Prevalence of Dry Eye Disease in a Community in Baguio City
Ruben Lim Bon Siong, MD1,2, Jayvee S. Rivera, MD1, Carlo Leandro R. Igama, MD1,3
1Department of Ophthalmology and Visual Sciences, University of the Philippines Manila-Philippine General Hospital, Manila, Philippines
2Eye Institute, St. Luke’s Medical Center, Quezon City, Philippines
3Baguio General Hospital and Medical Center, Baguio City, Philippines
Correspondence: Ruben Lim Bon Siong, MD
Office Address: Department of Ophthalmology and Visual Sciences, Philippine General Hospital, University of the Philippines Manila, Taft Avenue, Ermita, Manila, Philippines
Office Phone Number: +63285548400 local 8502
Email Address: rlimbonsiong@up.edu.ph
Disclosure: The authors report no conflict of interest.
Dry eye disease (DED) is a major ophthalmological health problem globally. As defined by the consensus report of the Asia Dry Eye Society (ADES), dry eye is a multifactorial disease characterized by unstable tear film causing a variety of symptoms and/or visual impairment, potentially accompanied by ocular surface damage.1 Patients with DED experience a plethora of symptoms which may compromise vision-related quality of life. Advanced age, female sex, hormonal changes, refractive surgery, smoking, connective tissue disease, use of video display terminals, and environmental factors such as altitude and humidity are some of the known risk factors of DED.2 Advancements in and increased exposure to digital devices have resulted in DED becoming a public health issue across various age groups, including the younger generation.
The prevalence of DED ranges from 5% to 35% and is influenced by geographic location, lifestyle of people, and the use of different diagnostic criteria.3 In the Philippines, the only published study on DED by Panggat, Covar, and Lim Bon Siong showed a prevalence rate of 23% in a community in Metro Manila which is a highly urbanized area located at sea level.4 To the best of our knowledge, there is no other published literature regarding the prevalence of DED in other communities in the Philippines.
Baguio City is a mountain tropical city located north of Manila, in the Benguet Province of the Cordillera Region in the Philippines. This city has a unique climate owing to its 5,000 feet elevation which is classified as high-altitude.5 All year round, the city’s temperature and humidity are lower compared to most parts of the country. Due to the potential effect of altitude in DED, there is a need to expand epidemiological studies to more geographic regions. Other studies in Asia such as the Henan Eye Study reported a prevalence rate of 50% at a high-altitude locality in Mongolia.6 A study in Northern India with a higher elevation of 3,300 meters reported a prevalence of 54%.7 The aims of this research were to determine the prevalence, demographic profile, and clinical findings of DED in a high-altitude urban area in the Philippines and to compare it to the prevalence rate in an urban area in Metro Manila using the same set of diagnostic criteria for DED.
METHODS
This was a community-based, cross-sectional study conducted from March 2019 to September 2022 through convenience sampling of residents living in Barangay Lualhati, Baguio City. The study protocol was reviewed and approved by the University of the Philippines Manila Ethics and Review Board. Residents aged 19 years old and above were recruited with the cooperation of the officials of the barangay. Those who did not give consent or those with corneal pathologies, ocular infections and inflammation, lid abnormalities, history of ocular surgery within the last 6 months, and those who were using any form of ocular drops were excluded.
Once participants were deemed eligible and after they signed the written informed consent, demographic data and clinical symptoms were obtained and recorded. Each study participant answered two self-administered questionnaires: the Dry Eye Form of the Philippine General Hospital (PGH) and the Ocular Surface Disease Index (OSDI) questionnaire. Each participant underwent ocular examination and dry eye tests performed by a single trained ophthalmologist who was masked to the answers on the questionnaires. Ocular examination was carried out in the following order: (1) gross and slit-lamp examination of the anterior segment and eyelid margin to check for presence of lid margin telangiectasia, collarettes/fibrin crust, and meibomian gland plugging, (2) fluorescein tear break- up time (TBUT) measurement, (3) fluorescein staining on the cornea, (4) lissamine green staining on the conjunctiva and posterior lid margin, (5) Schirmer 1 test, and (6) basal secretion test (BST). Degree of corneal and conjunctival staining were graded with the Oxford Scale. Lastly, meibum secretion and quality were evaluated by applying digital pressure on both the upper and lower tarsus. All the interviews and clinical examinations were done at the barangay hall of the community. During the study period, ambient temperature ranged from 18.1C-20.7C, and humidity ranged from 84%-93%.
A diagnosis of dry eye disease was made if the participant had one or more symptoms rated as “most of the time” or “all of the time” in the OSDI questionnaire and/or a TBUT of less than 10 seconds and/or a Schirmer 1 test of less than 10 mm or a BST of less than 5 mm. DED was further categorized into 3 types: evaporative/short TBUT, aqueous tear deficiency (ATD), or mixed type. Evaporative/short TBUT type DED was diagnosed when there was an abnormal TBUT with normal Schirmer 1 and BST; ATD was diagnosed when TBUT was normal but with abnormal Schirmer 1 or BST; and mixed type was diagnosed when features of both evaporative/short TBUT and aqueous tear deficiency dry eye were present.
Statistical Analyses
Descriptive statistics was used. T-test was done to compare two continuous variables. Prevalence rate with 95% confidence interval was computed. Chi square test was used to determine associations between the disease outcome and the risk factors identified. All p-values <0.05 were considered significant.
RESULTS
Out of the 1,200 adult population in Barangay Lualhati, 274 participants were recruited in the study (22.7%). Two participants were excluded because they were not residents of the community. Data from the 272 participants were included and analyzed. Based on the diagnostic criteria for DED used in this study, 111 out of 272 participants were diagnosed to have DED, giving a prevalence rate of 41%.
Table 1 shows the mean age among the dry eye group was 43 years, which is significantly lower compared to those without dry eye at 51.8 years. More females were diagnosed with dry eye (59.5%) compared to males (40.5%). Majority of the participants were college graduates or in college level of education (75%). The most common concomitant systemic conditions in both groups were hypertension (21%) and diabetes mellitus (3.7%). However, there were significantly more participants with hypertension in the dry eye group.
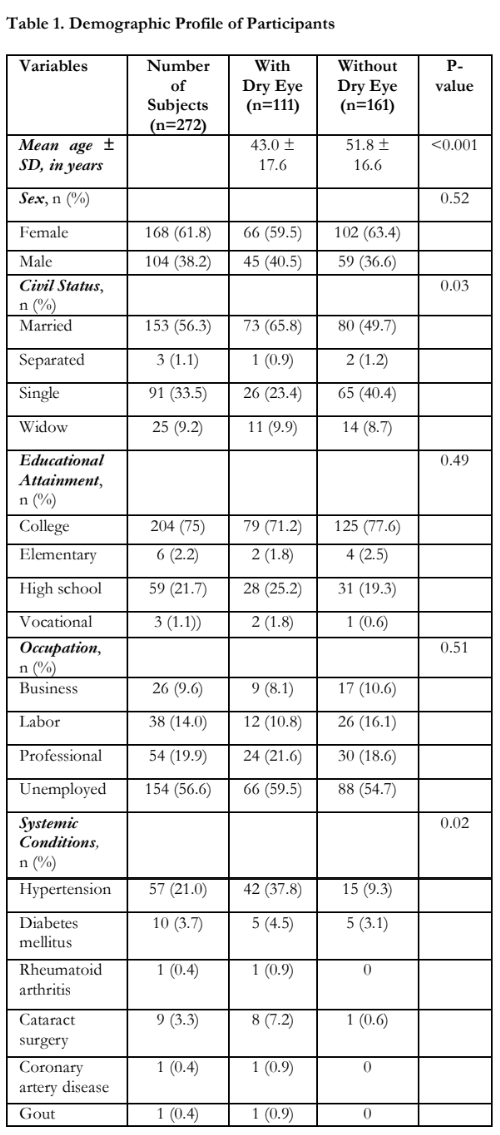
Figure 1 shows that the most common exacerbating condition in those with DED was screen time either using a personal device like a computer, watching TV, or playing video games (82%) followed by wind or fan use (29.7%).
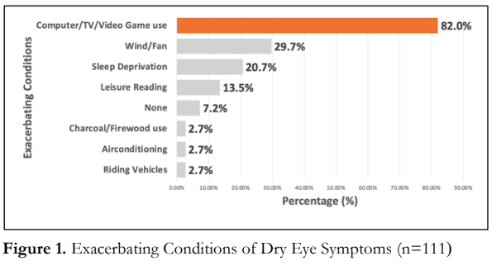
Figure 2 shows that the most common dry eye- related symptoms were foreign body sensation (55%) and burning or stinging sensation (51.4%).
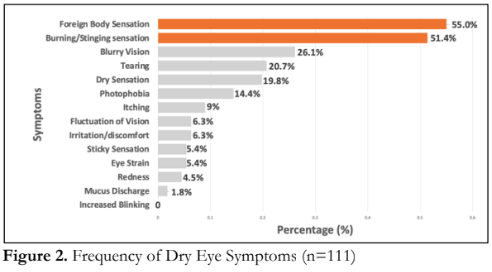
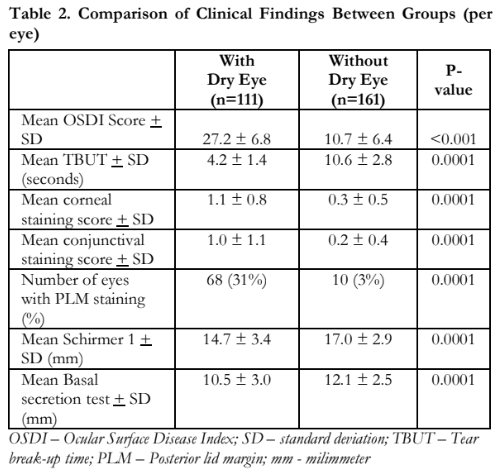
Table 2 shows the mean OSDI score of participants with dry eye (27.2 ± 6.8) was significantly higher than the mean score of those without dry eye (10.7 ± 6.4) (p<0.001). The mean TBUT was significantly lower in participants with dry eye (4.2 ± 1.4 seconds) compared to those without dry eye (10.6 ± 2.8 seconds) (p=0.001). The corneal, conjunctival, and posterior lid margin staining scores in participants with dry eye were significantly higher compared to those without dry eye (p=0.001). Mean Schirmer 1 and BST scores were significantly lower at 14.7 and 10.5 mm, respectively, for the dry eye group compared to 17.0 and 12.1 mm, respectively, in those without dry eye (p=0.001).
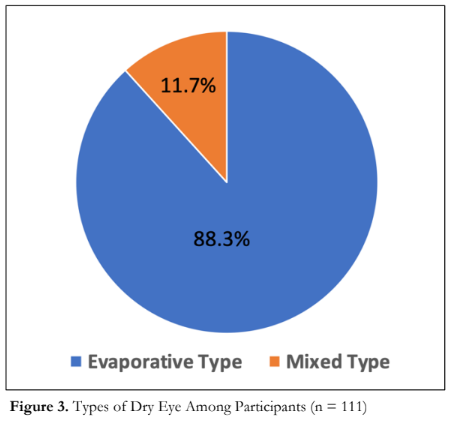
Figure 3 shows the distribution of the types of DED. Evaporative/short TBUT type of dry eye was the predominant form of dry eye in our study (88.3%) followed by the mixed type of dry eye (11.7%). There were no participants with pure aqueous deficiency type of dry eye identified in this study.
DISCUSSION
In this prevalence study conducted in a high- altitude urban community in the Philippines, the DED prevalence rate was 41% which is higher compared to the prevalence rate reported by Panggat et al. of 23% in a sea level community in Metro Manila.4 This is consistent with the increased prevalence of dry eye in studies done in high-altitude localities in Asia (50% and 54%).6,7 In high-altitude areas, the prevailing weather conditions and lower humidity levels compromise the tear film and increase tear evaporation promoting development of DED.6
A portion of the study was done during the COVID-19 pandemic where there was a significant increase in the use of screens and video display terminals as mobility of people were limited by global quarantine measures.8 A cross-sectional study in the USA reported that screen time increased by 20-30% during the pandemic.9 In our study, the most common exacerbating condition was screen use (82%). Prolonged screen time could have accounted for the increased prevalence rate seen in our study. Panggat et al. reported sleep deprivation (79%) and video display terminal use (65%) as the most common exacerbating conditions of dry eye.4 The DED prevalence among those who use video display terminals was shown in a meta-analysis to range from 9.5 to 87.5% with a global DED prevalence rate of 49.5%.10 A study done in Japan showed that the use of video screens for more than 4 hours was associated with a higher risk of DED, with longer screen time causing more severe symptoms.11,12 Furthermore, a meta-analysis done in 2023 showed an overall increase in the prevalence of DED to 61% during the COVID-19 pandemic.13 These results indicate that the use of video screens is an emerging risk factor for the development of DED.
In this study, subjects with DED had a mean age of 43 years compared to 52 years for those without dry eye. The current mean age is more than ten years younger compared to the previous prevalence study done in Manila of 54.6 years.4 The younger age of DED cases is contrary to our typical understanding that DED is mostly seen in the older age group. Dry eye symptoms and tear film instability in the younger population, including children, have been correlated with video screen time particularly before bed leading to sleep deprivation and the development of dry eye.14,15 Furthermore, this group is occupationally more active with increased exposure to video display terminals and air pollution. Our results underscore prolonged video screen time as a major factor in the development of DED especially in the young. The result also signifies a paradigm shift that DED is no longer just a problem of the older age group.
Dry eye symptomatology plays a big role in the diagnosis of the disease. The dry eye patients in our study reported foreign body sensation (55%) and burning/stinging sensation (51.4%) as the two most common symptoms. This differs from the results of the study done by Panggat et al. where the two most reported symptoms were itching and tearing.4 Our results were consistent with a study in a high-altitude community in India were foreign body sensation and grittiness were the most common complaints.3
Table 3 shows a comparison between clinical findings in this study and the study by Panggat et al. Our study has a lower TBUT (4.2 ± 1.4 vs 8.8 ± 3.1 sec). The corneal staining scores (1.1 ± 0.8 vs 0.3 ± 0.9) and conjunctival staining scores (1.0 ± 1.1 vs 0.8 ± 1.4) in this study were both higher compared to their study. The presence of posterior lid margin staining in the dry eye participants was lower in our study (31% vs 99%). Schirmer 1 and BST results were lower in our study (14.7 ± 3.4 mm vs 17.1 ± 1.0 mm, 10.5 ± 3.0 mm vs 11.9 ± 8.0 mm, respectively).4 Although the severity of dry eye was not specified in both studies, it would appear that this cohort had worse clinical findings compared to the cohort of Panggat et al. Risk factors, such as high altitude and video screen time, should be further investigated to determine causality with the severity of DED findings.

In this study, evaporative/short TBUT is the predominant type of dry eye disease and is consistent with the results of Panggat et al. (88% vs 67%, respectively). A tertiary hospital-based DED study by Lim Bon Siong et al. likewise reported evaporative/short TBUT dry eye (73%) as the most common form of DED in their cohort.16 This highlights the importance of TBUT in evaluating and detecting DED.
In summary, the prevalence rate of DED in Barangay Lualhati in Baguio City is 41% and is higher than the published prevalence rate in a community in Manila. The mean age of participants with dry eye in this study is younger compared to the participants without dry eye. Increased screen time is the most significant identified risk factor for the development of dry eye. Foreign body sensation and burning/stinging sensation are the most common reported symptoms. Evaporative/short TBUT dry eye remains as the predominant type of DED. Clinical findings of dry eye in this study are worse compared to the study done in Manila. A portion of this study was done during the COVID-19 pandemic lockdowns and may have confounded and affected the data. Selection bias may have also occurred during the study as residents with mobility issues either due to age or disabilities were not included in the sample. It is recommended to conduct similar studies with uniform diagnostic criteria of DED in different geographical regions to get a clearer picture of the prevalence rate of DED in the Philippines.
REFERENCES
- Tsubota K, Yokoi N, Shimazaki J, et al. New perspectives on dry eye definition and diagnosis: a consensus report by the Asia Dry Eye Society. Ocul Surf 2017;15(1):65-76.
- Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II Epidemiology report. Ocul Surf 2017;15:334–65.
- Titiyal J, Falera R, Kaur M, et al. Prevalence and Risk Factor of Dry Eye Disease in North India: Ocular Disease Index- Based Cross-Sectional Hospital Study. Indian J Ophthalmol 2018;66:207-11.
- Panggat K, Covar R, Lim Bon Siong R. Prevalence of Dry Eye Disease in an Urban Community. Philipp J Ophthalmol 2015;40:29-36.
- International Society for Mountain Medicine. Non- Physician Altitude Tutorial. June 24, 2011: https://themountainschool.com/wp- content/uploads/2017/11/Hi-Altitude_tutorial.htm (accessed January 15, 2024).
- Guo B, Lu P, Chen X, et al. Prevalence of Dry Eye Disease in Mongolians at High Altitude in China: The Henan Eye Study. Ophthalmic Epidemiol 2010;17(4):234–241.
- Gupta N, Prasad I, Himashree G, D’Souza P. Prevalence of dry eye at high altitude: a case controlled comparative study. High Alt Med Biol 2008;9(4):327-34.
- Regmi A, Suresh J, Asokan R. Changes in work patterns during COVID-19 lockdown and its impact on the eyes and body. Clin Exp Optom 2023;106(3)331–7.
- Meyer J, McDowell C, Lansing J, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Publ Health 2020;17(18):6469.
- Courtin R, Pereira B, Naughton G, et al. Prevalence of dry eye disease in visual display terminal workers: a meta- analysis. BMJ Open 2016;6(1):e009675.
- Yui Mineshita, Hyeon-Ki Kim, Hanako Chijiki, et al. Screen time duration and timing: effects on obesity, physical activity, dry eyes, and learning ability in elementary school children. BMC Public Health. 2021;21(1):422.
- Inomata T, Nakamura M, Iwagami M, et al. Risk factors for severe dry eye disease: crowdsourced research using Dry Eye Rhythm. Ophthalmology 2019;126(5):766-8.
- Ji H, Yang Y, Lu Y, et al. Prevalence of dry eye during the COVID-19 pandemic: A systematic review and meta- analysis. PLoS One 2023;18(12):e0288523.
- Clegg J, Guest J, Lehman A, Smith A. The Annual Cost of Dry Eye Syndrome in France, Germany, Italy, Spain, Sweden and the United Kingdom Among Patients Managed by Ophthalmologists. Ophthalmic Epidemiol. 2006;13(4):263-74.
- Uchino M, Schaumberg DA, Dogru M, et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology. 2008;115(11):1982–8.
- Lim Bon Siong R, Claudio KM, Dualan I, Sosuan, G. Clinical Profile of Dry Eye Disease at the Philippine General Hospital. Philipp J Ophthalmol 2022;47:23-30.

