Retinopathy in a patient with systemic lupus erythematosus
Franz Marie Cruz, MD, Ildefonso Chan, MD, Cherica Tee, MD, Carien Gulay, MD, Leonila Dans, MD, Jennifer Otadoy-Agustin, MD, Marysia Recto, MD
SYSTEMIC lupus erythematosus (SLE) is an autoimmune disease of unknown cause. It is a multisystemic disease that may affect almost all organ systems, including the joints, skin and mucous membranes, heart, kidneys,
and the central nervous system. Retinopathy associated with SLE is well described in medical literature. It is characterized as a microangiopathic disease with small-vessel occlusion resulting in multiple infarctions of the retinalnerve-fiber layer, giving a Purtscher-like appearance. However, a more severe form of SLE retinopathy has been reported in patients with antiphospholipid antibody. This rare form of retinopathy is associated with poor visual outcome and high risk of neovascularization and vitreous hemorrhage in as much as 40% of cases.1 Anticoagulation plays a major role in the secondary prevention of thrombosis in the presence of antiphospholipid antibodies. We report a case of severe SLE retinopathy in a pediatric patient who also had elevated levels of antiphospholipid antibody.
CASE REPORT
A 16-year-old female developed high-grade fever associated with blurring of vision. She was admitted for 9
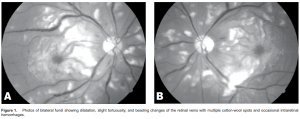
days in a local hospital and given intravenous antibiotics. Complete blood count showed leukopenia and anemia. She was discharged afebrile but noted “seeing red spots in her central vision.” She was brought to a private ophthalmologist who requested a fluorescein angiogram. Color photos of the fundus of both eyes showed dilatation, tortuousity, and beading changes of the retinal veins. There were numerous cotton-wool spots and occasional intraretinal hemorrhages (Figure 1). Fluorescein angiography revealed nonfilling of many retinal-end arterioles including those supplying the macula, and wide areas of capillary nonperfusion. Ischemic maculopathy was entertained and a collagen disease, specifically SLE, was suspected as the primary underlying condition. She was started on prednisone at 0.5mg/kg/day given for 2 months. The patient later consulted at the Medical Retina Clinic

of the Department of Ophthalmology and Visual Sciences of the University of the Philippines–Philippine General Hospital. Her best-corrected visual acuity was reduced to 20/100 in the right eye and 20/200 in the left. The anterior segment of both eyes was normal. Examination of both fundi revealed resolution of the cotton-wool spots and decrease in the venous dilatation and tortuosity. These were replaced with fibroproliferative membranes along the arcades (Figure 2A). In addition, a patch of preretinal hemorrhage was seen at the superonasal midperiphery of the left fundus (Figure 2B). A repeat angiogram revealed delayed filling of retinal arterioles, wide areas of capillary nonperfusion, telangiectatic vessels, and microaneurysms, indicating ischemic retinopathy with membranoproliferative changes probably secondary to SLE. The patient was further referred to a pediatric rheumatologist who noted malar rash and oral ulcers. Antinuclear antibody determination showed +4 (titer 1:80) with speckled pattern and elevated levels of anticardiolipin antibodies (ACA) IgM 12.6 (N <12.5 GPL) and ACA IgG 16.9 (N<15 GPL). The diagnosis of SLE was made based on the American College of Rheumatology 1997 revised criteria. High-dose systemic steroid (prednisone at 1 mg/kg/day) was resumed. With the etiology of the ischemic retinopathy fully established, panretinal photocoagulation was performed. A repeat angiogram 3 months after treatment completion revealed residual neovascularization in the right fundus and presence of vitreous hemorrhage inferiorly in the left. The patient was scheduled for laser augmentation of both retinas, but was lost to follow-up. She returned 6 months
later after experiencing a sudden drop in vision of the left eye. On examination, vision of the left eye was diminished to hand movement due to the dense vitreous hemorrhage. She was advised vitrectomy.
A second determination of anticardiolipin antibodies showed further elevation of ACA IgG to 21.20 GPL. Given
that the patient presented with ischemic retinopathy secondary to small-vessel occlusion and that ACA IgG and IgM levels were persistently elevated, the diagnosis of antiphospholid antibody syndrome (APAS) was considered. Patient was worked up for other sites of thrombosis including the carotid arteries, heart, and lower- extremity arteries and veins but findings were all negative. As prophylaxis for future thrombotic episodes, she was started on an anticoagulant (aspirin). Vitrectomy was temporarily deferred while she was receiving anticoagulation therapy. Due to the persistent SLE activity causing vision loss, methylprednisolone pulse therapy was suggested, in addition to maintaining her on high-dose prednisone to improve vision and observe the ophthalmologic findings in response to the steroid treatment. She was also prepared for vitrectomy after the anticoagulant was withdrawn. Regular follow-up to reassess the need for future anticoagulation was advised.
DISCUSSION
Retinopathy is a well-known complication of SLE, although retinopathy associated with SLE is not included
in the 1982 revised criteria of the American College of Rheumatology universally used today for the diagnosis of SLE. In a local study by Lising et al., the prevalence of retinopathy among SLE patients was found to be 16.7%.2 Retinopathy associated with SLE is most commonly characterized by the presence of multiple cotton-wool spots which may be associated with intraretinal hemorrhages and/or vasculitis. The underlying disease
involves immune complex formation leading to microvascular occlusions and infarction of the retinalnerve fiber. This form of retinopathy is reversible with systemic steroid and carries good visual-acuity prognosis.
A more severe form of SLE retinopathy has also been reported. The process is generally one of diffuse arteriolar occlusion with extensive capillary nonperfusion. After extensive ischemia, neovascularization may develop with possible resultant vitreous hemorrhage or fibroproliferative membranes causing traction retinal detachment. This form of SLE retinopathy, although rare, harbors a much poorer vision prognosis.
For the past 2 decades, the presence of antiphospholipid antibodies in SLE patients has been associated with
the more severe form of retinopathy. Antiphospholipid antibodies represent a heterogeneous group of antibodies against phospholipids binding proteins or their complexes with anionic phospholipids.4 The prevalence of antiphospholipid antibodies in children with SLE is 63.2 to 75.4%.5 Isolated or in association with a systemic disease such as SLE, elevated levels of antiphospholipid antibodies predispose patients to arterial and venous thrombosis in which the retinal and choroidal vasculatures are not spared. Ocular features of this disease include vasoocclusive retinopathy, papillitis, serous retinal detachment, vitritis, and iritis.1 Systemically, patients with high levels of antiphospholipid antibodies may present with recurrent deep-venous thromboses, pulmonary emboli, transient ischemic attacks, hemiparesis, and thrombocytopenia. Thediagnosis of antiphospholipid antibody syndrome in the pediatric population is made if at least one of the clinical criteria (presence of vascular thrombosis in any tissue or organ) and one of the laboratory criteria (significant
elevation of lupus anticoagulant or antocardiolipin antibody on 2 or more occasions at least 12 weeks apart)
are met. Presence of antiphospholipid antibodies necessitates anticoagulation therapy to prevent thrombotic
episodes. Evidence shows that recurrent thrombotic episodes and progression of vasoocclusive retinopathy
were less common in patients who received anticoagulants.3 Distinctive about this case was the otherwise good health status of the patient who only presented with bilateral diffuse vasoocclusive ischemic retinopathy. Even without the systemic complications associated with high levels of ACA, anticoagulation was already started. It is recognized that ocular disease may manifest earlier than the more severe systemic complications of the disease.3 Thus, prophylaxis with anticoagulants and regular followup are warranted. In conclusion, diffuse vasoocclusive ischemic retinopathy is one of the ocular complications of SLE, which has been associated with presence of antiphospholipid antibodies. These antibodies also predispose one to thrombosis formation in other organs with life-threatening consequences. Thus, prophylaxis with anticoagulation is key in its management. It is important, therefore, in this type of severe SLE retinopathy to screen for antiphospholipid antibodies as well.
References
1. Au A, O’Day J. Review of severe vasoocclusive retinopathy in systemic lupus erythematosus and the antiphospholipid syndrome: associations, visual outcomes, complications and treatment. Clin Exp Ophthalmol 2004; 32: 87-100.
2. Lising RS, Remulla JC, Cubillan LP, et al. Association of ocular manifestation and disease activity among Filipinos with systemic lupus erythematosus. Philipp J Ophthalmol 2004; 29: 17-20.
3. Ushiyama O, Ushiyama K, Koarada S, et al. Retinal disease in patients with systemic lupus erythematosus. Ann Rheum Dis 2000; 59: 705-708.
4. Campos LMA, Kiss MH, D’Amiro ÉA, Almeida Silva CA. Antiphospholipid antibodies in 57 children and adolescents with systemic lupus erythematosus. Rev Hosp Clin Fec Med S Paulo 2003; 58: 157-162.
5. Miserocchi E, Baltatzis S, Foster S. Ocular features associated with anticardiolipin antibodies: a descriptive study. Am J Ophthalmol 2001; 131:451-456.

