Ocular Surface Manifestations of Ophthalmia Nodosa from Caterpillar Setae
Karlo Marco C. Claudio, MD1,2,3, Ulysses Joseph L. Yap, MD-MBA1,4
AFFILIATIONS:
1Department of Ophthalmology, Quirino Memorial Medical Center, Quezon City, Philippines
2Department of Ophthalmology, Rizal Medical Center, Pasig City, Philippines
3Tanay General Hospital Eye Center, Rizal, Philippines
4Department of Ophthalmology, Asan Medical Center, Seoul, South Korea
Correspondence: Karlo Marco Claudio, MD
Clinic Address: Quirino Memorial Medical Center, JP Rizal cor P Tuazon, Project 4, Quezon City
Email Address: mackyclaudio@yahoo.com
Clinic Phone Number: +639178404800
Disclosure: The authors report no conflicts of interest or financial disclosures.
Ophthalmia nodosa is an ocular inflammatory reaction secondary to exposure to foreign organic matter such as sharp vegetable matter or hairs (setae) of certain invertebrates such as caterpillars or spiders.1 These foreign bodies can lodge in the conjunctiva or cornea, and with further manipulation, may migrate to deeper structures. Depending on the depth of tissue involvement, these penetrating foreign bodies may cause various inflammatory responses such as conjunctivitis, conjunctival nodules, keratitis, iris nodules, uveitis, focal cataract, vitritis, macular edema, and endophthalmitis in severe cases.2 We report three cases of eye contact with caterpillar setae, describing the different clinical presentations and steps to treatment.
CASE PRESENTATION
Case 1
A 12-year-old female presented with 1-week foreign body sensation on the right eye after a caterpillar fell on her face. Gross examination showed right upper lid swelling, papillary conjunctivitis, and conjunctival injection and chemosis. Slit-lamp evaluation showed numerous fine caterpillar setae embedded in the upper palpebral conjunctiva and multiple linear abrasions with dye uptake on the temporal cornea (Figure 1). Findings posterior to the cornea were unremarkable.
Manual removal of setae was done and the patient was started on moxifloxacin 0.5% and loteprednol 0.5% eyedrops every 6 hours. One week later, there was improvement of the conjunctival injection but there was note of setae surfacing on the upper palpebral conjunctiva that was unseen during the initial consult. Topical medications were continued and manual removal of setae was done during two more follow-up sessions, leading to complete resolution of symptoms.
Case 2
A 52-year-old male with a history of caterpillar contact on his left eye came in due to redness and foreign body sensation. He was initially started on a topical antibiotic-steroid combination eyedrop 3 times a day at a different clinic. Persistence of symptoms prompted the patient to seek a second opinion at our institution.
On examination, there were several setae lodged in the temporal third of the left upper and lower lids accompanied by localized papillary conjunctival inflammation. A gross epithelial defect was seen at the temporal cornea corresponding to the location of the lodged setae on the upper lid (Figure 2A). A seta was also embedded on the temporal limbal conjunctiva extending to the posterior corneal stroma. This was associated with a small conjunctival granuloma at the suspected entry point (Figures 2B and 2C). There was no anterior chamber reaction, and the rest of the intraocular structures were unremarkable.

Manual removal of all accessible setae was done. Removal of the seta embedded in the limbal conjunctiva and cornea was attempted by careful dissection of the conjunctival tissue. However, the seta broke off prematurely upon retrieval, and only the proximal segment over the conjunctiva was removed. The distal segment remained embedded in the cornea with medial displacement within the posterior stroma. Topical levofloxacin 0.5% was prescribed, to be instilled every hour.
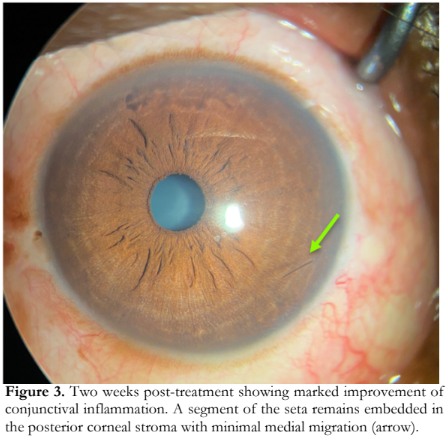
After 1 week, the corneal abrasion was fully healed. The corneal stroma and anterior chamber remained quiet, but significant conjunctival inflammation remained. Topical levofloxacin 0.5% was replaced with a topical steroid-antibiotic combination eyedrop three times a day. After 2 weeks, there was marked improvement of the conjunctival inflammation and resolution of the granuloma. The seta fragment embedded in the cornea remained inert without inciting further inflammation (Figure 3).
Case 3
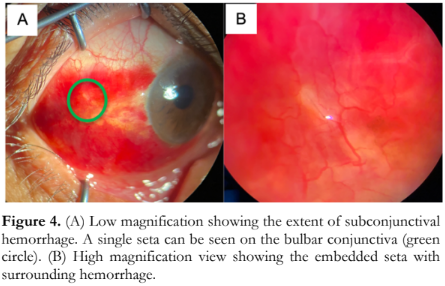
A 53-year-old hypertensive male experienced sudden onset redness with foreign body sensation in the right eye. A few hours prior to consult, he was cutting shrubs with caterpillars on the branches but did not recall a caterpillar landing on his eye.
Examination of the right eye showed an inferotemporal subconjunctival hemorrhage and a single seta embedded on the bulbar conjunctiva (Figure 4). Upon removal of the seta, there was immediate rebleeding at the puncture site which was controlled by applying pressure with a cotton-tipped applicator. The patient was advised to apply cold compress over the eye four times a day for the first 24 hours, then warm compress until the resolution of the hemorrhage. A topical steroid-antibiotic combination eyedrop was also given four times a day. Upon follow-up after 2 weeks, there were no additional setae detected, and the subconjunctival hemorrhage was seen to be gradually resolving.
DISCUSSION
While ophthalmia nodosa is a well-described ocular disease entity, the variations in symptomatology and extent of involvement may be a challenge to the general ophthalmologist. The Cadera classification (Table 1) provides a quick guide to management.3
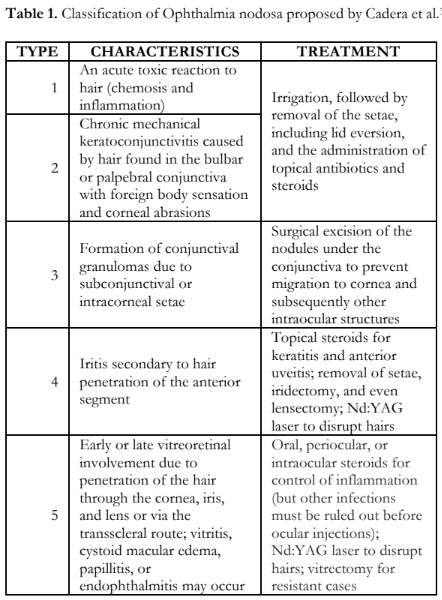
In this report, all cases were confined to the ocular surface and can be classified as Types 1-3 based on the Cadera classification. The subconjunctival hemorrhage observed in the third case is not described in the Cadera classification and we suggest that this finding should also be considered in setae-related injuries.
In all three cases, initiation of treatment and best efforts to remove all accessible setae, including meticulous checking of surfacing setae in succeeding clinic visits, resulted in significant improvements in inflammation. Complaints of persistent eye pain, redness or foreign body sensation, and/or fluorescein uptake should alert the clinician that there may be remaining setae lodged in the ocular surface tissues.
In conclusion, clinical features of ophthalmia nodosa may differ depending on the site of lodged setae in the eye. Treatment must include thorough examination for visible setae even on follow-up examinations. Prompt manual removal of setae, and initiation of appropriate symptomatic treatment with proper timing of steroid use, are both needed to decrease the risk of ocular surface damage, posterior segment migration of setae, and vision-threatening complications.
REFERENCES
- Joshi D. Ophthalmia nodosa with intraocular caterpillar setae. Med J Armed Forces India. 2011;67(2):167-168.
- Sahay P, Bari A, Maharana PK, Titiyal JS. Missed caterpillar cilia in the eye: cause for ongoing ocular inflammation. BMJ Case Rep. 2019;12(4):e230275.
- Cadera W, Pachtman MA, Fountain JA, Ellis FD, Wilson FM. Ocular lesions caused by caterpillar hairs (ophthalmia nodosa). Can J Ophthalmol. 1984;19(1):40-44.

