Predictors for failure of primary trabeculectomy
Franz Marie O. Cruz, MD, Patricia M. Khu, MD MS
SINCE its introduction 4 decades ago, trabeculectomy has remained the surgery of choice to lower intraocular pressure (IOP) in glaucomatous eyes. In various studies, the success rates ranged from 76% to 87%.1-11 However, complications and failure are inherent risks. Several studies have identified several risk factors that contribute to trabeculectomy failure: age below 40 years at the time of surgery, black race, presence of diabetes mellitus, an IOP greater than 40 mm Hg during the course of the disease, prolonged use of antiglaucoma medications, history of argon laser trabeculoplasty, pseudophakia or aphakia, and previous ocular surgery.4,6,10-11 Glaucomas associated with increased failure of trabeculectomies include steroid-induced, neovascular, uveitic, anglerecession, pseudophakia, and aphakia.7, 9, 12
Several surgical techniques have been associated with reduced risks of failure, including superonasal location of scleral flap13 and intraoperative use of mitomycin C.2-4, 6, 11, 14 Various studies reported conflicting results on the type of conjunctival flap created. Some studies showed higher success rates with limbus-based conjunctival flap compared to fornix-based,15 while others reported similar success rates between the two.16
Postoperatively, use of subconjunctival 5-fluorouracil injection has been associated with improved success rates,6,16 and performance of laser suture lysis with failed trabeculectomies.3
Hence, identification of risk factors for trabeculectomy failure will guide clinicians to institute early intervention within the perioperative period to increase chances for success. Identification of risk factors will also help clinicians during the preoperative counseling of patients regarding outcomes of surgery.
This study identified the risk factors for the development of failure in trabeculectomies done in a university hospital and determined the failure rate.
METHODOLOGY
All patients who underwent primary trabeculectomies from January 2005 to December 2007 were included in the study. They were identified from the operating-room records of the Department of Ophthalmology and Visual Sciences of the University of the Philippines–Philippine General Hospital (UP–PGH). Excluded were patients who underwent other ocular surgeries combined with trabeculectomy, repeat trabeculectomy, those who had congenital glaucoma, and those with less than one year of postoperative follow-up.
For patients who underwent bilateral trabeculectomies, only one eye was enrolled in the study. The eye with the more complete and accurate data was chosen.
Eyes that met the qualifying criteria were grouped according to the outcome of surgery. Cases were those who had failed trabeculectomies. Controls were those with successful trabeculectomies at one-year follow-up.
Successful trabeculectomy was defined as IOP of less than or equal to 21 mm Hg in all patients and less than or equal to 15 mm Hg in advanced glaucoma with at least 20% reduction from baseline IOP, and use of no more than 2 antiglaucoma medications at one-year follow-up. Failed trabeculectomy was defined as IOP greater than 21 mm Hg in all patients and greater than 15 mm Hg in advanced glaucoma at one-year follow-up. Eyes requiring further glaucoma surgery were also considered failures.
Optic disc and visual field as criteria for success were not analyzed. Outcome of trabeculectomy was assessed using a single criterion of IOP control.
Records were reviewed for the following preoperative parameters: age at the time of surgery, gender, presence of diabetes, history of ocular surgery, total number and duration of topical antiglaucoma medications, and previous laser treatment for glaucoma (i.e. peripheral iridotomy, peripheral iridoplasty, argon laser trabeculoplasty, goniophotocoagulation). The preoperative maximum IOP and type of glaucoma (i.e. primary open angle, pseudoexfoliation, pigmentary, primary angle closure, chronic angle closure, inflammatory, low tension, posttraumatic, steroid-induced, neovascular, and Chandler syndrome) were also recorded. The severity of the disease was graded based on the optic-disc appearance by slitlamp biomicroscopy with fundus lens examination. Mild to moderate glaucoma disease were those with cup-to-disc ratio (CDR) of less than 0.8 while advanced disease were those with CDR of at least 0.8.
The operative-technique record for each patient was reviewed and the following data were gathered: type of conjunctival flap (fornix- vs. limbus-based), site of scleral flap (superior, superonasal, superotemporal), shape of scleral flap (triangle, square, trapezoid), intraoperative use of mitomycin C (MMC) including concentration and duration, type of scleral flap suture (conventional interrupted vs. releasable), and competency of surgeon based on training level (resident, fellow, consultant).
The following post-operative data were obtained from the patients’ charts: intraocular pressures taken at postoperative day 1 (POD1), week 1 (POW1), months 1 (POM1), 3 (POM3), 6 (POM6), and year 1 (POY1); bleb manipulation (massage, needling, suctioning, suture removal); subconjunctival 5-fluorouracil (5FU) injection including total dose and timing of the first dose given, and number of post operative antiglaucoma medications.
All parameters collected were encoded and entered into Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). Statistical analyses were carried out using SPSS (Statistical Package for Social Sciences ver. 14, SPSS Inc., Chicago, IL, USA).
Measures of central tendency (mean) and dispersion (standard deviation) were obtained for continuous data (e.g. age, IOP). Rates and proportions were used for categorical data. Bivariate analyses were performed by cross-tabulating the risk factors according to success or failure.
To determine the causal association between risk factors and successful or failed trabeculectomy, unconditional logistic regression analysis was done to compute for the odds ratio and 95% confidence interval.
The study was approved by the ethics committee of the Expanded Health Research Office of the University of the Philippines–Philippine General Hospital.
RESULTS
From January 2005 to December 2007, primary trabeculectomy was performed on 253 eyes of 221 patients. One hundred ninety-two charts were reviewed and 104 patients met the inclusion criteria. Of the 104 patients who had at least one-year postoperative follow-up, there were 83 successful trabeculectomies and 21 failures, for a success rate of 79.8%.
The mean age of the study population was 54.34 ± 11.58 years old (range, 21 to 79). There was a difference in the mean age of the cases and the controls (Table 1).
Female patients accounted for 67.3% of all trabeculectomies. The number of failed trabeculectomies was similar for both sexes; the failure rate, however, was higher among males (26.5%) than among females (17.1%). This difference was not statistically significant (p = 0.39).
There were 52 trabeculectomies performed on the right eye with a failure rate of 26.9%, compared with 52 on the left eye with a failure rate of 13.5%. The difference was not statistically significant (p = 0.14).
Ninety-six percent of eyes that received various forms of laser treatment had successful trabeculectomies at oneyear follow-up, while 74% (57/77) of eyes that did not receive laser treatment prior to trabeculectomy had successful outcome at 1 year.
The mean preoperative IOP was 43 mm Hg for the cases and 44 mm Hg for the controls. There was no significant difference in the mean preoperative IOP between the 2 groups (Table 1).

For severity of disease, 67% of the failed cases had CDR ≥ 0.8 and 61% of successful trabeculectomies had advanced damage. This difference was not statistically significant (p = 0.73).
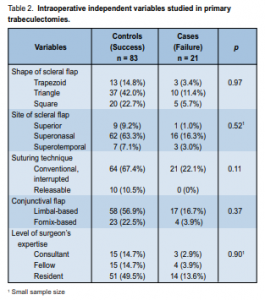
All trabeculectomies in this study were performed with intraoperative MMC at a concentration of 0.4 mg/ml applied for 2 minutes. Other intraoperative variables studies are summarized in Table 2.
There were 3 shapes of sclera flaps created: triangular flap was the most common at 53.4%, followed by square flap at 28.4%, and trapezoid at 18.2%. Failure rates of the triangular, square, and trapezoid flaps were similar at 21.3%, 20%, and 18.8% respectively (Table 2). The most common site chosen for the sceral flap was superonasal, with a failure rate of 20.5%. The samples for the superior and superotemporal sites were too small to make meaningful comparisons.
All failed cases occurred with the conventional interrupted sutures to anchor the scleral flap to the bed, and none when releasable sutures were used.
The limbus-based conjunctival flap was employed for 73.5% of surgeries with a success rate of 77.3%. The fornixbased approach had a slightly higher success rate at 85.2%. Most of the trabeculectomies were done by residents (63.7%), followed by fellows (18.6%), and consultants (17.6%). The residents had the highest failure rate (21.5%) followed by the fellows (26.1%) and the consultants (16.7%). The differences, however, were not statistically significant (Table 2).
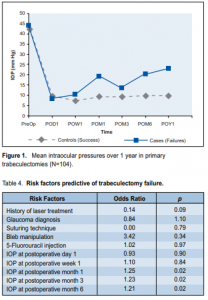
The mean follow-up for cases (failure) was 19.40 months (range, 12 to 43 months), while that for controls (success) was 19.03 months (range, 17 to 25 months). All postoperative mean IOP measurements in success and failed cases were significantly lower than preoperative mean maximum IOP (Table 3). For both cases and controls, the resulting IOP reduction from preoperative maximum IOP to day 1 postoperative were similar. In failed cases, however, the mean IOP started to rise as early as 1 week after surgery. A steep rise in the mean IOP among cases was observed at one-month follow-up (Figure 1).
Bleb manipulation in the form of massage, needling, and suctioning was performed in 52.9% of all posttrabeculectomy posttrabeculectomy eyes. Twenty-eight eyes (26.9%) received subconjunctival 5-FU injections. Suture removal was performed in 48 eyes (46.2%).
The logistic regression model included the main independent variables and those found to be significant in the univariate analysis. The preliminary model consisted of the following risk factors: preoperative laser treatment, severity of the disease, glaucoma type, and postoperative bleb manipulation. The IOP measurements from postoperative day 1 to month 6 of follow-up were each entered separately into the model (Table 4).
Of the risk factors, IOP at 1 month, 3 and 6 months were significantly associated with failed trabeculectomy, with odds ratio of 1.25, 1.23, and 1.21 respectively (p = 0.02, p = 0.02, p = 0.01).
DISCUSSION
Incidence rates
Using IOP reduction as the sole criterion for success at 1 year, the success rate of primary trabeculectomy with mitomycin C was 79.8% in this study. This is comparable with the 81 to 90% range reported in previous studies.3-4, 11, 14, 17 All these studies used intraoperative MMC in all their subjects with different types of glaucoma.
Although the criteria determining success and failure differed among the studies, the rates were similar. The criteria used in this study also took into account a much lower IOP for advanced glaucoma, which comprised 61% of the study population. In spite of this, the success rate was comparable to the overall published success rates of trabeculectomy.3-4, 11, 14, 17
Preoperative independent variables
Age has been suggested to affect the outcome of trabeculectomy,18 with poorer success rates among those younger than 40 years old.10 This was not observed in this study. Either the use of intraoperative MMC in all cases in this study has camouflaged the effect of age or the number of patients less than 40 years old (5 in this study) was too small to demonstrate an effect.
Even though there were more females included in the study, gender was not shown to be a risk factor for failure, consistent with results of other studies.10 The much higher percentage of females in the study is not an indication that more females undergo trabeculectomy; rather, that more females in the population fulfilled the follow-up criteria of 1 year, indicating perhaps better follow-up compliance than men.
Preoperative IOP was not found to be a risk factor for failure in this study (p = 0.93). This was in contrast to the study by Sturmer and colleagues10 who identified IOP >40 mm Hg as a risk factor for failure. However, they did not use intraoperative MMC and had a younger group of patients with a mean age of 33. The use of MMC has increased the success rates of trabeculectomies,2,11 including in this study, thereby reducing the effects of previously known factors.

This study did not show the effect of previous ocular surgery on eyes undergoing trabeculectomy with MMC in contrast to other studies where prior manipulation of the conjunctiva was identified to be a risk factor for failure of primary unenhanced trabeculectomy.7, 10, 19 Increased number of conjunctival fibroblasts and inflammatory cells from previous ocular surgery has been documented as the primary cause of poorer success rates.19 When trabeculectomy is augmented with MMC, an antimetabolite that inhibits fibroblast proliferation, success rates at one-year follow-up go up significantly. Other factors, such as the amount of mobile conjunctivae, the interval after the last procedure involving the conjunctival procedure, and the number of procedures with conjunctival incisions,19 may be more predictive of the success of surgery. These factors, however, were not within the scope of this study.
Presence of diabetes and history of laser treatment were not found to be predictive of trabeculectomy failure in this study, similar to previous investigations employing intraoperative MMC.11
The ratio of eyes with advanced disease was higher in the failed group than in the success group, largely as a result of the lower target IOP set for successful surgery in those with advanced cupping. Nevertheless, a high success rate was still observed in the advanced group.
Previous studies have identified the type of glaucoma as a risk factor for trabeculectomy failure. Glaucoma types associated with higher risk of trabeculectomy failure included posttraumatic, uveitic, neovascular,7, 18 and medically uncontrolled acute primary angle closure.1 Due to the small number of patients with glaucoma types other than primary open angle and chronic angle closure, the high-risk types (pseudoexfoliative, neovascular, posttraumatic, pseudophakic, inflammatory) were grouped together under “high-risk glaucomas” for purposes of statistical analyses. Findings in this study, however, showed that when trabeculectomy with MMC was performed, glaucoma type was not predictive of outcome.
The number and duration of topical ocular hypotensive agents have been associated with lower success rates of trabeculectomies by producing inflammatory changes in the conjunctivae,20-22 which were not observed in this study. Either the use of intraoperative MMC in all cases eliminated the previously recognized effects of long-term use of topical antiglaucoma medications or the number of patients on antiglaucoma medications for more than 12 months (10 in this study) was too small to produce an effect.
Intraoperative independent variables
Trabeculectomy creates a guarded outflow passage for aqueous from the anterior chamber to flow into the Tenon space. The factors that influence the establishment of sufficient filtration are not completely understood, but the inflammatory reaction and fibrotic response of the involved tissue have been shown to play a major role.17, 21 Several studies have tried to identify whether variations in surgical technique could affect the outcome.13, 15, 23-24
All trabeculectomies included in this study were performed with adjunctive MMC at a concentration of 0.04% for a duration of 2 minutes. Thus, the effect of intraoperative use of MMC or varying its dose and concentration on outcome could not be extrapolated.
Previous investigations reported conflicting results regarding the success rates of limbus- versus fornix-based conjunctival flaps. While older studies favor the use of limbus-based conjunctival flap in terms of better IOP reduction and less number of postoperative antiglaucoma medications, the findings in this study were more consistent with the results of Traverso’s15 where success rates of both conjunctival approaches were similar.
The shapes of the scleral flaps created in this study were not predictive of trabeculectomy failure, similar to findings in other studies.15
The location of the scleral flap was also not predictive of trabeculectomy outcome. Other studies have suggested better survival rates with superior location of the flaps.13
In this study, use of releasable sutures was started in 2007. Even with the small numbers, those with releasable sutures had 100% success rate compared to 75.3% using conventional interrupted sutures, similar to the results of the study by Raina and associates.23
Surgeon’s skills and competency were not demonstrated as risk factors for failure in this study, in contrast to the common sense that experience would improve the success rates. Analysis of variance showed no statistical difference in the failure rates among surgeries done by residents, fellows, or consultants. Results of this study were consistent with previous published studies that showed surgeon’s skills were not associated with outcome of trabeculectomy.7, 10, 20
Postoperative independent variables
Postoperative IOP at one month (POM1), 3 months (POM3), and 6 months (POM6) were all predictive of IOP at one-year follow-up with odds ratio of 1.25, 1.23, and 1.21 respectively. This means that there is a 20% chance that if the IOPs are low during these months, IOPs at 1 year would also be low (p < 0.001). Clinically, if the mean IOP remains in the low teens to single digits at POM1, the odds are that the IOP would remain low at 3 and 6 months, and most likely at 1 year. If the IOPs rise to mid and high teens by POM1, the odds increase that IOPs would be much higher at 1 year and the trabeculectomy would, therefore, be considered a failure, especially for advanced glaucoma cases where a low target IOP is essential. Those eyes would also require supplemental antiglaucoma medication earlier. Other studies have shown similar results.25-26 Most of the remodeling with active inflammation and repair process occurs during the first month, with scarring of the bleb expected during the second and third weeks postoperatively. This is characterized by increased vascularization around the filtering bleb with a more focal and less diffuse filtration. It is also at this time that if there is excessive healing, supplemental antifibrotic agents may be given at the area. Clinically, this is also seen as a rise in IOP. Thus, a rise in IOP may indicate excessive scarring, and if not managed early enough, may lead to failure. Hitchings and colleagues demonstrated that failure of trabeculectomy within the first few months was associated with a hypercellular response within the bleb, characterized histologically by inflammation and an increase in the number of active fibroblasts.27
Five fluorouracil (5-FU) is the most common antimetabolite given postoperatively to modulate wound healing. In large multicenter clinical trials, postoperative subconjunctival 5-FU has been shown to improve IOP control6, 28 and lower the risk of reoperations in posttrabeculectomy eyes with history of conjunctival incisional surgery.16 This study was not able to clearly demonstrate that postoperative injections of 5-FU improved success rates. One factor could be that the frequency and timing of the injections were on an as-needed basis depending on the clinical findings of increased vascularity and IOP rise. This is in contrast to the multicenter 5-FU studies in which injections were given regularly and consecutively.
This study had several limitations. Because it is a retrospective study with outcomes determined only up to 1 year, other variables may exert their effects beyond the period studied. Significant wound remodeling can still occur beyond 1 year that may affect long-term success rates. A larger sample size with longer follow-ups monitored prospectively to yield survival curves would demonstrate more clearly the effect of the different variables on the success rate of primary trabeculectomy over the long term.
In summary, the overall success rate of primary trabeculectomy at 1 year was 79.8%. Postoperative intraocular pressures at 1, 3, and 6 months were predictive of trabeculectomy failure at 1 year with odds ratio of 1.25, 1.23, 1.21 respectively.
1.Aung T, Tow SLC, Yap EY, et al. Trabeculectomy for acute primary angle closure. Ophthalmology 2000; 107: 1298-1302.
2.Bindlish R, Condon G, Sclosser J, et al. Efficacy and safety of mitomycin C in primary trabeculectomy: five-year follow-up. Ophthalmology 2002; 109: 1336-1342.
3.Fontana H, Nouri-Mahdavi K, Lumba J, et al. Trabeculectomy with mitomycin C: outcomes and risk factors for failure in phakic open-angle glaucoma. Ophthalmology 2006; 113: 930-936.
4.Fontana H, Nouri-Mahdavi K, Lumba J, et al. Trabeculectomy with mitomycin C in pseudophakic patients with open-angle glaucoma: outcomes and risk factors for failure. Am J Ophthalmol 2006;141: 652-659.
5.Lamping KA, Bellows AR, Hutchinson BT, et al. Long-term evaluation of initial filtration surgery. Ophthalmology 1986; 93: 91-101.
6.Lamping KA, Belkin JK. 5-fluorouracil and mitomycin C in pseudophakic patients. Ophthalmology 1995; 102: 70-75.
7.Mietz H, Raschka B, Krieglstein GK. Risk factors for failures of trabeculectomies performed without antimetabolite. Br J Ophthalmol 1999; 83: 814-821.
8.Mills KB. Trabeculectomy: a retrospective long-term follow-up of 444 cases. Br J Ophthalmol 1981; 65: 790-795.
9.Molteno AC, Bosma NB, Kittelson JM. Otago Glaucoma Surgery Outcome Study. Ophthalmology 1999; 106: 1742-1750.
10.Sturmer J, Broadway DC, Hitchings RA. Young-patient trabeculectomy. Ophthalmology 1993;100: 928-939.
11.Scott IU, Greenfield DS, Schiffman J, et al. Outcomes of primary trabeculectomy with the use of adjunctive mitomycin. Arch Ophthalmol 1998; 116: 286-291.
12.Mermoud A, Salmon JF, Murray AD. Posttraumatic angle-recession glaucoma: a risk factor for bleb failure after trabeculectomy. Br J Ophthalmol 1993; 77: 631- 634.
13.Negi AK, Kiel AW, Vernon SA. Does the site of filtration influence the medium to long-term intraocular pressure control following microtrabeculectomy in low-risk eyes? Br J Ophthalmol 2004; 88: 1008-1011.
14.Megevand GS, Salmon JF, Scholtz RP, et al. The effect of reducing the exposure time of mitomycin C in glaucoma filtering surgery. Ophthalmology 1995; 102: 84- 90.
15.Traverso CE, Tomey KF, Antonios S. Limbal- vs. fornix-based conjunctival trabeculectomy flaps. Am J Ophthalmol 1987; 104: 28-32.
16.The Fluorouracil Filtering Surgery Study Group. Five-year follow-up of the Fluorouracil Filtering Surgery Study. Am J Ophthalmol 1996; 121: 349-366.
17.Casson R, Rahman R, Salmon JF. Long-term results and complications of trabeculectomy augmented with low-dose mitomycin in patients at risk for filtration failure. Br J Ophthalmol 2001; 85: 686-688.
18.Inaba Z. Long-term results of trabeculectomy in the Japanese: an analysis by lifetable method. Jpn J Ophthalmol 1982; 26: 361-373.
19.Broadway DC, Grierson I, Hitchings RA. Local effects of previous conjunctival incisional surgery and the subsequent outcome of filtration surgery. Am J Ophthalmol 1998; 125: 805-818.
20.Lavin MJ, Wormald RPL, Migdal CS, et al. The influence of prior therapy on the success of trabeculectomy. Arch Ophthalmol 1990; 108: 1543-1548.
21.Broadway DC,Grierson I, Hitchings RA. Adverse effects of topical antiglaucoma medication: I. The conjunctival cell profile. Arch Ophthalmol 1994; 112: 1437-1445.
22.Broadway DC, Grierson I, Hitchings RA. Adverse effects of topical antiglaucoma medication: II. The outcome of filtration surgery. Arch Ophthalmol 1994; 112: 1446- 1452.
23.Raina UK, Tuli D. Trabeculectomy with releasable sutures. Arch Ophthalmol 1998; 116: 1288-1293.
24.Stark WJ, Goyal RK, Awad O. The safety and efficacy of combined phacoemulsification and trabeculectomy with releasable sutures. Br J Ophthalmol 2006; 90: 146-149.
25.Polikoff LA, Taglienti Z, Chanis RA, et al. Is intraocular pressure in the early postoperative period predictive of antimetabolite-augmented filtration surgery success? J Glaucoma 2005; 14: 497-503.
26.Alwitry A, Moodie J, Rotchford A, et al. Predictive value of early IOP in mitomycin- C-augmented trabeculectomy. J Glaucoma 2007; 16: 616-621.
27.Hitchings RA, Grierson I. Clinicopathological correlation in eyes with failed fistulizing surgery. Trans Ophthalmol Soc UK 1983; 103: 84-88.
28. Araie M, Shoji N, Shirato S, et al. Postoperative subconjunctival 5-fluorouracil injections and success probability of trabeculectomy in Japanese: results of fiveyear follow-up. Jpn J Ophthalmol 1992; 36: 158-168.

