The Quality of Life in Patients with Non-Surgical and Surgical Presbyopic Corrections
Robert Edward T. Ang, MD, Abigail O. Panganiban, MD, Ma. Melizza Theresa Toledo-Ramirez, MD, Gladness Henna A. Martinez, MD, Dennis C. Vizconde, MD
Presbyopia is the age-related decline in accommodation. This process usually becomes perceptible between ages 40 to 50 and accelerates with age. Changes in the shape, size, and mechanical characteristics of the lens, as well as the function of the ciliary muscle have all been theorized to decrease the amplitude of accommodation.1
Optical solutions to improve near vision in presbyopic patients can be classified as surgical or nonsurgical. Nonsurgical solutions include the use of bifocals, progressive eyeglasses, and contact lenses (multifocal or monovision).2 Surgical presbyopic correction can be classified into cornea-based and lens-based techniques. Corneal presbyopic treatments, such as presbyopic LASIK (Supracor)3 or inlays (Acufocus Kamra),4 are performed on patients with no cataract, typically in the 40-60 year age group. Patients with cataract, usually aged above 60 years, undergo cataract surgery with implantation of an intraocular lens (IOL). Patients can choose a non-presbyopia-correcting monofocal IOL or presbyopia-correcting lenses which can be a multifocal or an accommodating lens.
The choice of optical correction for presbyopia can be influenced by many factors among which are the amount of visual disability, desire for spectacle inde-pendence, occupational and recreational needs, cost of treatment, availability of the procedure, discomforts and inconveniences, motivation for aesthetic appear-ance, and fear of side effects. Regardless of the form of optical solution, each patient has his/her own perceived satisfaction with the current state (with eye-glasses or spectacle-free) and the subsequent effect on the quality of life.
Uncorrected near-vision impairment caused by presbyopia may have a negative impact on activities of daily living, career options, and self-esteem. According to a worldwide census data, one-third of the population is older than forty.5 As the global population ages, the prevalence of presbyopia will increase. Presbyopia is commonly overlooked as a major source of disability due to the ease of acquiring reading glasses.6
With an increasing demand for spectacle independence, presbyopic LASIK, corneal inlays, multifocal and accommodating intraocular lenses were developed for optimum spectacle-free visual function. The safety and efficacy of these procedures are well-reported in the literature.2,3,4,7 However, studies on presbyopia that assessed quality of life and freedom Ophthalmologyfrom spectacles are scarce, especially in developing countries.8
Aside from clinical parameters and functional tests of visual acuity, patient-reported outcomes are important in the comprehensive assessment of patients with ocular conditions. Quality of life assessments complement and enhance our understanding of patient’s visual status; thereby, supplementing clinical tests used for assessment.8 Several functional patient-reported outcome scales have been developed in recent years. However, the National Eye Institute Refractive Error Quality of Life (NEI-RQL) instrument is the most widely used because of its reliability and validity.9
This study compared the quality of life of presbyopic patients with non-surgical and surgical corrections using the NEI-RQL instrument. It specifically assessed the differences in quality of life outcomes in 40-60 year old patients with reading glasses and presbyopic LASIK and 60-80 year old patients with monofocal and multifocal IOLs. It also assessed the spectacle independence of patients who underwent presbyopic LASIK and those with multifocal implants.
Study patients were grouped according to age: 40-60 years comprised group 1 and 60-80 years group 2. Each group was further categorized according to their non-surgical and surgical presbyopia treatment. Group 1a included patients 40-60 years old with reading glasses. Group 1b included patients 40-60 years old with presbyopic LASIK correction. Group 2a included patients 60-80 years old with standard bilateral monofocal intraocular implants. Group 2b included patients 60-80 years old with bilateral multifocal intraocular implants.
Using the LaMorte sample size calculator, the estimated sample size for each group was 26 with the α value set at 0.05 and power equal to 95%. The sample size was calculated based on the study by McDonnell et al,10 wherein the mean difference in the NEI-RQL subscale clarity of vision had the minimum sample size requirement with the α value set at 0.05 & power of 95%. The mean score for the older age group was 80 with standard deviation of 10, and the mean score for the younger age group was 90 with standard deviation of 10.
The 42-item NEI-RQL has been validated and utilized in previous studies; hence, validation was not needed for this particular study. The study by Nichols et al9 determined that the NEI-RQL questionnaire had excellent reliability at 91% and good concurrent validity at 83%. After signing the informed consent, the patients filled up the self-administered NEI-RQL questionnaires. Although the questionnaires were self-administered, an ophthalmologist was on site to facilitate administration and guide the participants. The responses in the questionnaires were subsequently collated, analyzed, and compared between the subgroups in group 1 and group 2.
The NEI-RQL instrument included questions that assessed different subscales (Table 1). As detailed in the scoring manual,11 all items were scored so that a high score represented better quality of life. Each item was converted to a 0 to 100 possible range so that the lowest and highest possible scores were set at 0 and 100, respectively. In this format, scores represented the achieved percentage of the total possible score. For example, a score of 50 represented 50% of the highest possible score. Each of the 13 subscales comprised 1-7 items whose scores were averaged to yield a final score for each subscale.
The main outcome measures were NEI-RQL average score, NEI-RQL subscale scores, spectacle independence, uncorrected distance visual acuity (UDVA), and uncorrected near visual acuity (UNVA).
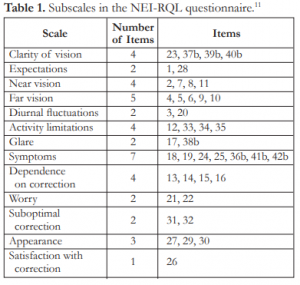
Table 1. Subscales in the NEI-RQL questionnaire.11
The demographic data and visual acuities were obtained from the patients’ medical records. NEI-RQL scores, spectacle-freedom responses, and patients’ satisfaction were compared within the groups. The study population was described using the frequency distribution, mean, and standard deviation. T-tests were used to compare differences in mean NEI-RQL and subscale scores of the subjects: 40-60 years old with reading glasses vs. 40-60 years old with unilateral or bilateral presbyopic LASIK correction, and 60-80 years old with standard bilateral monofocal intraocular implants vs. 60-80 years old with bilateral multifocal intraocular implants.
The study adhered to the tenets of the Declaration of Helsinki and approval was granted by the Institutional Ethics Review Committee.
RESULTS
A total of 150 patients who met the study’s inclusion criteria were able to complete the NEI-RQL questionnaire. Demographic characteristics in the 4 groups of study participants are shown in Table 2. The median age was 60 years (range 41 to 80 years); 93 (62%) were women. Basic refractive characteristics showed mean binocular UDVA of 20/32 or better in all 4 groups and mean binocular BDVA of 20/20 in all groups. The mean UNVA in subjects with presbyopic LASIK was J2, in subjects with multifocal IOLs J1, and in subjects with reading glasses including those with monofocal IOLs had J5 and J6 respectively.

Table 2. Demographic characteristics of study population (N=150).
UDVA=uncorrected distance visual acuity; BDVA=best-corrected distance visual acuity; UNVA=uncorrected near visual acuity; BNVA=best-corrected near visual acuity; D=diopters
Out of the 36 subjects who previously had presbyopic LASIK treatment, 25 (69%) could read J1+ (20/20), 7 (19%) J3 (20/40) or better independent of spectacles. The difference in the mean binocular UNVA of subjects (aged 41-59 years) with presbyopic LASIK treatment compared to subjects of similar ages with reading glasses was statistically significant (p=0.0012). The mean reading add requirement was significantly lower (p=0.0001) by 0.93D in the presbyopic LASIK group. However, the mean binocular BDVA of subjects with reading glass was significantly better (p=0.0038) compared to subjects who underwent presbyopic LASIK.
The difference in the mean binocular UDVA of subjects (aged 60-80 years) with monofocal and multifocal implants was not statistically significant (p=0.734). Subjects with multifocal implants had significantly better mean UNVA (p=0.0001). Out of 34 subjects with multifocal implants, 25 (74%) could read J1 (20/20), 6 (18%) J2 (20/30) independent of reading glasses. The reading add requirement was statistically lower (p=0.0001) by 2.3D in those with multifocal implants.
The mean NEI-RQL score and the 13 subscale scores for 47 subjects aged 41-59 years with reading glasses and 36 subjects aged 42-58 years with presbyopic LASIK treatment are shown in Table 3. The mean quality of life score exhibited no difference (p=0.191) between patients with reading glasses and those who underwent presbyopic LASIK. Subjects who underwent presbyopic LASIK had a higher subscale score for satisfaction than those of similar age with reading glasses; however, the difference was not significant (p=0.422). Statistically higher subscale scores for dependence on correction (p=0.0001) and appearance (p=0.0001) were achieved in patients with presbyopic LASIK. They also had poorer subscale scores for clarity of vision, far vision, diurnal fluctuations, symptoms, and glare (p=0.041)but all were not statistically significant except for glare.
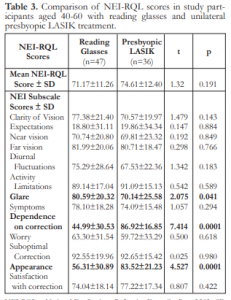
Table 3. Comparison of NEI-RQL scores in study participants aged 40-60 with reading glasses and unilateral presbyopic Lasik treatment.
NEI-RQL = National Eye Institute Refractive Error Quality of Life; SD = standard deviation
The mean NEI-RQL score and the 13 subscale scores for 33 subjects aged 60-80 years with monofocal implants and 34 subjects aged 60-80 years with multifocal implants are shown in Table 4. The mean quality of life score was significantly higher in patients with multifocal implants (p=0.006). Greater improvement in near vision (p=0.0006) and dependence on correction (p=0.0001) were achieved with multifocal implants. Subscale scores for worry (p=0.008), appearance (p=0.012) and satisfaction (p=0.036) were significantly better in those with multifocal implants. There was no statistical difference in glare scores (p=0.368). Subscale score for far vision was slightly higher in patients with monofocal implants but the difference was not significant (p=0.884).
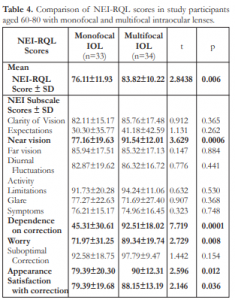
Table 4. Comparison of NEI-RQL scores in study participants aged 60-80 with monofocal and multifocal intraocular lenses.
NEI-RQL = National Eye Institute Refractive Error Quality of Life; SD = standard deviation
DISCUSSION
Previous studies have shown that presbyopia has a negative impact on vision-targeted health-related quality of life.10, 12 This association was strengthened by the finding that with increasing degree of presbyopia, subjects were more likely to fall into the group reporting the most difficulty, suggesting a dose-response relationship.8 There are several surgical strategies to correct presbyopia, including implantation of multifocal, accommodating or pseudoaccommodating intraocular lenses, for those with visually significant cataracts. From the wide range of intraocular lens options, multifocal IOLs have the advantage of providing functional vision at near, intermediate, and far distances. In recent developments, the cornea has been targeted to provide pseudoaccommodation in younger presbyopes. Presbyopic LASIK is one of the corneal approaches in treating presbyopia, wherein a multifocal corneal surface is created with the use of excimer laser ablation, thereby making a hyperpositive central cornea for near vision while leaving the mid-peripheral cornea for far vision.13 Therefore, presbyopic LASIK is a good option for young presbyopes who also require good distance vision correction. Well-established safety, efficacy, ease of surgery and availability of enhancement all make presbyopic LASIK an attractive option. Ultimately, these surgeries, whether lens-or corneal-based, are aimed at reducing near vision spectacle dependence in presbyopic patients.
In this study, we compared the quality of life of 40-60 year-old patients with reading glasses and presbyopic LASIK correction and in 60-80 year-old patients with monofocal and multifocal intraocular implants. Our data showed that presbyopic LASIK improved both UDVA and UNVA. The binocular BDVA (logMAR) of 0.03 (SD 0.06) was statistically different compared with the BDVA of 0.00 (SD 0.03) in the reading glass group (p=0.0038). Presbyopic LASIK decreased the reading add requirement by +1.00 D; thereby, decreasing spectacle dependence. Subjects who underwent presbyopic LASIK had a higher mean quality of life score; however, the difference was not statistically significant (p=0.191). Although they had less dependence on correction (p=0.0001) and perceived better appearance (p=0.0001), patient satisfaction (p=0.422) and perception of clarity of vision (p=0.143) were similar to those with reading glasses. The reduction in binocular BDVA in presbyopic LASIK patients might be due to higher experience of glare (p=0.041), dry eye symptoms (p=0.294), and diurnal fluctuations (p=0.183). Theoretical reasons for reduced BDVA included reduced light striking the retina from any focal length, thus reducing contrast sensitivity; pupil size reduction; the need for adaptation to the multifocal cornea; and dysfunctional tear syndrome.3
In older presbyopes with visually-significant cataracts, the implantation of multifocal intraocular lenses significantly improved UNVA (p=0.0001) com-pared to those with monofocal implants. Multifocal implants reduced the reading add requirement by 2.3 D, thereby providing spectacle independence. Subjects with multifocal implants had better mean quality of life score (p=0.006), better near vision (p=0.0006), less dependence on correction (p=0.0001), improvement in appearance (p=0.012), and higher patient satisfaction (p=0.036).
Previous studies have shown that patients have high preference and satisfaction with multifocal corrections.14 Our findings were consistent with previous published reports that implantation of multifocal IOL has a positive effect on the patient’s quality of life by improving reading performance.15 Cillino et al16 compared the visual outcomes, reading performance, and quality of life of working-age cataractous patients bilaterally implanted with 3 different diffractive multifocal intraocular lenses. In that study, the quality of life scores by the NEI-RQL instrument, photopic UNVA, distance-correctd near visual acuity (DCNVA), and corrected near visual acuity (CNVA) did not differ among the groups. The differences in reading acuity and maximum reading speed were exhibited under mesopic conditions. This evidence supported our findings that multifocal IOL implantation improved reading performance and quality of life.
In the study by Blaylock et al,17 refractive lens exchange with a multifocal IOL in presbyopic patients provided good visual function and better satisfaction compared to preoperative corrections. Slight reduction in contrast sensitivity function appeared to have no influence on quality of life.
Our data showed that higher quality of life scores were obtained with the NEI-RQL in younger subjects with presbyopic LASIK and in older pseudophakic subjects with multifocal intraocular implants. Uncorrected reading ability was very satisfactory, with 88% of subjects with presbyopic LASIK reading J3 or better and 92% of subjects with multifocal IOL reading J2 or better. Both procedures provided spectacle independence but with varying patient satisfaction. Patients with multifocal implants had higher satisfaction. Presbyopic LASIK patients experienced more glare and ocular surface symptoms which could have effected the diurnal fluctuations in vision, lower far vision and overall clarity of vision scores; hence, patient satisfaction and overall quality of life scores were comparable with the reading glasses group.
Based on MEI-RQL scores, we recommend presbyopic LASIK for younger qualified presbyopes who value functional and aesthetic spectacle independence but are cautious in assuring improvement in their vision-related quality of life due to consequential glare, ocular surface symptoms and a mild compromise in their far vision. On the other hand, in older presbyopes who aspire for better near vision and spectacle independence, the implantation of a multifocal intraocular implant has been shown to significantly improve their quality of life. However, patient expectations should be managed equally in all patients, whether with non-surgical or surgical presbyopia correction, since these patients have comparable demands and expectations.
The weakness of our study lay in the length of the questionnaire making it unappealing to some respondents. The Hawthorne effect (tendency of survey respondents to feel more positively about a topic due simply to the extra attention) and cognitive dissonance (a greater likelihood to have positive feelings about a result in an attempt to be consistent with and justify one’s choice in having surgery) should be considered18. For future studies, we recommended using a short-form version of the questionnaire and possible translation and validation of a Filipino version in order to widen population coverage.
In conclusion, presbyopic LASIK improved uncorrected near visual acuity and provided spectacle independence in presbyopes; however, quality of life and patient satisfaction were similar to those with reading glasses. Multifocal intraocular lenses significantly improved uncorrected near visual acuity, spectacle independence, and quality of life in pseudophakic patients with high patient satisfaction. Better perceived appearance seemed to be the greatest motivator to attain spectacle independence.
REFERENCES
1. Wubben T, Guerrero C, Salum M, et al. Presbyopia: A pilot investigation of the barriers and benefits of near visual acuity correction among a rural Filipino population. BMC Ophthalmology 2014;14:1-7.
2. Tabernero J, Schwarz C, Fernandez E, Artal P. Binocular visual simulation of a corneal inlay to increase depth of focus. Invest Ophthalmol Vis Sci 2011;52:5273-5277.
3. Ryan A, O’Keefe M. Corneal approach to hyperopic presbyopia treatment: six-month outcomes of a new multifocal excimerlaser-in-situ keratomileusis procedure. J Cataract Refract Surg 2013;39:1226-1233.
4. Chayet A, Barragan Garza E. Combined hydrogel inlay and laser-in-situ keratomileusis to compensate for presbyopia in hyperopic patients: one-year safety and efficacy. J Cataract Refract Surg 2013;39:1713-1721.
5. Census data and global changes in demographics. Available at www.census.gov/cgi-bin/broker. Accessed March 21, 2014.
6. Joy S, Frick K, Holden B, et al. The global burden of potential productivity loss from presbyopia. Invest Ophthalmol Vis Sci 2013;54:4545.
7. Alió JL, Chaubard JJ, Caliz A, et al. Correction of presbyopia by Technovision central multifocal LASIK (presby-LASIK). J Refract Surg 2006;22:453-460.
8. Patel I, Munoz B, Burke A, et al. Impact of presbyopia on quality of life in a rural African setting. Ophthalmology 2006;113:728-734.
9. Nichols JJ, Mitchell GL, Saracino M, et al. Reliability and validity of refractive error-specific quality of life instruments. Arch Ophthalmol 2003;121:1289-1296.
10. McDonnell PJ, Lee P, Spritzer K, et al. Associations of presbyopia with vision-targeted health-related quality of life. Arch Ophthalmol 2003;121:1577-1581.
11. Hays RD, Spritzer KL. National Eye Institute Refractive Error Quality of Life Instrument (NEI-RQL-42™), Version 1.0: A Manual for Use and Scoring. Los Angeles, CA. �(2002, February).
12. Luo BP, Brown GC, Luo SC, et al. The quality of life associated with presbyopia. Am J Ophthalmol 2008;145:618-622.
13. Epstein RL, Gurgos MA. Presbyopia treatment by monocular peripheral presbyLASIK. J Refract Surg 2009;25:516-523.
14. Richdale K, Mitchell GL, Zadnik K. Comparison of multifocal and monovision soft contact lens corrections in patients with low-astigmatic presbyopia. Optom Vis Sci 2006;83:266-273.
15. Alio JL, Plaza-Puche AB, Pinero DP, et al. Optical analysis, reading performance, and quality of life evaluation after implantation of a diffractive multifocal intraocular lens. J Cataract Refract Surg 2011;37:27-37.
16. Cillino G, Casuccio A, Pasti M, et al. Working-age cataract patients: visual results, reading performance, and quality of life with three diffractive multifocal intraocular lenses. Ophthalmology 2014;121:34-44.
17. Blaylock JF, Si Z, Aitchison S, et al. Visual function and change in quality of life after bilateral refractive lens exchange with the ReSTOR multifocal intraocular lens. J Refract Surg 2008;24:265-73.
18. Pasquali T, Smadja D, Savetsky M, et al. Long-term follow-up after laser vision correction in physicians: quality of life and patient satisfaction. J Cataract Refract Surg 2014;40:395-402.

