patients using the Glaucoma Quality of Life–15 (GQL–15) Questionnaire. J Glaucoma 2009; 18: 6-12.
7. du Toit R, Palagyi A, Ramke J, et al. Development and validation of a visionspecific quality-of-life questionnaire for Timor-Leste. Invest Ophthalmol Vis Sci 2008; 49: 4284-4289.
8. Krochik V, Loayza Gamboa W, Saenz Valiente A, Lerner F. Quality of life in patients with glaucoma in Buenos Aires, Argentina. Presented at ARVO Meeting April 2011. Invest Ophthalmol Vis Sci 2008; 49: 1585.
9. Kidscreen Group. Kidscreen Translation and Validation Procedure. 2004. http:// www.kidscreen.org/cms/newtranslation (accessed October 21, 2009).

