Implantation of an Alternative, Novel Glaucoma Drainage Device in the Treatment of Congenital Glaucoma Following Two Failed Filtration Surgeries
Aldo Mar B. Cariaga, MD, DPBO1
1Baguio General Hospital and Medical Center
Correspondence: Aldo Mar B. Cariaga, MD, DPBO1
Clinic Address: Rm 212, Pueblo de Maria Bldg., Notre Dame De Chartres, Gen. Luna Rd., Baguio City
Clinic Phone Number: +63 (074) 4424877
Email Address: domski2007@gmail.com
Disclaimer: The author reports no conflict of interest
Managing a failed glaucoma drainage device (GDD) is a daunting task even for an experienced glaucoma surgeon. Administration of anti-glaucoma drops is usually the first-line treatment in such cases. However, if medical therapy is inadequate, more invasive procedures such as laser or surgical bleb revision may be required.1 This is especially challenging in the pediatric population where the patient’s cooperation is needed during laser procedures or injection of subconjunctival anti-fibrotics.
Implanting a second GDD is one of the surgical options in managing a failed glaucoma shunt. This can be particularly burdensome to the patient considering that these devices can still fail. The failure rate of implanting a second GDD ranges from 13.6%-60%, depending on the definition of failure in each study.1-6Additionally, some surgeons will opt to use a different shunt for the second implant. However, there is limited published data about the success rates of implanting the same device or using a different one.1
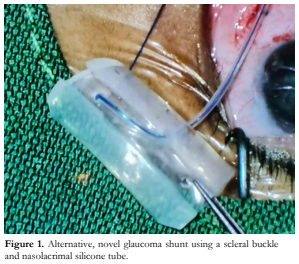
All GDDs consist of a silicone tube connected to a drainage plate. The tube drains the aqueous from the anterior chamber to the plate which functions to maintain a draining bleb or capsule. Of interest to this case is the Schocket tube implant. It uses an existing scleral buckle or an encircling band from a previous retinal surgery as the draining plate, while a silicone tube is attached from the inner capsule that has formed over the buckle/band extending to the anterior chamber.7,8,9 This study used the same raw materials as the Schocket implant to fashion a more affordable alternative GDD for the patient.
CASE REPORT AND SURGICAL TECHNIQUE
This is a case of a 6-year-old boy with congenital glaucoma who underwent trabeculectomy on the right eye. Two months after the first filtering procedure, due to a scarred bleb, a non-valved GDD (Aurolab Aqueous Drainage Implant, Aurolab) was inserted. His intraocular pressure (IOP) was initially controlled at low-to mid-teens.
However, 6 months after the glaucoma shunt insertion, the IOP increased to low 20s mmHg. This was initially controlled with a topical beta-blocker medication. At 7 months post-op, IOP remained elevated despite maximum tolerated medications or after removal of the ripcord suture.
The plan was to implant a second glaucoma shunt at the inferonasal bulbar area. However, due to financial constraints, a cheaper, alternative, novel GDD was fashioned from readily available materials in the hospital pharmacy, namely, a scleral buckle and nasolacrimal stent. The alternative GDD was created from a 1.5 cm portion of a scleral buckle with the edges trimmed to make them round. This served as the silicone plate of the shunt. Two holes located at the middle and near one end of the silicone plate were created. A silicone tube, obtained from a nasolacrimal stent, was passed through the underside portion of the middle hole, and then threaded to the topside of the other hole, to exit in the underside (Figure 1). The end of the tube entering the middle hole was made long enough to reach the anterior chamber. Nylon 4-0 was inserted through the silicone tube to function as a ripcord. Vicryl 6-0 was used to ligate the longer end of the tube near the plate, ensuring a watertight seal to prevent aqueous from initially reaching the plate posteriorly.
Informed consent describing the procedure was signed by the patient’s mother.
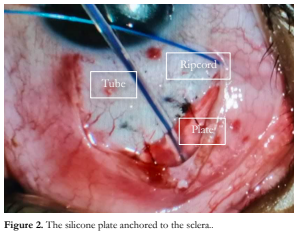
The patient underwent implantation with the alternative GDD under general anesthesia. After asepsis and antisepsis procedures were done, a surgical drape was placed and an eyelid retractor was applied. Conjunctival peritomy was performed at the inferonasal quadrant between the medial and the inferior recti muscles of the right eye. Tenon’s capsule was dissected away from the scleral and the bleeders were cauterized. The silicone plate was inserted about 8-10 mm away from the limbus and secured with nylon 10-0 (Figure 2). The silicone tube was trimmed to a length permitting 2-3 mm insertion into the anterior chamber and the bevel facing upwards. An anterior chamber paracentesis was formed. A partial thickness 4×4 mm limbus-based scleral flap was created at the position of the tube. A gauge 21 needle tract was created under the scleral flap, 2-3 mm posterior to the limbus, then advanced anterior and parallel to the iris plane. The silicone tube was inserted into the needle tract. The scleral flap was sutured over the tube with nylon 10-0. Finally, the Tenon’s capsule and conjunctiva were anchored to the limbus with nylon 10-0 to seal the surgical site. Post-operative medications included steroid and antibiotic eye drops.
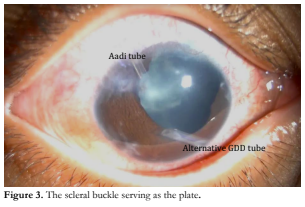
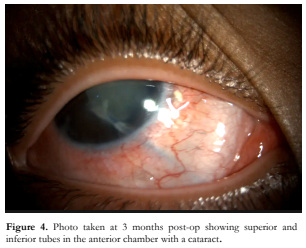
Postoperatively, IOP was 8-10 mmHg. There were no signs of infection or implant rejection (Figure 3). On the third month post-op, the patient developed a posterior subcapsular cataract (Figure 4). A minor post-op complication was implant migration anteriorly. The tube touched the corneal endothelium resulting in a localized corneal edema.
DISCUSSION
The author reported implantation of an alternative glaucoma shunt fashioned out of a scleral belt and nasolacrimal tube in a child with congenital glaucoma who had undergone 2 failed drainage procedures. Post-operatively, IOP was consistently measured to be 8-10 mmHg.
Tube migration is not an uncommon complication following GDD implantation. This is more common in children since their sclerae are still soft and pliable, making their axial lengths variable with IOP fluctuation. The varying globe size results in unpredictable tube positions after the surgery. The patient’s tube can easily be trimmed once cataract surgery is performed to address the localized corneal edema. The risk of tube displacement can be lessened by ensuring that the silicone plate is firmly anchored to the underlying sclera. Another possible solution is to utilize a wider silicone plate that can be tucked under the recti muscles, effectively anchoring the device at the equator of the globe.
This alternative glaucoma shunt may be particularly beneficial in resource-poor countries wherein the cost of even the cheapest GDD may be prohibitive. Long-term follow-up on its efficacy and safety are clearly needed.
This case presentation was able to demonstrate that an alternative GDD made from a scleral buckle and the silicone tube of a nasolacrimal stent may be a viable and cheaper alternative to the GDDs available in the market.
REFERENCES
- Blieden L. A Tube Shunt Fails: What’s Next? October 14, 2018: https://www.reviewofophthalmology.com/article/a- tube-shunt-fails-whats-next (accessed March 27, 2023).
- Anand A, Tello C, Sidoti P, et al. Sequential Glaucoma Implants in Refractory Glaucoma. Am J Ophthalmol. 2010;149:95-101.
- Shah AA, WuDunn D, Cantor LB. Shunt Revision Versus Additional Tube Shunt Implantation After Failed Tube Shunt Surgery In Refractory Glaucoma. Am J Ophthalmol. 2000;129 455-460.
- Godfrey DG, Krishna R, Greenfield DS, et al. Implantation of Second Glaucoma Drainage Devices After Failure of Primary Devices. Ophthalmic Surg Lasers. 2002; 33: 37-43.
- Omi CA, De Almeida GV, Cohen R, et al. Modified Schocket Implant for Refractory Glaucoma. Experience of 55 Cases. Ophthalmology. 1991;98(2):211-214.
- Burgoyne JK, WuDunn D, Lakhani V, Cantor LB. Outcomes of sequential tube shunts in complicated glaucoma. Ophthalmology. 2000;107:309-314.
- Schocket SS, Lakhanpal V, Richards RD. Anterior Chamber Tube Shunt To An Encircling Band in the Treatment of Neovascular Glaucoma. Ophthalmology. 1982;89:1188-1194.
- Schocket SS, Nirankari VS, Lakhanpal V, et al. Anterior Chamber Tube Shunt to an encircling Band in the Treatment of Neovascular Glaucoma and Other Refractory Glaucomas: A Long Term Study. Ophthalmology. 1985;92:553.
- Aref A. Modified Schocket Procedure Can Manage Glaucoma After Scleral Buckling Surgery. Feb. 10, 2013: https://www.healio.com/news/ophthalmology/2013020 8/10_3928_1081_597x_20130101_01_1025218 (accessed March 27, 2023).

