Silicone-oil removal using a 20-gauge infusion cannula
Harvey S. Uy, MD
SILICONE-oil tamponade is widely used for the treatment of retinal detachment and macular holes. Because prolonged intraocular silicone-oil retention may cause sight-threatening complications such as keratopathy, glaucoma, hypotony, and perisilicone-oil fibrosis, silicone oil should be removed once its tamponade effect is no longer necessary. 1-4 Active drainage techniques utilize a vitrectomy machine to suction silicone oil from the vitreous cavity while passive drainage uses a stream of water to float silicone oil out through an oversized limbal, pars plana, or corneal incision. 5-8 While passive drainage avoids high suction pressures that may lead to retinal traction or redetachment, the prolonged use of surgical instrumentation to retract the drainage incision may traumatize the wound edges and lead to wound leak, hypotony, pain, scleral melt, or infection. We conducted this study to assess the safety and efficacy of a passive silicone-oil removal through a self-retaining cannula inserted into the pars plana.
METHODOLOGY
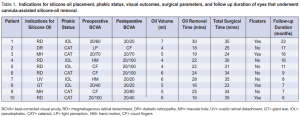
Ten phakic or pseudophakic eyes underwent removal of low-viscosity silicone oil (Oxane 1300 centistokes, Bausch and Lomb, Rochester, New York). The indications for silicone-oil tamponade and phakic status are shown in Table 1. The mean injected silicone-oil volume was 5.2 ± 1.0 ml (range, 4 to 7).
Surgical Technique
Local anesthesia with intravenous sedation was used. After making conjunctival incisions, a 20-gauge, 4-mm infusion cannula, connected to a 500-ml bottle of balanced saline, was inserted through an inferotemporal, pars plana, stab incision and anchored using vicryl 7-0 sutures. An MVR blade was then used to create a superotemporal pars plana sclerotomy through which a standard 20-gauge 4- mm infusion cannula, which had been previously disconnected from its tubing, was inserted. The infusion-bottle height was then raised to 3 feet and the infusion line opened. Silicone oil was allowed to drain out through the self-retaining cannula until a gush of fluid was visualized from its tip (Figure 1).
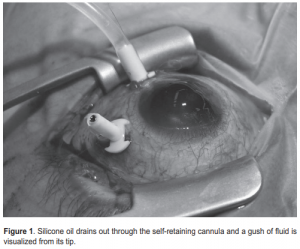
The infusion cannula was then removed and the superotemporal incision enlarged to 2 mm using a 15-degree blade. The incision was held open with 0.12 toothed forceps for 2 minutes to drain the remaining silicone oil. The incision was then plugged. Indirect ophthalmoscopy was done to confirm no remaining silicone oil. The incisions were closed with vicryl 7-0. The silicone-oil removal time was measured using a stopwatch set from the moment the drainage cannula was inserted and a gush of fluid was observed. During each postoperative examination, the following data were recorded: presence of floaters, best-corrected visual acuity (BCVA), intraocular pressure (IOP), and results of dilated-fundus examination. Descriptive statistics are reported. Informed consent was obtained from all patients. The study protocol was approved by the Asian Eye Institute ethics committee.
RESULTS
Nine of the 10 eyes (90%) experienced improvement in BCVA from preoperative levels. The mean silicone-oil removal time was 22.0 ± 4.8 minutes (range, 16 to 30); the mean total surgical duration was 29.6 ± 4.9 minutes (range, 24 to 35). The mean silicone-oil flow rate was 0.24 ml/minute (Table 1). Four patients (40%) reported postoperative floaters. There were no cases of keratopathy, wound leak, hypotony, retinal detachment, uveitis, or suture-related complications. The mean follow-up period after silicone-oil removal was 12.0 ± 5.7 months (range, 6 to 23).
DISCUSSION
Our technique of silicone-oil removal differs from the practice of creating an oversized pars plana incision held open with forceps until complete silicone-oil removal. Instead, a readily available, self-retaining extrusion cannula, inserted through a regular-sized incision, served as the conduit for silicone-oil egress. This method is less traumatic for the patient and less stressful for the surgeon. The advantages of this cannula-assisted technique include: (1) less work for surgeons because the surgeon is freed from holding the wound edges open during most of the surgery; (2) less risk for wound maceration, potentially improving wound closure and preventing wound leaks, hypotony, and infection; (3) less surgical trauma as only 2 sclerotomies are needed; (4) less risk for retinal phototoxicity because the surgical microscope light can be turned off during this automated process; (5) less risk for corneal endothelial damage because removal through the pars plana route avoids anterior-chamber turbulence. 9 Compared to active drainage techniques, passive drainage techniques lessen the risk of retinal traction resulting from high-suction pressures. Addition of a third
1. Casswell AG, Gregor ZJ. Silicone-oil removal: The effect on the complications of silicone oil. Br J Ophthalmol 1987; 71: 893-897.
2. Hutton WL, Azen SP, Blumenkranz MS, et al. The effects of silicone-oil removal: Silicone Study Report 6. Arch Ophthalmol 1994; 112: 778-785.
3. Falkner CI, Binder S, Kruger A. Outcome after silicone-oil removal. Br J Ophthalmol 2001; 85: 1324-1327.
4. Silicone Study Group: Silicone Study Report 4. Postoperative intraocular-pressure abnormalities in the silicone study: results of a randomized clinical trial. Ophthalmology 1993; 100: 1629-1635.
5. Fletcher ME, Peyman GA. A simplified technique for the removal of liquid silicone from vitrectomized eyes. Retina 1985; 5: 168-171.
6. Zilis JD, McCuen BW, de Juan E, et al. Results of silicone-oil removal in advanced proliferative vitreoretinopathy. Am J Ophthalmol 1989; 108: 15-21.
7. Assi A, Woodruff S, Gotzaridis E, et al. Combined phacoemulsification and transpupillary drainage of silicone oil: results and complications. Br J Ophthalmol 2001; 85: 942-945.
8. Garodia VK, Kulkarni A. Silicone-oil removal using vitrectomy machine: a simple and safe technique. Retina 2001; 21: 685-687.
9. Boscia F, Cardascia N, Sborgia L, et al. Evaluation of corneal damage by combined phacoemulsification and passive efflux of silicone oil in vitrectomized eyes. J Cataract Refract Surg 2003; 29: 1120-1126.
10. Qin B, Zhao Tieying Z, Huang L. Removal of silicone oil from aphakia: use of a selfsealing corneal incision. Am J Ophthalmol 2004; 138: 1055-1057.scleral incision for posterior-segment manipulation can be easily done in case of need for additional surgical procedures. The only complications in this series were postoperative floaters; however, the incidence of floaters reported here is less than in other studies. 10 Finally, operating costs are reduced because a vitrectomy machine is not utilized. The main disadvantage of this technique compared to active drainage procedures is potentially longer oilremoval and surgical time. However, the surgical time achieved here seems comparable to those reported in other studies that utilized passive drainage procedures. 10 One of the limitations of this study is the lack of comparison with a control group where silicone oil is passively removed without the use of an extrusion cannula. The effectiveness of this technique for aphakic eyes or eyes that received higher-viscosity silicone oil was also not determined. These are areas for future research. In conclusion, low viscosity silicone oil can be successfully and safely removed from phakic or pseudophakic eyes using a standard 20-gauge, self-retaining extrusion cannula inserted through the pars plana. This technique facilitates silicone-oil removal and reduces surgical trauma.

