Cytopuncture Microbiopsy during Transcanalicular Endoscopic Lacrimal Duct Recanalization: A Novel Approach
Reynaldo M. Javate MD FICS1 , Rolando A. Lopez MD2
1University of Santo Tomas Hospital Eye Institute and Department of Ophthalmology, University of Santo Tomas Hospital, Manila
2Section Chief of Cytophatology, Department of Anatomic Pathology, University of Santo Tomas Hospital, Manila
Correspondence: Reynaldo M. Javate, MD, FICS
Clinic Address: Rm. 501, Doctors’ Clinics, 5th Floor, Clinical Division, University of Santo Tomas Hospital, España Blvd, Sampaloc Manila, Philippines 1008
Clinic Phone Number: +632-296-3636/ +632-731-3001 local 2516
E-mail: rmjavatemd@gmail.com
Disclosure: The authors report no financial conflict of interest.
Epiphora or tearing is a very common ocular symptom and it can be quite bothersome when it interferes with activities of daily living. Mechanisms of epiphora include hypersecretion, lacrimal pump failure, or lacrimal drainage obstruction. Lacrimal obstruction may be proximal involving a single or the common canaliculus, distally located involving the lacrimal sac or nasolacrimal duct, or a combination of both. The majority of acquired obstructions occur in adulthood and are more common in females.1,2 The surgical treatment for lacrimal obstruction is dacryocystorhinostomy (DCR) which involves marsupialization of the lacrimal sac into the nasal cavity.
External DCR remains the gold standard treatment of nasolacrimal duct obstruction in terms of functional outcome.3 However, complications associated with the procedure include cutaneous incisional scarring, injury to medial canthal structures, cerebrospinal fluid (CSF) rhinorrhea, periorbital bruising, copious hemorrhage, or late DCR failure. Alternative techniques have been developed such as endonasal laser DCR, endocanalicular and translacrimal laser DCR, fiber optic laser probing and endoscopic radiofrequency- assisted DCR. All of these techniques use microendoscopes that are able to pass through the lacrimal drainage system. They provide less invasive approaches in treating lacrimal outflow problems via direct visualization of the anatomy and precise localization of the pathology of the lacrimal system.4
These microendoscopes have also been used to biopsy lesions within the lacrimal drainage system through the external and endoscopic endonasal approaches. However, there are no reports yet of biopsies done during transcanalicular endoscopic lacrimal duct recanalization (TELDR). The objective of this study is to demonstrate the cytopuncture microbiopsy (CM) technique performed during TELDR in patients with primary acquired nasolacrimal duct obstruction (PANDO).
METHODS
This is a noncomparative, interventional case series of patients diagnosed with complete PANDO who underwent TELDR with balloon dacryoplasty, silicone intubation and CM at the University of Santo Tomas Hospital (USTH) performed by a single surgeon (RMJ). The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the hospital’s research ethics committee.
Patients diagnosed with PANDO in a private clinic in USTH from October 2014 to January 2017 were included in the study. The diagnosis of complete PANDO was made based on dye disappearance test, probing of the canaliculus, presence of fluid reflux upon pressure on the lacrimal sac, presence of fluid reflux from the superior canaliculus on canalicular irrigation with saline or direct visualization of nasolacrimal duct obstruction via microendoscopy. Patients with epiphora due to ocular surface disease, lower eyelid laxity, punctal stenosis and those with history of previous lacrimal surgery, post-traumatic bony deformity, canalicular or common canalicular obstruction, acute dacryocystitis, and congenital craniofacial abnormalities were excluded from the study. All patients signed a written consent prior to the procedure.
Surgical Technique
The procedure was performed under local anesthesia using a combination of proparacaine hydrochloride 0.5% solution instilled into the conjunctival cul-de-sac and irrigation of the lacrimal passage with 4% xylocaine. General anesthesia can be used based on the patient’s age, medical condition, or personal preference. Additional regional nerve block anesthesia to the medial canthal and infratrochlear areas using a mixture of 2% lidocaine with 1:200,000 epinephrine and 0.75% bupivacaine hydrochloride was given when the patient complained of pain.
The lacrimal puncta were expanded using two punctum dilators of increasing caliber. The Javate lacrimal trephine (Karl Storz GmbH and Co., Tuttlingen, Germany) with the microendoscope (Karl Storz Miniature Telescope 0 Degree; Karl Storz GmbH and Co., Tuttlingen, Germany) were inserted into the lumen of the canaliculus, advanced horizontally toward the medial wall of the sac and then rotated to assume a vertical position. As the trephine and the microendoscope were advanced, the site of obstruction was localized. After visualization of the obstruction in the lacirmal sac-duct junction, the trephine, inserted into the lumen of the microendoscope, was used to pierce through and remove the fibrous tissue obstruction up to the opening of nasolacrimal duct in the inferior meatus of the nose. The specimen was collected using an FCI biopsy cannula (Figure 1) attached to a 50-cubic centimeter (cc) syringe which was inserted into the Javate lacrimal trephine (Karl Storz GmbH and Co., Tuttlingen, Germany) (Figure 2). The specimen was visualized with the microendoscope. Then, once visualized, negative pressure from the 50-cc syringe was applied to collect the specimen (Figure 3). The specimens were placed in storage vessels containing 4% paraformaldehyde and 20% ethylenediamine tetraacetic acid which were sent for histopathologic examination. The obstruction was mechanically removed using the trephine while images of the lacrimal sac and nasolacrimal duct lumen were obtained and stored in the AIDATM DVD-M system with SmartscreenTM (Karl Storz GmbH and Co., Tuttlingen, Germany). The rigid 4-mm 300 Hopkins II® rhinoscope (Karl Storz GmbH and Co., Tuttlingen, Germany) was used to visualize the lacrimal trephine below the vault of the anterior end of the inferior nasal meatus. The microendoscope with the trephine was gradually withdrawn to view the recanalized nasolacrimal duct while providing continuous and forceful irrigation with saline to wash off remaining obstruction, debris, and mucosal secretions from the entire lacrimal drainage system using the Endomat® LC (Karl Storz GmbH and Co., Tuttlingen, Germany). Dilation of the stenotic areas with balloon dacryoplasty was done. Force was applied to the lacrimal balloon duct catheter along the nasolacrimal duct in a radial and longitudinal manner. This was followed by placement of a self-retaining, bicanalicular intubent stent. Antibiotic-steroid eyedrops (TobraDex®; Alcon laboratories, Inc., Fort Worth, Texas, USA) was used to flush the nasolacrimal duct mucosa at the end of the procedure. Post-operative medications include combination antibiotic-steroid eye drops. The patients were followed up the next day, then weekly for 1 month, then every other week for 6 months for nasolacrimal duct flushing with antibiotic-steroid eye drops. Pathology reports of the biopsy specimens were retrieved, reviewed and documented.

RESULTS
Eighteen (18) patients were included in the study. Sixteen (89%) were female. Mean age was 57.5 years. All patients presented with epiphora and duration of symptoms ranged from 6 to 48 months. All patients were diagnosed with complete nasolacrimal duct obstruction (NLDO). Two patients had complete bilateral NLDO while 16 patients had complete unilateral NLDO.
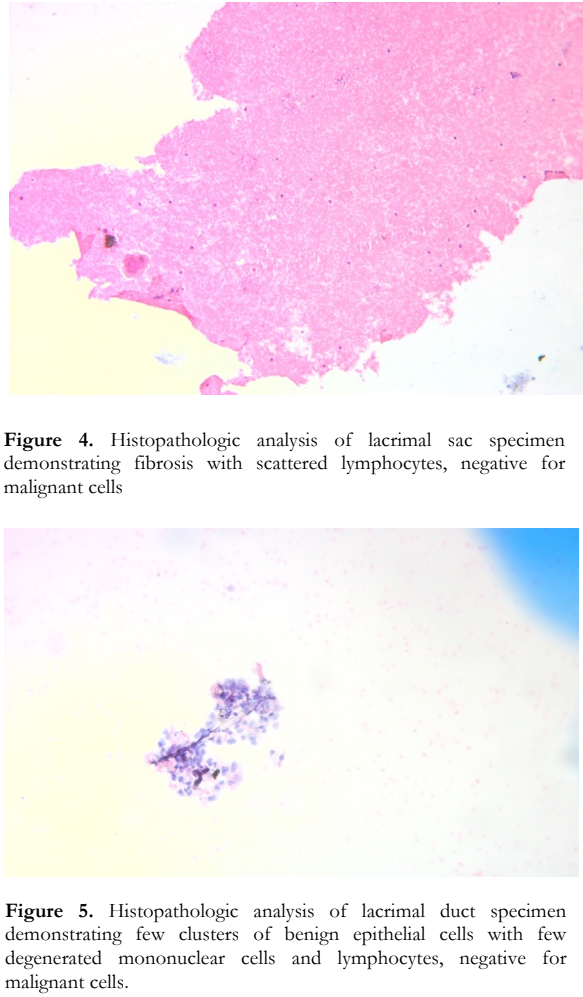
A total of 20 tissue specimens were taken and sent for histopathologic examination. All 20 tissue specimens revealed few clusters of benign epithelial cells with few degenerated mononuclear cells and lymphocytes and singly scattered lymphocytes that are set in fibrinous background on cell block analysis and cytology (Figure 4). Tissue cytology for all specimens were negative for malignant cells (Figure 5). All patients on follow up were functionally and anatomically patent.
DISCUSSION
To our knowledge, there is no literature or study on biopsy specimens taken transcanalicularly using the cytopuncture microbiopsy technique during TELDR. Endonasal and external DCR are invasive procedures but cytopuncture microbiopsy is minimally invasive. In this study, the cytopuncture microbiopsy technique is described during TELDR. It is a fast and efficient technique that can be integrated in the TELDR procedure. It is a less invasive approach. Together with direct visualization of the anatomy and precise localization of the pathology of the lacrimal system, an adequate specimen can be collected allowing the complete histopathologic studies of all the 20 specimens collected. It can serve as an alternative in obtaining biopsy specimens in patients with PANDO.
Lacrimal tumors can mimic PANDO. Several literatures reported patients initially diagnosed with PANDO who turned out to have malignancy after undergoing tissue biopsy.1,5-10 Koturovic et al. found neoplastic pathology in 55/3865 (1.42%) of the lacrimal sac wall they biopsied. Malignant cases were 2.24 times more frequent than benign. Lymphoma was the most common preoperatively unsuspected or intraoperatively unexpected neoplastic pathology.7 Tucker et al. obtained biopsy by external or endonasal DCR approach and found 98% of the 147 specimens had histopathologic findings consistent with inflammation or fibrosis of the lacrimal sac or both.8 Of note were changes in the diagnoses of 3 patients which were sarcoid granuloma oncocytoma, and lymphoma. Mauriello et al. found that majority of their specimens displayed chronic inflammatory changes.11 Goblet cells were missing in 2/3 of the specimens and marked fibrosis in half.
Several techniques on tissue sampling of the nasolacrimal canal also exist. Linberg and McCormick demonstrated an external DCR approach of excisional biopsy.1 Histopathologic analyses revealed a spectrum of changes that correlated with the symptom duration. Patients who had short symptom duration had active chronic inflammation along the entire length of the narrowed nasolacrimal duct. Those who had intermediate symptoms had signs of fibrosis and focal resolution of the inflammatory process while patients who had prolonged symptoms had fibrous obliteration of the entire duct.
Despite the previous literature reporting the presence of malignancy in patients initially diagnosed with PANDO, certain studies have concluded that routine biopsies are not necessary, not indicated, expensive, burdensome, and time consuming.6 With the cytopuncture microbiopsy technique, it can be advantageous since it is certainly not a time- consuming procedure for the surgeon and does not increase the cost of the surgery. It is just an additional step in the TELDR procedure. This technique can be performed routinely during TELDR in patients clinically suspected of cancer which will decrease the risk of overlooking primary malignant pathologies causing PANDO. It can be done as an outpatient procedure under topical and local anesthesia with no major complications.12,13 This procedure may bring forward the diagnosis of unsuspected or unexpected neoplasia. This is a minimally invasive procedure that offers an alternative to open biopsy technique that can be done routinely during TELDR under general anesthesia or local anesthesia as an office procedure. Further studies with more patients, more specimens and comparison with external DCR will help in future researches.
REFERENCES
- Linberg JV, McCormick, SA. Primary Acquired Nasolacrimal Duct Obstruction. A Clinicopathologic Report and Biopsy Technique. Ophthalmology 1986; 93(8): 1056.
- Woog JJ. The incidence of symptomatic acquired lacrimal outflow obstruction among residents of Olmsted County, Minnesota, 1976-2000 (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc 2007;105: 649-666.
- Savino G, Battendieri R, Traina S, et al. External vs. endonasal dacryocystorhinostomy: has the current view changed? Acta Otorhinolaryngol Ital 2014; 34(1): 29–35.
- Becker BB. Recanalization of the Obstructed Nasolacrimal Duct System. J Vasc Interv Radiol 2001;12: 697–699.
- Merkonidis C, Brewis C, Yung M, et al., Is routine biopsy of the lacrimal sac wall indicated at dacryocystorhinostomy? A prospective study and literature review. Br J Ophthalmol 2005; 89: 1589-1591.
- Koturović Z, Knežević M, Rašić DM. Clinical significance of routine lacrimal sac biopsy during dacryocystorhinostomy: A comprehensive review of literature. Bosn J Basic Med Sci 2017; 17(1): 1-8.
- Knezˇevic ́ M,Stojkovic ́M, Jovanovic, M,, et al.. A 7-year prospective study of routine histopathological evaluation of the lacrimal sac wall incisional biopsy specimens obtained during external dacryocystorhinostomy in adults and a review of the literature. Med Oncol 2012;29: 396–400.
- Tucker N, Chow D, Stockl F, et al. Clinically Suspected Primary Acquired Nasolacrimal Duct Obstruction Clinicopathologic Review of 150 Patients. Ophthalmology 1997; 104 (11): 1882-1886
- Paulsen FP, Thale AB, Maune S, et al. New Insights into the Pathophysiology of Primary Acquired Dacryostenosis. Ophthalmology 2001;108(12): 2330.
- 1Mills DM, Meyer DR. Acquired Nasolacrimal Duct Obstruction. Otolaryngol Clin N Am 2006;39: 979–999.
- Mauriello JA, Palydowycz S, DeLuca J. Clinicopathologic study of lacrimal sac and nasal mucosa in 44 patients with complete acquired nasolacrimal duct obstruction. Ophthalmic Plast Reconstr Surg 1992;8(1):13-21.
- Javate RM, Pamintuan FG, Cruz RT. Efficacy of Endoscopic Lacrimal Duct Recanalization Using Microendoscope. Ophthalmic Plast Reconstr Surg 2010;26 (5): 330-333.
- Javate RM, Roxas JLT. Surgical Technique and Preliminary Results of Transcanalicular Endoscopic Lacrimal Duct Recanalization and Balloon Dacryoplasty with Silicone Intubation in Filipino Patients with Complete Nasolacrimal Duct Obstruction. Philipp J Ophthalmol 2015; 40: 36-40.

