Prognostic Value of a Classification and Regression Tree Model in Patients with Open-Globe Injuries
Danica T. Esteban, MD1,2, Karlo Marco D. Claudio, MD1, Cheryl A. Arcinue, MD1
1Department of Ophthalmology, Rizal Medical Center, Pasig City, Philippines
2Department of Ophthalmology, Southern Isabela Medical Center, Santiago City, Philippines
Correspondence: Danica Tomas-Esteban, MD
Clinic Address: Department of Ophthalmology, Rizal Medical Center, Pasig City, Philippines
Clinic Phone Number: +639272335051
Email Address: estebandanix@gmail.com
Disclosure: The authors report no conflict of interest.
Although ocular trauma comprises a minor proportion of ophthalmology consults, it has a devastating outcome and is one of the most common causes of acquired blindness. In a study published by the Department of Health (DOH) Eye Center in 2018, the 5-year proportion of open globe injuries was 7.3 cases per 1000 new patients. Among these patients, 6.5% presented with vision of no light perception (NLP) at initial consult, 0.9% underwent enucleation, and 27.7% had a final visual acuity <20/200 for those with at least 1 month follow-up after all interventions were done.1 Quality of life studies in ocular trauma patients showed that most report significant pain and discomfort, difficulty in performing routine activities, and anxiety and depression after sustaining visually-disabling ocular injuries in as early as the first visit.2
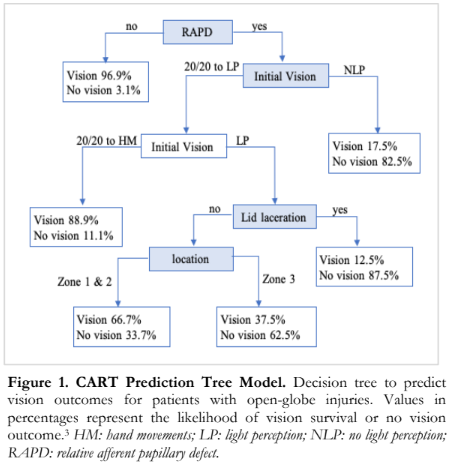
Management of ocular injuries has improved due to the emergence of standardized classification systems and tools for evaluating visual recovery. The Birmingham Eye Trauma Terminology (BETT) differentiates between open and closed globe injuries and further categorizes open injuries into four groups: rupture, intraocular foreign body (IOFB), perforating, and penetrating injury. Tools such as the Ocular Trauma Score (OTS) and the Classification and Regression Tree (CART) Model (Figure 1) are used to predict chances of visual recovery based on the nature and extent of trauma.3,4,5 These systems enable ophthalmologists to better diagnose and manage cases by serving as guides for individualized treatment decisions and visual prognostication.
The CART model is a validated tool for determining the visual prognosis of open-globe injuries with studies showing accurate predictive outcomes.4,5 There is, however, no published data regarding the application of this prognosticating tool in Filipino patients. The purpose of this study was to evaluate the diagnostic accuracy of the CART model in predicting visual recovery among open-globe trauma patients in a local tertiary hospital setting.
METHODS
This was a retrospective, single-center, hospital- based, cohort study which included patients with open-globe injuries at the Rizal Medical Center (RMC) from January 2019 to December 2020. The study was approved by the institutional review board of the hospital.
Eyes diagnosed with open-globe injuries with at least one-month follow-up were included in the study. Patients with incomplete medical records, children belonging in the preverbal age group, those who had any ocular disease or ocular surgery unrelated to the injury that can confound visual outcome, ocular injuries which cannot be classified according to the BETT system, patients discharged against medical advice, cases initially managed at a different institution, and patients lost to follow-up were excluded.
Purposive sampling of in- and out-patient medical records was done by searching the hospital electronic patient database using the following keywords: “penetrating eye injury”, “enucleation”, “evisceration”, “intraocular foreign body”, “perforating injury”, and “ruptured globe”. The records retrieved were screened based on the inclusion and exclusion criteria, then data collection was done using a three-part patient data form to extract the following information: demographics (age, gender, laterality of affected eye, place of injury, mechanism of injury, duration between injury and management), clinical profile (extent of injury, visual acuity, management done, complications), and visual outcome (actual and CART-predicted). The type of open-globe injury was classified according to the BETT system.6 Final visual outcome was defined as the visual acuity at the most recent out-patient clinic visit at least one month from the date of injury, and was stratified as follows: good (6/12 or better), fair (6/18 to 6/60), poor (<6/60 to counting fingers), worst (<light perception, light projection, post- enucleation or post-evisceration). Predicted visual outcome was determined using the algorithm from the CART model and reported as either “vision” (defined as final visual acuity of hand movement or better) or “no vision” (defined as final visual acuity of no light perception including those that underwent enucleation or evisceration).
Statistical Analysis
Descriptive statistics such as frequency and percentage were used for categorical data. The diagnostic accuracy of the CART model was determined by computing for sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). The area under the receiver operating characteristic curve (AUC) was calculated to check the discriminatory capability of the CART model. Level of significance was set at 5%. All calculations were done using MedCalc® Statistical Software version 22.021 (MedCalc Software Ltd, Ostend, Belgium, 2024).
RESULTS
A total of 65 eyes of 65 patients were included in the study, and patient demographic data are summarized in Table 1. Majority were male patients (81.5%) and belonged to the 17 to 39 year age group (40%). All had monocular involvement with almost equal involvement of the right and left eye (47.6 vs 52.3%, respectively). Based on the BETT system, 58 eyes (89%) had penetrating eye injury, 2 (3%) had globe rupture, and 5 (8%) had IOFB. None had perforating injury.
Table 2 shows the management and rates of complications stratified according to visual outcome. All eyes underwent at least one surgical procedure, and 4 eyes underwent combined anterior and posterior segment repair. No eye received medical management alone. The most common type of surgical procedures performed were anterior segment repair in 52 eyes (80%) and enucleation in 8 (12%). Majority of eyes (48%) had poor visual outcome and 14% had worst outcome, while 18% and 20% had good and fair vision, respectively. The most common complications were secondary cataract (22%), increased intraocular pressure (15%), aphakia (9%), and retinal detachment (9%) across all patients. Among patients with fair to worst visual outcome, some eyes were noted to have more than one complication. Endophthalmitis was the most common complication (33%) seen among patients with worst visual outcome.
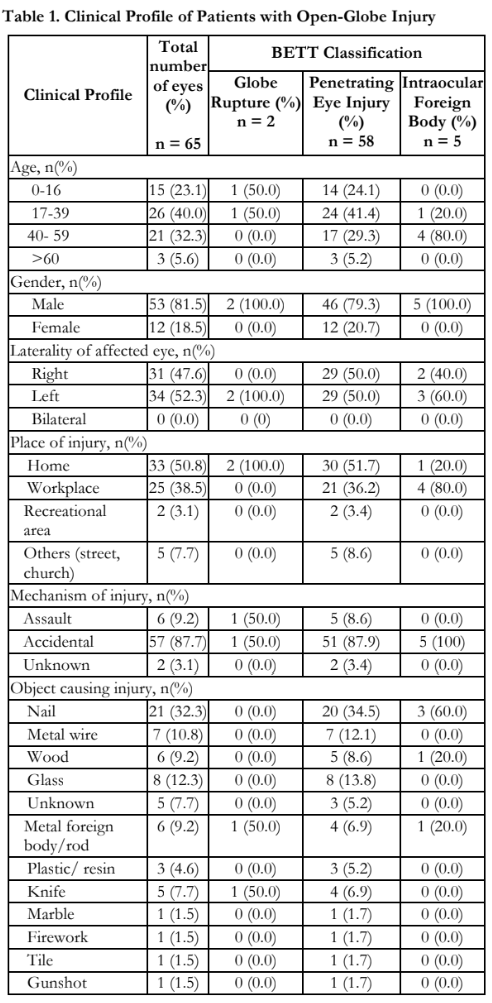
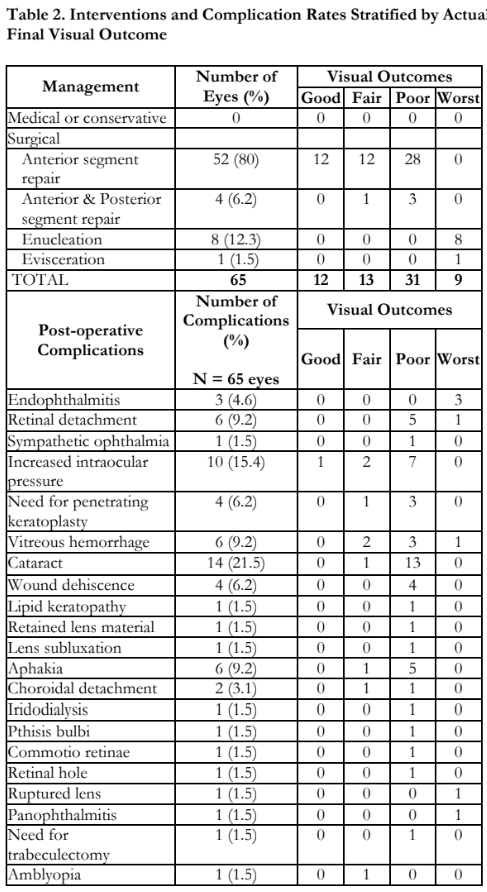
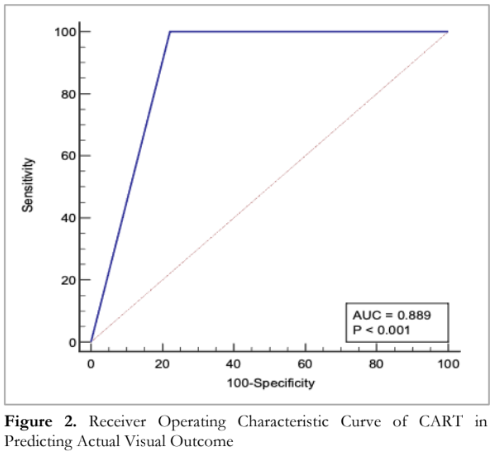
Table 3 shows the CART predictions of visual outcome compared to the actual visual outcome. Sensitivity and NPV were both 100%, while specificity and PPV were 77.8% and 96.5% respectively; overall accuracy was very high at 96.9% (95% CI 89.3 to 99.6%). AUC was 0.89 (95% CI 0.79 to 0.95, p< 0.001), which indicates that CART can significantly discriminate vision survival from no vision (Figure 2).
DISCUSSION
Based on the data from this study, open-globe injuries were more common among adult males in the working age group, and majority were accidental in nature. These findings are similar to published data from local ocular trauma studies.1,7 A notable difference, however, is that injuries occurred more frequently at the workplace in previous studies, while our data points to the home as the most common place of injury. This shift in location is probably an effect of enforced lockdowns during the COVID-19 pandemic, which resulted in more people staying at home in the latter half of the study period.

Despite the changing trend in place of injury, the mechanisms for visual loss remain the same. In this study, penetrating eye injuries (89%) were the most common type of ocular trauma. The most common complications resulting in poor vision even after treatment were cataract and increased intraocular pressure (42% and 23% of eyes with poor visual outcomes, respectively) and endophthalmitis (33% of eyes with worst visual outcomes), which are consistent with previous reports.1,7,8
Applying the CART model in this cohort showed favorable discriminating capability in predicting vision survival with sensitivity at 100%, specificity at 77.8%, and overall accuracy at 96.9%. This study was comparable to previous studies using the CART model for prognostication, which showed sensitivity ranging from 85.7% to 97.7% and specificity ranging from 73.95% to 91.9%.3,4,5 Although the Ocular Trauma Score (OTS) had a higher prognostic accuracy compared to CART in a head-to-head analysis, the results from this study suggest that using the CART in the local setting is a viable option for prognosticating open-globe injuries.3 Initial vision at presentation, presence of relative afferent pupillary defect, adnexal injury, and zone of injury are the main factors for visual outcome considered in the CART, and results from this study are indicative that these factors hold similar prognostic weight in assessing outcomes in local cases.
The limitations of the study were its retrospective nature, small sample size, single-center population, and limited study duration. It is recommended to explore the utility of the CART model in a large, prospective, multi-center study and its applicability to other types of ocular trauma aside from open-globe injuries.
In summary, the CART model showed high accuracy in discriminating vision survival from no vision among Filipino patients with open-globe injuries. Given its utility as a prognosticating tool for visual outcomes, it may be used to guide treatment decisions for open-globe injuries in the local setting.
ACKNOWLEDGEMENT
The authors thank Mr. Reginald Arimado for his invaluable assistance with the statistical computations.
REFERENCES
- Aquino J, Jimenez MS, Jacoba CM, Medalle RS. Demographics and Clinical Characteristics of Open-Globe Ocular Trauma at a Tertiary Eye Center in the Philippines: A 5-Year Retrospective Review. W J Ophthalmol & Vision Res. 2020;3(2).
- Artiaga JCM, Lim Bon Siong R. Quality of Life After Ocular Trauma: A Prospective, Longitudinal, Questionnaire- Based Study in a Tertiary Hospital in the Philippines. Philipp J Ophthalmol. 2019;44:59-67.
- Man C, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models—the Ocular Trauma Score and the Classification and Regression Tree. Eye. 2010; 24: 84-89.
- Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision Survival after Open Globe Injury Predicted by Classification and Regression Tree Analysis. Ophthalmology. 2008;115(1):202–9.
- Mekhasingharak N, Namatra C. Classification and regression tree analysis for predicting visual outcome after open-globe injuries in Siriraj Hospital. J Med Assoc Thai. 2014 Sep;97(9):939-46. P
- Kuhn F, Morris R, Witherspoon C. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmol Clin N Am. 2002 Jun;15(2):139–43.
- Regalado RNC, Lim Bon Siong R, Agahan ALD, Felipe AF. Prognostic Value of the Ocular Trauma Score in Traumatic Open Globe Injuries in the Philippines: A Five-Year Retrospective Study —Prognostic Value of the Ocular Trauma Score in Open Globe Injuries. Open Access Library Journal. 2018;5(01):1–12.
- Gupta R, Gupta S, Chauhan L. Predicting visual outcome after open globe injury using classification and regression tree model: the Moradabad ocular trauma study. Canadian J Ophthalmol. 2019;54(4):473–8.

