Orbital Subperiosteal Abscess Secondary to Osteomyelitis in a Patient with Chronic Sinusitis
Steffani Krista Someda MD1 , Hendrik Onson MD2 , and Yvette Marie Santiago MD2
1Department of Oculoplastic, Orbital & Lacrimal Surgery, Aichi Medical University Hospital, Aichi, Japan
2Eye Institute, St. Luke’s Medical Center, Quezon City, Philippines
Correspondence: Yvette Marie Santiago
Clinic Address: 1405 N CHBC, St. Luke’s Medical Center, 279 E. Rodriguez Sr. Avenue, Quezon City 1112, Philippines
Clinic Phone Number: +632 8723 0101 ext 5105
Email Address: yvettesantiago@me.com
Disclosure: The authors report no conflict of interest.
Orbital subperiosteal abscess is an accumulation of pus between the periosteum and orbital bone that may occur secondary to direct spread of sinus infection.1 A history of chronic sinusitis or trauma may predispose the patient to infection of the orbital bone. This can lead to loss of vision and damage to the extraocular muscle. Hence, rapid, thorough diagnosis and treatment are essential in order to achieve rapid and thorough resolution of the infection and decrease the morbidity and mortality of the patient.
CASE REPORT
A 65-year-old, diabetic female presented with a two-month history of poor vision and a palpable orbital mass inferior to the left brow area. History started 4 months prior to consult when the patient was diagnosed with chronic rhinosinusitis at a different hospital and underwent functional endoscopic sinus surgery (FESS) with polypectomy and septoplasty. The procedure was reported to have no intraoperative complications and the patient recovered well and was discharged 7 days after the surgery. During the interim, she had febrile episodes associated with severe generalized headache and yellowish nasal discharge. She was readmitted for management of postoperative infection. She was given unrecalled intravenous antibiotics for 7 days. During the admission, she had new-onset right facial pain with associated bitemporal headache, relieved temporarily by pain medication. She was then transferred by relatives to another hospital after the 9th day of admission due to the persistence of the right facial pain.
Two months prior to consult at our institution, she was again transferred to another hospital where cranial magnetic resonance imaging (MRI) revealed bilateral mastoiditis, right-sided maxillary sinusitis, minimal chronic lacunes in the frontoparietal subcortices, equivocal enhancement of the trigeminal ganglion, and trigeminal neuritis. Lumbar tap and cerebrospinal fluid (CSF) fluid cytology showed occasional pus cells, high CSF protein (735 mg/dL), and high CSF glucose (5 mmol/L), suggestive of possible bacterial infection. She was started on intravenous ceftriaxone for 21 days and on the third week of admission, headache was noted to decrease in severity. However, she complained of decreased hearing on both ears at this time. Otoscopy revealed middle ear effusion. Pure tone audiometry showed profound hearing loss on the left ear and severe hearing loss on the right ear. She was advised to undergo revision of FESS but was not cleared for surgery due to her unstable condition. She then noted decreased vision on both eyes and a palpable mass on the left brow area. She was admitted for a month without resolution of her eye symptoms which prompted the consult at our institution.
On initial examination, there was no light perception on the right eye and the best-corrected visual acuity on the left eye was 20/400. The right pupil was dilated at 5 millimeter (mm) with minimal response to light; left pupil was 3 mm and sluggishly reactive to light. Relative afferent pupillary defect (RAPD) was present on the right eye. Extraocular muscle motility was also restricted in all gazes on both eyes. External examination revealed inferior displacement of the left globe and a palpable, fixed mass on the left superior orbital rim (Figure 1). Margin reflex distances and levator function were normal on both eyes. Hertel’s exophthalmometry showed 3 mm difference of protrusion on the left eye. There was a note of decreased sensation on the right hemifacial area, as well as decreased hearing on both ears. Fundus examination revealed optic disc pallor on the right eye and slightly pale-looking optic disc on the left eye.

Cranial MRI was repeated and showed multiloculated subperiosteal abscess collection along the left superior orbital rim with intraorbital extension along the roof, measuring 3.1 x 3.0 x 3.8 cm, with mild compression and inferior displacement of the left globe (Figure 2). Systemic work-up revealed increased white blood cell count with neutrophilia, elevated erythrocyte sedimentation rate and C-reactive protein, increased ferritin suggestive of an inflammatory condition, and a positive serum galactomannan indicative of fungal infection. 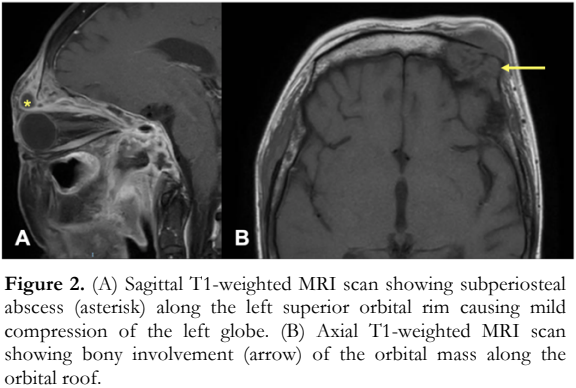
The patient underwent left anterior orbitotomy via a subbrow incision under general anesthesia with drainage of the orbital abscess and incision biopsy of the orbital mass and bone. Approximately 5 milliliters of mucopurulent fluid were drained. The surrounding tissue was excised and sent for study. The left superior orbital rim was noted to be friable and irregularly surfaced. Surrounding tissues of the orbital mass including bone were sent for pathologic evaluation. Gram stain and culture of the drained fluid were done. The fluid drained from the left orbital mass was negative for malignancy but its culture was positive for Pseudomonas aeruginosa and Enterobacter cloacae, which were sensitive to vancomycin and meropenem. Although the culture result was negative for fungal growth, fungal infection could not be completely ruled out due to the patient’s history of uncontrolled diabetes and positive serum galactomannan. Pathologic examination of the left superior orbital rim bone revealed signs of acute inflammation (Figure 3) consistent with osteomyelitis.

Postoperatively, the patient recovered well and was treated with intravenous vancomycin, meropenem, and amphotericin B. She was discharged but was lost to follow-up until 6 months later when granulation tissue on the postoperative site prompted consultation. There was no recurrence of the orbital mass and the patient’s vision on the left eye had slightly improved to 20/200. The rest of the ocular findings, however, neither improved nor worsened.
DISCUSSION
Osteomyelitis is an opportunistic infection of the bone that may result from: (1) hematogenous infection, (2) extension from a contiguous site, (3) direct introduction of pathogenic organisms into the bone via trauma or surgery, or (4) vascular insufficiency.2,3 This can cause non-specific symptoms such as fever, headache, and generalized body weakness. Since the advent of antibiotic therapy, the incidence of osteomyelitis has substantially decreased. However, the prevalence of diabetes has continued to increase worldwide, and alongside this problem is the growing incidence of opportunistic infections leading to possibly fatal complications, such as osteomyelitis.5
Bacterial infection of adjacent structures, such as in cases of sinusitis, has been reported to be the usual cause of orbital osteomyelitis, which can lead to abscess formation. Accumulation of pus between the orbital bones and periorbital layer results in the development of subperiosteal abscess. In 1983, Harris first reported 7 cases of orbital subperiosteal abscess that were treated with systemic antibiotic and surgical drainage of the abscess. Targeted antibiotic therapy is crucial for patients suffering from various systemic complications such as in this case. The presence of osteomyelitis necessitates removal of the infected bone and prolonged antibiotic therapy even after surgery.1 Although bone debridement was not achieved in this case, the patient was maintained on systemic antibiotic treatment even after hospital discharge. Unfortunately, since the patient was lost to follow-up, the duration of antibiotic treatment was not documented.
There are several factors to consider in the development of orbital osteomyelitis. Although sinus disease has been reported to cause orbital osteomyelitis, surgical trauma from the previous FESS may also have triggered the infectious process in our patient.4 It is, therefore, important to control the blood sugar level and seek clearance from endocrinology service prior to any surgical procedure. Furthermore, a history of uncontrolled type 2 diabetes mellitus, with persistently high blood sugar level of more than 180 mg/dL or hemoglobin A1C of >7%, predisposes the patient to opportunistic infections due to her immunocompromised state.5 Pseudomonas is a Gram-negative bacterium that has been found to be commonly involved in chronic sinusitis recalcitrant to medical and surgical therapy. Enterobacter bacteria are commensal organisms of the gastrointestinal tract and are considered opportunistic pathogens for patients with lowered resistance to infections, such as in uncontrolled diabetes. Susiyanti et al. has recently reported on two rare cases of orbital cellulitis in patients with type 2 diabetes, one of which was found to have periorbital abscess positive for Klebsiella pneumoniae and Enterobacter cloacae on bacterial culture of the collected pus.5 Suneetha et al. has also published a report on the microbiological profile of orbital abscess and has found that Pseudomonas aeruginosa and Enterobacter species were associated with more complications.6
Early detection of osteomyelitis can be made through computed tomography (CT) and MRI. As seen in our patient, the abscess may appear loculated due to periosteal adhesions to sutures between frontal and zygomatic bones.1 Osteomyelitis can spread to adjacent structures, leading to numerous complications that the patient presented with during her clinical course. In cases with increased susceptibility to opportunistic infections, such as in our patient with uncontrolled diabetes mellitus, the possibility of a fungal infection must be considered, especially if there is poor response to antibacterial therapy. Di Lullo et al. reported a case of otogenic skull base fungal osteomyelitis caused by Candida parapsilosis in a diabetic patient who presented with a subtle but aggressive clinical course.7 Even with a negative fungal culture, suspicion of a fungal etiology may be reinforced by a serum galactomannan test, which turned out positive in our patient. Given these findings, initiation of the anti-fungal amphotericin B was warranted. The treatment goal for osteomyelitis is directed to resolution of the infection while maximizing patient function.
In conclusion, osteomyelitis of the orbital bone is a complex problem requiring rapid and thorough diagnosis and treatment. It is a multifactorial disease and the clinical presentation varies. Complete resolution of the infection must be achieved to decrease the risk of morbidity and mortality of the patient.
ACKNOWLEDGEMENTS
The authors wish to thank Dr. Jeffrey Domingo of the Institute of Pathology at St. Luke’s Medical Center, Quezon City for the histologic photos and interpretation of the pathological findings.
REFERENCES
- Harris GJ. Subperiosteal abscess of the orbit. Arch Ophthalmol. 1980; 101: 751-757.
- Townsend DJ, Beyer-Machule CK, Fabian RL. Osteomyelitis of the orbit: A case report. Ophthalmic Plast Reconstr Surg. 1986; 2(1): 12-19.
- Hu AC, Ng WKY. Orbital osteomyelitis in the pediatric patient. J Craniofac Surg. 2021; 32: 206-209.
- El-Toukhy E, Szal M, Levine MR, Levine HL. Osteomyelitis of the orbit. Ophthalmic Plast Reconstr Surg. 1997; 13(1): 68-71.
- Susiyanti M, Hartono M, Pintary MR. Management of orbital cellulitis with periorbital abscess and rhinosinusitis in older patient with type 2 diabetes mellitus: a case series. April 18, 2022: https://assets.researchsquare.com/files/ rs-2169771/v1/98ea31b5-706a-4c9e-b7c1-b49e672b9771. pdf?c=1682243971 (accessed July 15, 2023).
- Suneetha N, Teena MM, Usha V, Mary J. Microbiological profile of orbital abscess. Indian J Med Microbiol. 2012; 30(3): 317-22.
- Di Lullo AM, Russo C, Grimaldi G, et al. Skull base fungal osteomyelitis: A case report and review of the literature. Ear Nose Throat J. 2021;100(10_suppl):1089S-1094S.

