Preseptal and orbital cellulitis at the Philippine General Hospital
Harvey S. Uy, MD, Prospero Ma. C. Tuaño, MD
PRESEPTAL and orbital cellulitis are potentially lifeand sight-threatening periocular infections with varied etiologies and severity.1 In the preantibiotic era, the complications of these infectious conditions such, as meningitis, brain abscess, and cavernous sinus thrombosis, resulted in high rates of mortality and blindness.2 Prevention of these complications requires appropriate and timely antimicrobial intervention. Aggressive organisms such as Haemophilus sp. were classically taught to be the primary causes of periocular cellulitis in children; however, the introduction of vaccines for Haemophilus influenzae may have resulted in changing microbiologic spectrum of preseptal and orbital cellulitis.3 Most of the published reports on preseptal and orbital cellulitis involve populations in developed countries.2-9 This study investigated the clinical patterns, causative agents, management practices, and outcomes of preseptal and orbital cellulitis in a developing country like the Philippines.
METHODOLOGY
The medical records of all consecutive preseptal- and orbital-cellulitis patients seen at the Orbit Clinic of the Philippine General Hospital from January 1990 to December 1995 were identified and retrieved. The patient charts were reviewed and the following data obtained: age, gender, presenting signs and symptoms, results of imaging studies such as computerized axial tomography (CAT scan), results of microbial investigation such as blood and tissue aspirate cultures, type of medical intervention, and outcomes.

Based on clinical findings and imaging studies, the patients were classified according to the scheme developed by Chandler:
• Group 1: Preseptal cellulitis (PC) – edema and inflammation confined to lid soft tissues.
• Group 2: Orbital cellulitis (OC) – true bacterial and leucocytic infiltration of orbital tissues with erythema, chemosis, eye pain, proptosis, limitation of eye movement, or some blurring of vision.
• Group 3: Subperiosteal abscess (SA) – collection of pus between the bony wall of the orbit and the periorbita.
• Group 4: Orbital abscess (OA) – collection of pus within the orbital soft tissue with marked exophthalmos, chemosis, severe impairment of vision, and ophthalmoplegia.
• Group 5: Cavernous sinus thrombosis (CST)– extension of migratory phlebitis into the cavernous sinus causing neurologic deficits and bilateral involvement.
RESULTS
Ninety-one patients presented with periocular infection. The distribution of patients according to the classification scheme of Chandler is presented in Table 1.
Preseptal Cellulitis (Group 1)
Fifty-six patients were diagnosed to have preseptal cellulitis (Group 1). The mean age at presentation was 12.6 ± 17.0 years (range, 0.1 to 65) and the median age was 4 years. No gender predilection was observed. The most common presenting signs of preseptal cellulitis are presented in Table 2. Bilateral involvement occurred in 9 of 56 patients (16%). Associated factors were identified in 48 of 56 (86%) patients (Table 3). The most common associated factors were lid infections and periocular trauma, which included eyelid abrasions, blunt trauma, dog bites, and one case of subgaleal hematoma. Nasolacrimal-duct obstruction was diagnosed in 10 of 56 (18%) patients. Microbial studies were performed for 5 of 56 (9%) patients. In 4 patients, samples were obtained from conjunctival discharge or from lid-abscess material while 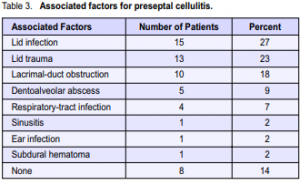
in one patient, blood was drawn and sent for culture and sensitivity studies. The conjunctival discharge established one case each of Staphylococcus aureus and gonococcal conjunctivitis that resulted in preseptal cellulitis. The rest of the samples resulted in negative cultures probably due to antibiotic treatment before consultation at our clinic. Because only a small number of patients underwent microbial studies, no conclusions can be made regarding the etiology of preseptal cellulitis. Imaging studies were performed in only 3 patients with a history of head trauma and sinusitis. Thirteen patients were admitted because of severe eyelid swelling that prevented a full ocular examination. Antibiotics were administered to all patients. Fifty-one of 56 (91%) patients were treated empirically with antibiotics. An intravenous loading dose was started in 46 of 56 (82%) patients. Cloxacillin or oxacillin was the preferred initial antibiotic (Table 4). In case of hypersensitivity to cloxacillin or oxacillin, cefazolin was administered because this drug has good coverage for Staphylococci. One patient with gonococcal conjunctivitis was given an intramuscular injection of ceftriaxone. Clindamycin was administered to one patient with maxillary sinusitis. In general, multiple antibiotics were started in patients with abscess formation or lid injury. Amoxycillin with clavulanic acid was administered to one patient who did not respond to penicillin. A surgical procedure was performed in 20 of 56 (36%) patients. Fifteen (27%) patients underwent incision and drainage of a preseptal or lid abscess, 4 (7%) underwent dental extraction, and one patient (2%) underwent evacuation of an associated subdural hematoma. All patients had improved at the time of discharge from the hospital. No complications were noted. None of the cases progressed to orbital cellulitis. Follow-up period ranged from one to two weeks. The short follow-up period is attributed to the lack of patient compliance with the follow-up schedule.
Postseptal cellulitis (Groups 2-5)
Thirty-five patients were diagnosed to have OC or its sequelae, OA and CST. Of these, 25 (71%) were classified as OC, 5 (14%) as OA, and 5 (14%) as CST. No cases of SA were observed. There were slightly more females than males (1.3:1). The mean age at presentation was 17.1 ± 18.6 years (range 0.8 to 78). The median age was 10 years. The most common signs and symptoms of OC, OA, and CST are presented in Table 5. Lid swelling, ophthalmoplegia, and chemosis were the most common presenting signs. Proptosis was present in 25 (71%) patients. Hertel’s exophthalmometry showed an average increase of 5.4 mm (range 1 to 10) in globe protrusion. Funduscopy revealed 4 patients with papilledema and 1 patient each with disc pallor, central-retinal-artery occlusion, and central-retinal-vein occlusion. Afferent pupil defects were seen in 6 of 35 (17%) patients. Resistance to globe retrodisplacement was observed in 5 of 35 (14%) patients. This low incidence may be due to interobserver variations in the interpretation of this
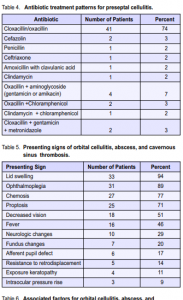

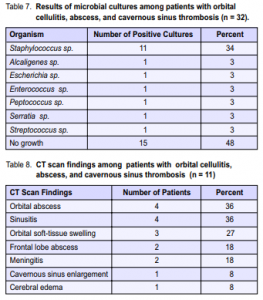
subjective test. Five of 35 (14%) patients presented with no light perception. Four patients (11%) had exposure keratopathy. Of 5 patients with OA, the average amount of proptosis was 8.0 mm (range 6 to 10). All CST patients presented with additional neurologic findings (behavioral changes, sensorial changes, neck rigidity, Babinski, headache, vomiting, and facial numbness). Predisposing factors were identified in 32 of 35 (89%) patients. Five of 6 (80%) patients with sinusitis manifested with ethmoid sinus involvement, 4 (67%) manifested with maxillary sinus involvement, and 1 patient (17%) had frontal sinus involvement. Multiple sinus involvement was seen in one patient. Trauma was a predisposing factor in 5 of 35 (14%) patients. Trauma included dog bites, blast injury, and penetrating eye injury. Panophthalmitis developed in patients with blast injury and penetrating injury. One patient each had associated chickenpox and concurrent septic arthritis (Table 6). Microbiological studies were done in 22 (63%) patients. Thirty-two samples were obtained, of which 17 (53%) yielded positive cultures. Orbital-abscess material yielded positive cultures in 9 of 13 (69%) patients while blood culture and sensitivity yielded 6 of 11 (54%) positive cultures. Isolates from culturing 3 conjunctival discharge specimen did not correlate with orbital-abscess aspirate or blood cultures. Cerebrospinal fluid and anterior chamber aspirates were negative (Table 7). Radiologic studies were done in 16 patients (46%). CT scan was performed for 11 patients who manifested with neurological changes, severe proptosis, or marked visual loss. The scans revealed 3 patients with intraorbitalsoft-tissue swelling, 5 with intraorbital abscesses, with extension of the abscess to the ethmoidal sinus in 1 patient and extension into the frontal lobe in 2 patients. Cerebral edema and cerebritis were seen in one CST patient who later expired from uncal herniation. Three of 8 (38%) who underwent orbital radiography demonstrated orbital soft-tissue densities or sinus haziness. Three patients underwent both CT scan and orbital radiography (Table 8). All patients diagnosed with orbital cellulitis were admitted for intravenous antibiotic treatment. The mean length of hospitalization was 17 days (range 1 to 78). Factors that influenced the choice of intial antimicrobial treatment included severity of the disease and focus of infection. Monotherapy with cloxacillin was administered to 12 (33%) patients. The remaining two-thirds received combination therapy that usually included a betalactamase-resistant penicllin derivative, an aminoglycoside or cephalosporin, and an antianaerobic antibiotic. The choice of medication was modified either by results of culture and sensitivity testing or by clinical response. Five out of 7 patients (71%) showed resistance to penicillin treatment (Table 9). The most common surgical intervention was incision and drainage of orbital abscess, performed when the patient was unresponsive to medical therapy. Drainage of the orbital abscess resulted in immediate and dramatic

improvement of the patient’s condition. Enucleation or evisceration was performed in patients with ruptured globe and subsequent panophthalmitis to remove the focus of infection. Ethmoidectomy and antrostomy were performed in 2 cases with chronic sinusitis. Patients with dentoalveolar abscesses were referred for either dental extraction or drainage of the abscess by the oral route. Tarsorrhaphy was performed in one case with exposure keratitis. Biopsy was performed in two cases where the initial impression was malignancy but later turned out to be an infectious abscess. One patient, a 4-year-old male with a dentoalveolar abscess with secondary cavernous sinus thrombosis and cerebral edema, died from complications of orbital infection. This patient developed uncal herniation despite drainage of intracranial abscess and medical therapy.
Visual Outcomes
None of the patients with PC suffered loss of visual acuity. Among the patients with postseptal infection, 10 (29%) experienced deterioration in visual acuity to 20/200 or worse. Five of 25 (20%) of OC patients, 4 of 5 (80%) of patients with OA, and 1 of 5 (20%) patients with CST lost all light perception. Nine patients continued to experience poor visual acuity even after treatment, with 3 eventually undergoing enucleation or evisceration and 6 losing all light perception permanently. Only one initially with no light perception demonstrated improvement in vision and obtained a final visual acuity of counting fingers. Proptosis was the most frequent clinical finding related to loss of vision (Table 5). Of 10 patients that were blind, 8 manifested with proptosis while only 2 patients without proptosis became blind.
Complications
Five patients developed elevated IOP that was easily controlled with topical carbonic anhydrase inhibitors and beta-blockers. Central-retinal-artery occlusion developed in 1 patient while central-retinal-vein occlusion affected 2 patients. These vascular occlusive events resulted in diminished visual acuity. Optic atrophy was observed in 2 patients. The neurologic complications included meningitis in 3 patients, brain-abscess formation in 2 patients, and uncal herniation in one patient that resulted in death. Residual neurologic deficits included ophthalmoplegia, facial anesthesia, and chronic papilledema.
DISCUSSION
PC and OC are two important infectious ophthalmic conditions. A Medline literature search revealed that most of the published articles on PC and OC are from developed countries. We conducted this study to determine the patterns of PC and OC in the Philippines where environmental and health standards may differ significantly from those in developed countries. In this series, PC occurred more frequently than OC and predominantly affected infants and young children, which may be related to the children’s relative lack of antibodies.5 OC affects older children and teenagers, occurs less frequently, but is a much more severe disease. These demographic data parallel published data from developed countries.5, 10 The most frequent signs of OC in this series were lid swelling, ophthalmoplegia, chemosis, proptosis, and decreased vision. Similarly, the Michigan study reported that the most frequent symptoms include lid swelling, proptosis, ophthalmoplegia, chemosis, and blurred vision. Limitation of ocular motility and proptosis are believed to be the most reliable signs of OC.11, 12 Skin, dental, and nasolacrimal infections were the predominant predisposing factors in this series in contrast to developed countries where trauma and respiratory-tract infections were the most important predisposing factors for preseptal cellulitis. These findings suggest that poor hygienic and dental care, as well as lack of access to medical care, can contribute to the development of PC. This series demonstrated concurrent skin infection (eg. eyelid infection from trauma, infected hordeolum, spread of other periorbital skin infection) as the most common predisposing factor, followed by sinusitis, trauma, dentoalveolar abscess, and respiratory-tract infection. In contrast, sinusitis, trauma, and systemic diseases like asthma and diabetes were the most common predisposing causes for OC in developed countries.12 Hodges and Tabarra reported similar trends in 23 patients from Saudi Arabia where only 30% of OC was associated with sinusitis.9 Concurrent infectious conditions were the predominant predisposing factors for OC in our series. This is probably due to poorer standards of hygiene and health care. Often, a neglected insect bite or skin wound led to a fulminant infection that spread to preseptal and postseptal tissues.9
Microbial studies were not performed for most cases of PC; however, majority of patients responded to empirical treatment. Since PC is a fairly benign condition, there was enough time for modification of drug therapy. Because OC is associated with more serious sequelae such as death and neurologic or ocular damage, appropriate antibiotic treatment should be started earlier and guided by the results of microbial studies as much as possible. In this series, around half of samples were positive for the causative agent, which were obtained from skin or orbital abscesses, the surfaces of infected wounds, or blood cultures. Staphylococcus sp. was the most common organism recovered from orbital or skin abscesses and infected wounds among patients with PC and OC. Other isolated microbes included anaerobes, Streptococcus, Escherichia, Neisseria, and Serratia sp. Weiss et al. reported Staphylococci as the most common organisms isolated in acute bacterial infections.5 Interestingly, Haemophilus, which is a common organism isolated in studies from developed countries,was not isolated in this series. Skin infections tended to be associated with Staphylococci and Streptococci while sinusitis and dental infections tended to be associated with mixed infections consisting of gram-negative and anaerobic bacteria. Radiological studies were not contributory to PC management because only a few were requested, but were very useful for the management of OC. In particular, CT scans confirmed the presence of sinusitis, orbital abscesses, and intracranial involvement and identified patients who needed aggressive intervention such as drainage of orbital and brain abscesses, anticoagulant therapy for CST, and selection of antibiotics with good brain-barrier penetration. Timely and appropriate antibiotic therapy is the most important component in the management of orbital infections. Empirical therapy should immediately be started after microbial specimens are obtained. Antibiotic selection may be guided by the foci of infection and disease severity. Patients with previous skin infections, trauma, or dacryocystitis usually received a beta-lactamase-resistant drug such as oxacillin, cloxacillin, or nafcillin. An intravenous loading dose may be given for more severe cases. Cephalosporin or amoxycillin with clavulanic acid is an alternative initial therapy. The UP-PGH infectiousdisease service recommends intramuscular ceftriaxone for cases with associated gonorrheal conjunctivitis. Patients with associated dentoalveolar abscesses or ear infections receive an additional aminoglycoside or chloramphenicol in order to cover for gram-negative organisms. Clindamycin or metronidazole is started when an anaerobic infection is suspected.13 The choice of antibiotics should be guided by culture and sensitivity results and clinical response. Lack of improvement or deterioration within 2 to 3 days should prompt modification of antibiotic treatment. Surgical intervention has an important role in the management of PC and OC. For patients presenting with toothaches, maxillary or mandibular swelling and tenderness, a dental evaluation can determine presence of dentoalveolar infections. Patients with otitis should be evaluated and treated by an otorhinolaryngologist. Orbital decompression is indicated for patients with impending visual loss, severe proptosis, glaucoma, or retinal vascular occlusion. Drainage of a localized infection such as orbital, dental, sinus, or intracranial abscesses or enucleation for endophthalmitis may remove foci of infection and lead to dramatic improvement of the clinical course. Biopsy may help distinguish an infectious from malignant process. Tarsorrhaphy may be useful for preventing exposure keratitis in cases where orbital pressure has normalized or where the primary goal is preservation of the ocular surface because of little visual potential. In summary, OC is associated with greater morbidity and mortality and should be treated early and aggressively. The proper use of imaging and antimicrobial studies can greatly guide appropriate therapy.
References
1. Westfall CT, Baker AS, Shore JW. Infectious diseases of the orbit. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology. Philadelphia: W.B. Saunders, 2000: 3121-3129.
2. Gamble RC. Acute inflammations of the orbit in children. Arch Ophthalmol 1933; 10: 483-497.
3. Donahue SP, Schwartz G. Preseptal and orbital cellulitis in childhood. Ophthalmology 1998; 105: 1902-1906.
4. Smith TF, O’Day D, Wright PF. Clinical implications of preseptal (periorbital) cellulitis in childhood. Pediatrics 1978; 62: 1006-1009.
5. Weiss A, Friendly D, Eglin K, et al. Bacterial and orbital cellulitis in childhood. Ophthalmology 1983; 90: 195-203.
6. Bergin DJ, Wright J. Orbital cellulitis. Br J Ophthalmol 1986; 70: 174-178.
7. Harris GJ. Subperiosteal inflammation of the orbit: a bacteriological analysis of 17 cases. Arch Ophthalmol 1988; 106: 947-952.
8. Clary R, Weber AL, Eavey R, Oot RF. Orbital cellulitis with abscess formation caused by sinusitis. Ann Otol Rhinol Laryongol. 1988; 97: 211-212.
9. Hodges E, Tabbara KF. Orbital cellulitis: Review of 23 cases from Saudi Arabia. Br J Ophthalmol 1989; 73: 205-208.
10. Spires JR, Smith RJ. Bacterial infections of the orbital and periorbital soft tissues in children. Laryngoscope 1986; 96: 763-767.
11. Rubin SE, Slavin ML, Rubin LG. Eyelid swelling and erythema as the only signs of subperiosteal abscess. Ophthalmology 1983; 90: 195-203.
12. Jackson K, Baker SR. Clinical implications of orbital cellulitis. Laryngoscope 1986; 96: 568-574.
13. Valenton MJ, Dy-liacco JU, Espiritu CG. Corneal and external-eye-disease problems in the Philippines. Phillip J Ophthalmol 1993; 22: 52-55.

