Suture-Related Corneal Abscess caused by Enterococcus casseliflavus following Complicated Phacoemulsification Surgery
Patricia Kaye T. Sy, MD, MBA, Karlo Marco D. Claudio, MD
Department of Ophthalmology, Quirino Memorial Medical Center, Quezon City, Philippines
Correspondence: Patricia Kaye T. Sy, MD, MBA
Office Address: Quirino Memorial Medical Center, JP Rizal cor P Tuazon, Project 4, Quezon City
Office Phone Number: +639178467750
Email Address: patriciakayesy2003@gmail.com
Disclosure: The authors report no conflict of interest.
Suture abscesses in the cornea following penetrating keratoplasty surgeries are well- documented, while those occurring after cataract surgery, especially phacoemulsification, are less frequently reported.1,2 Well-constructed, clear corneal incisions in phacoemulsification cataract surgery rarely require sutures to seal the wounds; however, they may be added according to the surgeon’s preference. These sutures may be susceptible to infections depending on certain circumstances. We report a case of Enterococcus casseliflavus suture abscess that developed 9 weeks after a complicated phacoemulsification surgery and the course of management.
CASE PRESENTATION
A 73-year-old woman underwent phacoemulsification surgery on her left eye during which zonulysis and vitreous prolapse into the anterior chamber were noted. A partial anterior vitrectomy was performed, a single-piece acrylic intraocular lens was implanted in the sulcus, and the corneal incisions were sutured with nylon 10-0 to reinforce wound closure. Uncorrected visual acuity on the first post-operative day was 20/20 and slit-lamp examination showed minimal anterior chamber inflammation, but the eye was otherwise unremarkable.
At 4 weeks post-operation, visual acuity was the same and the anterior segment inflammation had subsided. Removal of corneal sutures was done which was completed for the main port incision, but the suture at the side port incision prematurely broke and a fragment was left buried in the corneal stroma. No part of the fragment was left exposed and accessible; hence, no further attempts were done to retrieve the remaining suture. The patient was advised to consume the remaining topical medications and to follow-up as needed.
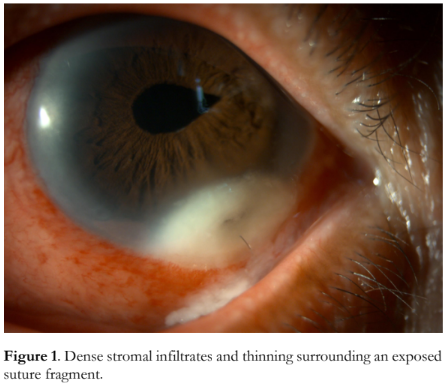
At 9 weeks post-operation, the patient returned to the clinic with a 3-day history of eye redness, tearing, mucoid discharge, blurred vision, and photophobia. She denied any trauma or eye manipulation. Best-corrected visual acuity deteriorated to 20/80. Gross examination revealed generalized conjunctival congestion with discharge at the inferior fornix. A 3.0 x 4.0 mm whitish corneal opacity with dense stromal infiltrates and a central area of ulceration was observed at the 5 o’clock limbal area surrounding an exposed suture fragment, with associated intense anterior chamber inflammation (Figure 1). The pupil was peaked at the 2 o’clock position but no distinct vitreous strand was seen, and the intraocular lens was stable in the sulcus.
The corneal opacity was diagnosed as a suture- related stromal abscess, and corneal scraping specimens were collected and sent for microbiological cultures. Empiric therapy was initiated with levofloxacin 1.5% eye drops (Oftaquix®, Santen Pharmaceutical Co., Ltd.) administered via (1) intrastromal injections in the normal areas of the cornea surrounding the abscess; (2) subconjunctival injection adjacent to the abscess; and (3) hourly topical drops while awake.
The culture results were released a week later and revealed a heavy growth of Enterococcus casseliflavus susceptible to tobramycin and ciprofloxacin. Tobramycin eye drops were added hourly alternating with levofloxacin and oral ciprofloxacin 500 mg twice a day was prescribed for one week.
Ten days after initiating treatment, there was a noticeable decrease in stromal infiltrates and resolution of the epithelial defect. However, there was still a localized area with significant amount of thinning appearing as an impending descemetocoele at the 5 to 6 o’clock midperipheral stroma (Figure 2). Topical antibiotics were continued at tapering frequency.

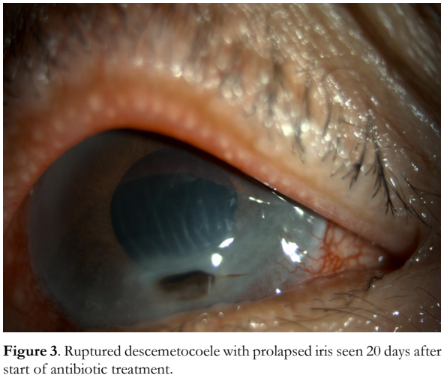
On the 20th day of treatment, the patient complained of sudden-onset worsening of vision after eye manipulation the day before. Uncorrected visual acuity had dropped to 20/400, and a 1.0 x 2.0 mm ruptured descemetocele surrounded by corneal scarring was seen. The anterior chamber was flat, and iris tissue was seen prolapsed into the corneal perforation (Figure 3).
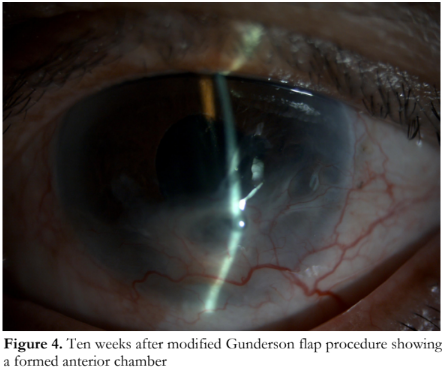
The corneal defect was deemed to be sterile at this point, and a modified Gunderson flap procedure was done to seal the perforation. The anterior chamber findings became stable after the surgery. On return visit 10 weeks after the flap procedure, uncorrected visual acuity was improved to 20/60, the anterior chamber was successfully reformed, and no further corneal thinning was observed (Figure 4).
DISCUSSION
A suture abscess is defined as a lesion composed of inflammatory stromal infiltrates found in direct contact with or adjacent to suture material. It is a known complication following penetrating keratoplasty, with incidence rates of 1 to 3.3%,3 but there are also reports in patients following cataract surgery done via extracapsular cataract extraction (ECCE) or phacoemulsification.
Suture abscesses associated with ECCE surgeries have been reported as late-onset complications. Cameron et al. reported a case of an 82-year-old man with a corneoscleral abscess 15 months after a routine extracapsular cataract extraction caused by Streptococcus pneumoniae.4 Mena et al. describe a similar abscess in a 47-year-old female 3 years post-ECCE.5
In reports of suture abscesses in phacoemulsification surgery, the onset of abscesses is more variable, ranging from as early as 1 week to as late as 3 years after surgery. Lee et al. presented a case series of 3 patients who underwent phacoemulsification with additional procedures (trabeculectomy and pars plana vitrectomy). The onset of abscess ranged from 9 weeks to 33 months, with the infections occurring after suture removal.6
Kehdi et al. reported 5 patients who developed wound infections even after uneventful clear corneal cataract surgery, presenting from a few days to several weeks post-operatively.7 Our reported case is consistent with the relatively earlier onset seen in phacoemulsification surgeries, and was associated with suture removal. A suture located in the avascular clear cornea, compounded by the incomplete suture removal, may have served as a nidus for opportunistic bacterial infiltration when the prophylactic antibiotics after cataract surgery were discontinued.
Culture isolates from suture abscess cases following cataract surgeries vary, with Streptococcus pneumoniae, Pseudomonas aeruginosa, Aspergillus, and different Staphylococcus species being the commonly reported organisms.7-9 Most of the organisms reported were from the normal flora of the conjunctiva and eyelids. The isolate found in our case, Enterococcus casseliflavus, is known to cause opportunistic infections and has been previously documented to cause trauma-related endophthalmitis.10,11 There have been, however, no previous reports of Enterococcus casseliflavus causing suture-related corneal abscess in post-phacoemulsification surgery.
The outcome of treatment for suture abscess is also variable, with some abscesses resolving with empiric topical antibiotic therapy, and others needing surgery such as lamellar keratectomy and conjunctival flaps to repair perforations. Topical, subconjunctival, intravitreal, and systemic antibiotics have been used for treatment depending on the extent of involvement.8,11,12 In our case, administration of antibiotics was focused in the anterior segment and supported by oral medication. Despite initial success in containing the infection as evidenced by the resolution of the stromal infiltrates and anterior chamber inflammation, the residual thinning and eventual perforation necessitated surgical repair.
Stromal injections have been documented for use in fungal keratitis, with amphotericin B and voriconazole as the commonly administered antifungal drugs.13 There is also increasing evidence of the use of the intrastromal technique in treating bacterial keratitis, although formal practice guidelines have yet to be developed.14 Published reports describe stromal injection procedures using a 30-gauge needle to administer the medication directly into the abscess and surrounding areas, with the level of corneal hydration used as a reference for the amount of medicine administered. This procedure may be repeated with at least a 72-hour interval between injections.15
In our patient, a similar approach was used with the 1.5% levofloxacin eye drops, but no injection was made directly to the abscess, since there was significant thinning at the initial presentation. Injections were instead done in the surrounding clear cornea which was structurally more stable, with the endpoint of creating visible stromal hydration completely surrounding the abscess borders. A subconjunctival injection was added to cover the limbal side of the lesion. Only one round of injections was done since there was significant resolution of the stromal infiltration after 10 days of culture-guided topical and oral antibiotics.
In conclusion, we reported a novel case of suture- related corneal abscess caused by Enterococcus casseliflavus in a post-phacoemulsification eye with a retained broken suture. The stromal abscess resolved with the combination of empiric treatment with levofloxacin 1.5% stromal and perilesional subconjunctival injections, and culture-guided topical and oral antibiotics. Despite efforts to control the infection medically, the resultant thinning and perforation of the cornea warranted surgical repair with a modified Gunderson flap.
REFERENCES
- Christo CG, van Rooij J, Geerards AJ, et al. Suture-related complications following keratoplasty: a 5-year retrospective study. Cornea. 2001;20(8):816-819.
- Hood CT, Lee BJ, Jeng BH. Incidence, occurrence rate, and characteristics of suture-related corneal infections after penetrating keratoplasty. Cornea. 2011;30(6):624-628.
- Mannis MJ, Holland EJ. Cornea. Fundamentals, Diagnosis and Management, 5th ed. Vol. 1. London: Elsevier Health Sciences; 2021; 1217-1218.
- Cameron JA, Huaman A. Corneoscleral abscess resulting from a broken suture after cataract surgery. J Cataract Refract Surg. 1994;20(1):82-83.
- Mena WG. Suture associated corneal abscess three years after cataract surgery: a case report. South Sudan Medical Journal. 2014;7(12):66-67.
- Lee BJ, Smith SD, Jeng BH. Suture-related corneal infections after clear corneal cataract surgery. J Cataract Refract Surg. 2009;35(5):939-942.
- Kehdi EE, Watson SL, Francis IC, et al. Spectrum of clear corneal incision cataract wound infection. J Cataract Refract Surg. 2005;31(9):1702-1706.
- Cosar CB, Cohen EJ, Rapuano CJ, Laibson PR. Clear corneal wound infection after phacoemulsification. Arch Ophthalmol. 2001;119(12):1755-1759.
- Valenton M. Wound infection after cataract surgery. Jpn J Ophthalmol. 1996;40(3):447-455.
- Berenger BM, Kulkarni S, Hinz BJ, Forgie SE. Exogenous endophthalmitis caused by Enterococcus casseliflavus: A case report and discussion regarding treatment of intraocular infection with vancomycin-resistant enterococci. Can J Infect Dis Med Microbiol. 2015;26(6):330-332.
- Yoshino Y. Enterococcus casseliflavus infection: a review of clinical features and Treatment. Infect Drug Resist. 2023 Jan 20;16:363-368
- Confino J, Brown SI. Bacterial endophthalmitis associated with exposed monofilament sutures following corneal transplantation. Am J Ophthalmol. 1985;99(2):111-113.
- Hu J, Zhang J, Li Y, et al. A combination of intrastromal and intracameral injections of Amphotericin B in the treatment of severe fungal keratitis. J Ophthalmol. 2016;2016:3436415.
- El Shabrawy RM, Saed A. Experimental Intrastromal Antibiotic Injection for Refractory Keratits Caused by Biofilm Forming Pseudomonas Aeruginosa. Egyptian Journal of Medical Microbiology. 2016;25(1):133-140.
- Sharma N, Sahay P, Maharana PK, et al. Management Algorithm for Fungal Keratitis: The TST (Topical, Systemic, and Targeted Therapy) Protocol. Cornea. 2019;38(2):141-145.

