Intravitreal injection of bevacizumab before pars plana vitrectomy in tractional retinal detachment
DESPITE major advances in the medical management of diabetes mellitus (DM), diabetic retinopathy remains a leading cause of blindness worldwide. Proliferative diabetic retinopathy (PDR) is one of the major causes of severe visual loss among patients with DM. Almost half a century ago, Michelson identified the role of growth factors in the development of retinovascular diseases.1 By 1994, Aeillo recognized high levels of vascular endothelial growth factor (VEGF) in the vitreous of patients with PDR,2 prompting animal studies on VEGF. It was found that intravitreal injection of VEGF into normal primate eyes resulted in neovascularization, formation of microaneurysms, and increased vascular permeability. On the other hand, VEGF inhibition resulted in suppression of iris and retinal neovascularization.3-5 Human clinical studies also consistently demonstrated correlation of VEGF levels with the severity of PDR, such as the degree of retinal and iris neovascularization.6-7VEGF was found to be a potent inducer of vascular permeability, playing an important role in diabetic macular edema.8 Studies also concluded that there was a reduction of VEGF levels in the vitreous following successful laser treatment.9
Bevacizumab (Avastin, Genentech, San Francisco, California), a humanized monoclonal recombinant antibody that binds all isoforms of VEGF,10 is approved by the United States Food and Drug Administration for the treatment of metastatic colon cancer. Several studies involving intravitreal injection of bevacizumab in patients with choroidal neovascularization,11-12 central-retinal-vein occlusion,13 and PDR7, 14-16 reported favorable preliminary results. Initial animal trials concluded that a 2.5-mg dose intravitreally injected is nontoxic to the retina and optic nerve.17-18
Recently, intravitreal bevacizumab has been used as a preoperative adjunct for the repair of tractional retinal detachment (TRD) in severe PDR. A case series by Ishikawa and colleagues involving 8 eyes with TRD secondary to PDR concluded that pretreatment with intravitreal bevacizumab is likely effective in vitrectomy for severe PDR.19 An inter ventional, randomized, prospective study by Rizzo and colleagues, likewise, noted that preoperative intravitreal bevacizumab was well tolerated and reduced active neovascularization, thus facilitating pars plana vitrectomy (PPV).20
We report a case series of 5 patients who underwent preoperative intravitreal injection of bevacizumab demonstrating its efficacy as an adjunct to PPV.
CASE REPORT
This case series involved 5 eyes of 5 patients, 4 males and 1 female, aged 26 to 49 years, with preoperative visual acuity ranging from hand movement to counting fingers at 5 feet (CF5). All eyes had TRD with fibrovascular membrane (FVM) secondary to PDR. One eye was complicated by total rhegmatogenous retinal detachment (RRD) while another had extensive subhyaloid hemorrhage. Patients underwent routine ophthalmologic examination including fundus photography and fluorescein angiography (FA). Patients were asked to sign a consent form after extensive discussion of the risks and benefits of the treatment.
Bevacizumab 1.25 mg was injected followed by surgical repair in 5 to 7 days. One day prior to the surgery, postinjection fundus photos and fluorescein angiogram were taken. The 5 patients then underwent pars plana vitrectomy, membrane peeling, air-fluid exchange, endolaser, and silicon-oil injection. Intravitreal injection and surgical repair of TRD was done by a single surgeon.
Preoperatively, outcome measures observed were change in amount of vitreous and intraretinal hemorrhage, change in size of vessel caliber, amount of neovascularization, and the variability of size of the FVM. Main intraoperative outcome measures were ease in dissection during surgery, surgical time, and anatomical attachment.
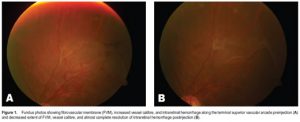
Fundus photos taken 1 day before surgery revealed significant reduction of FVM and attenuation of intraretinal hemorrhages in all 5 cases (Figure 1). A small decrease in vessel caliber was also noted. FA also showed remarkable regression of retinal neovascularization with fair resolution of dye leakage. Intraoperatively, there was minimum membrane dissection, minimal intraoperative bleeding in one patient that was easily controlled by endodiathermy. Surgery time ranged from 65 to 110 minutes. Complete anatomical attachment of the retina in all 5 eyes was achieved.
DISCUSSION
Preoperative injection of bevacizumab was believed to cause significant reduction in VEGF levels leading to attenuation of FVM, and reduced incidence of intraoperative bleeding and relatively shorter surgery time. 19-20 Our results were consistent with those of recent similar studies.
However, in a study by Avery,7 TRD was noted to worsen following the administration of intravitreal bevacizumab among patients with severe PDR. A retrospective study by Arevalo21 noted that the time from intravitreal injection to the progression of TRD was a mean of 13 days (range, 3 to 31 days). The natural course of PDR is described by a cycle of proliferation and regression of new vessels, followed by proliferation of fibrous tissue with neovascularization, resulting in adhesion of fibrous neovascularization to the posterior hyaloid face. Ultimately, TRD results from the contraction of the posterior vitreous face and the adherent proliferation. Thus, the progression of TRD following intravitreal injection of bevacizumab may be a component of the natural course of PDR. On the other hand, it can be assumed that the rapid neovascular involution with accelerated fibrosis and posterior hyaloid contraction as a response to low levels of VEGF may result in progression of TRD. In this series, however, no adverse event was noted. It was presumably because of the short time interval (5 to 7 days) between the preoperative injection and PPV, and that significant FVM contraction had not occurred; hence, worsening of TRD was not observed.
The amount of hemorrhage, vessel caliber, neovascularization, and fibrovascular membrane decreased significantly 7 days postinjection. The 5 cases exhibited minimal bleeding during dissection of the fibrovascular membrane.
Our results indicated that intravitreal injection of bevacizumab was an effective adjunct in the surgical treatment of TRD secondary to PDR.

