Comparison of the Rotational Stability of Different Toric Intraocular Lens Implants
Kate C. Torio, MD, Robert Edward T. Ang, MD, Gladness Henna A. Martinez, MD1, Jocelyn Therese M. Remo, MD
Implantation of standard intraocular lens (IOL) following cataract surgery corrects spherical refractive errors. However, patients with astigmatism still depend on spectacles for cylindrical correction.It has been estimated that 15% to 29% of patients with cataract have more than 1.50 diopters (D) of pre-existing astigmatism.1,2 This can be reduced or eliminated through astigmatic keratotomy, relaxing incisions, excimer laser keratectomy, and toric IOL implantation; all of which have their own advantages and disadvantages.
Astigmatic keratotomy combined with cataract surgery can improve a patient’s chances of excellent uncorrected postoperative vision. Limitations of this technique include lack of precision and reproducibility of incision depth and length, wound gape, epithelial ingrowth into the incision, infection, haze, scarring, and rarely, corneal perforation.3 Recently, studies on femtosecond laser technology seem to minimize these limitations. One advantage of femtosecond incisions is that they are customisable and adjustable, enabling the surgeon to create an incision according to the desired size, shape, length, and depth. In a study by Venter et al, the use of femtosecond laser astigmatic keratotomy improved mean uncorrected distance visual acuity (UDVA) from 0.18 ± 0.14 to 0.02 ± 0.12 logMAR, and cylinder from 1.20 ± 0.47D preoperatively to 0.55 ± 0.40D after surgery.
Limbal relaxing incision may be used to correct up to 3.5D of astigmatism through the use of a knife or blade, and more recently with femtosecond laser. The procedure is fast, easy to perform, gives highly predictable results, and is inexpensive. In a study by Carvalho et al, there was a significant improvement of best corrected visual acuity (BCVA) from 0.9 ± 0.7 logMAR preoperatively to 0.1 ± 0.1 logMAR at 1, 3, and 6 months postoperatively. There was also a significant reduction in the mean topographic astigmatism from 1.93 ± 0.58D preoperatively to 1.02 ± 0.60D at month 6 after surgery.
Excimer lasers (LASIK) have been used successfully to correct low to moderate astigmatism. Barraquer and Gutierrez evaluated LASIK in correcting hyperopic compound astigmatism in 111 eyes. Mean residual cylinder was -0.61D at 6 months and 71% of the eyes had UDVA of 0.50D or better.6 In another study by Kymionis et al, LASIK was found to be effective and predictable in terms of obtaining very Ophthalmologygood to excellent uncorrected visual acuity for eyes treated with mild to moderate astigmatism (less than 2.0D).
Today, toric IOLs represent a significant advance in achieving both optimal cylindrical and spherical refractions after cataract surgery, offering greater predictability and precision in the visual outcome of patients. The main advantage of toric IOLs over the cornea-based procedures mentioned above is that it can correct the sphere, cylinder, and cataract in a single-step procedure without creating an additional wound on the cornea. Several studies have found that different models of toric IOL are effective in astigmatic correction.8-17 However, rotation after toric IOL implantation has been a major concern.
Several studies have been made on toric IOLs, and most of those encountered were on AcrySof (Alcon Laboratories, USA). In a study on the AcrySof toric by Mendicute et al, IOL rotation was 3.63 degrees with a residual cylinder of 0.72D.21 In the study by Ruiz-Mesa et al, the mean rotation was 0.9 degrees, with a residual cylinder of 0.53D.22 In studies on the AT Torbi and AT LISA (Carl Zeiss, Germany), T-Flex (Rayner, United Kingdom), Tecnis (AMO, USA), and Lentis Mplus (Oculentis, Germany), the maximum mean rotation was 4.42 degrees (AT Torbi), while the minimum was 1.46 degrees (AT LISA). Residual cylinders of the different IOLs were more or less similar (0.43 to 0.9D).
Accurate positioning and rotational stability are essential for any toric IOL to function properly. The efficacy of astigmatic correction can be reduced by 33% in as little as 10 degrees of axis mis- alignment.
In most cases, capsular bag shrinkage due to fibrosis causes IOL rotation following uneventful cataract surgery.31 This is usually observed within the first 3 months after implantation.32 Specifically, the postoperative rotation of toric IOLs seems to occur in the early postoperative period of around 1 month, and remains constant after 6 months.24
Toric IOLs are available in different platforms.There are C-loop designs, such as the Alcon Toric (Alcon Laboratories, USA) and the Envista Toric (Bausch and Lomb, USA) series; plate haptic designs, such as the AT Torbi (Carl Zeiss, Germany) and Lentis Toric (Oculentis, Germany) models; and the double C-loop design with 4-point fixation POD-FT (Physiol, Belgium). All claim to have rotationally stable platforms. With the various options available, it is important to determine if there is a difference in rotational stability among these lenses. Since we had been using the same standardized surgical technique in cataract surgery and lens implantation, there is an opportunity to study and compare the IOL rotation in eyes we previously implanted with the various models of toric IOLs.
It is crucial for a toric IOL to maintain its position for consistent performance. Significant deviation from the intended axis causes deterioration of visual acuity, and, therefore, defeats the purpose of implanting a toric IOL. The significance of our study was in determining the toric IOL that demonstrates the greatest rotational stability. Patients with corneal astigmatism that will undergo cataract surgery in the future will be aided in deciding which specific toric IOL to choose.
This study compared the rotational stability, cylinder reduction, and refractive outcomes of eyes implanted with three different toric IOLs.
METHODOLOGY
PATIENTS
This was a prospective, analytical, cross-sectional study of patients who previously underwent phacoemulsification and were implanted with a toric IOL. Prior to cataract surgery, these patients had visually significant cataracts and had a preoperative corneal astigmatism of 0.75D or greater. The study followed the tenets of the Declaration of Helsinki, and all patients provided their written consent. Patients who came for postoperative follow up between January to September 2014 were invited to participate. Inclusion criteria were patients aged 40 years or older with preoperative regular corneal astigmatism of 0.75D or greater, were implanted with either AcrySof, Envista or FineVision toric IOL (Figure 1), and had at least 3 months of postoperative follow up. Patients with intraoperative complications (e.g., zonular dehiscence, capsular bag tear, etc.) were excluded.


Figure 1. Envista (A), AcrySof (B), and FineVision (C) toric IOL.
Preoperative Preparation and Surgical Technique
Prior to cataract surgery, a toric IOL calculator was used to determine the IOL power and the intended axis. On surgery day, while the patient was sitting up, ink marks were placed on the corneal limbus to mark 12, 3, 6, and 9 o’clock positions. During surgery, additional marks were placed on the cornea to coincide with the intended axis of placement based on the toric IOL calculator. After the lens was implanted, viscoelastic material was thoroughly removed in the anterior chamber and under the lens. Before ending the surgery, the dot or hash marks on the IOLs were checked to ensure that they were aligned to the intended axis based on the preplaced corneal marks. Any deviation afterwards was presumed to be caused by IOL rotation. A single surgeon performed all the cataract surgeries. Postoperative care followed routine standard of care after cataract surgery.
Study Examination
Patients previously implanted with toric lenses who came for routine follow up were invited to participate in the study. After securing informed consent, patients underwent vision testing, manifest refraction, slit lamp examination, and intraocular pressure test. The enrolled subjects’ eyes were then dilated using tropicamide with phenylephrine (Sanmyd-P, Santen, Japan) eye drops and were viewed through the slit lamp. Proper positioning was ensured by placing the subject’s head squarely on the chin rest, with both lateral canthi aligned with the marker on the slit lamp. IOL axis was determined by rotating the slit-lamp beam to align with the IOL toric markings (Figure 2). The axis deviation (in degrees) was computed as the difference between the intended axis as determined by the toric IOL calculator and the actual axis as read from the slit-lamp gauge that coincided with the IOL axis placement. Slit-lamp photos were taken for documentation. No surgical intervention was performed in this study.


Figure 2. Toric IOL axis determination through slit-lamp examination.
Statistical Analysis
Data were analyzed by getting the mean and standard deviation of patient demographics, refractive and visual outcomes. Axis deviations from the intended axis were determined, and comparison between the three groups was analyzed using F test through one-way ANOVA. The level of significance was set at p of less than 0.05.
RESULTS
Sixty-eight eyes of 44 subjects underwent phacoemulsification and were implanted with different toric IOLs. Twenty-three were implanted with Envista toric, 33 with AcrySof toric, and 12 with FineVision toric (Table 1).
Table 1. Patient demographics (N=44 subjects).


There was no difference in rotational stability among the three IOL groups (p=0.95) (Table 2). The overall mean absolute rotation was 2.47 degrees for Envista, 2.66 degrees for AcrySof, and 2.75 degrees for FineVision. All of the eyes in the Envista, 98% (32/33) in the AcrySof, and 92% (11/12) in the FineVision groups had axis rotation of 10 degrees or less.
Table 2. Comparison of the mean IOL axis deviation among the 3 groups (N=68 eyes).
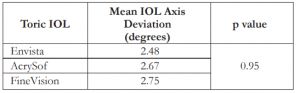

IOL – intraocular lens
Astigmatism correction was significant in all groups. A mean astigmatism correction of 0.86D (p=0.003) with a mean cylinder reduction of 50% was observed in the Envista, 0.63D (p=0.033) with a mean cylinder reduction of 33% in the AcrySof, and 1.29D (p=0.00) with a mean cylinder reduction of 67% in the FineVision groups (Table 3).
Table 3. Mean and percent cylinder reduction among the 3 groups.
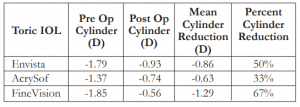

IOL – intraocular lens
Refractive outcomes for all groups were improved from preoperative to last postoperative visit. Mean refractive spherical equivalent for Envista (p=0.03), AcrySof (p=0.00), and FineVision (p=0.01) have all significantly improved. (Table 4). Uncorrected and best corrected visual acuity of Envista, AcrySof, and FineVision eyes, likewise, showed significant improvement (Table 5).
Table 4. Mean refractive outcomes for the 3 groups.
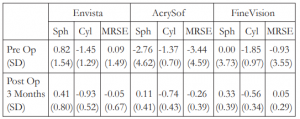

MRSE – mean refractive spherical equivalent
Table 5. Pre- and postoperative UCVA and BCVA (LogMAR and Snellen) for the 3 groups.
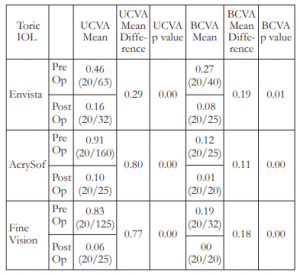

UCVA – uncorrected visual acuity, BCVA – best-corrected visual acuity
DISCUSSION
There are several ways of correcting corneal astigmatism during cataract surgery; namely, astigmatic keratotomy, limbal relaxing incision, and toric IOL implantation. Each has its own advantages and disadvantages.
In a study by Titiyal et al, toric IOL was similar to astigmatic keratotomy in terms of residual cylinder and visual acuity.33 The mean preoperative and postoperative refractive cylinders were 2.00 ± 0.49D and 0.33 ± 0.17D in the toric IOL group, and 1.95 ± 0.47D and 0.57 ± 0.41D in the keratotomy group. There were no differences in UCVA or BCVA between the two groups at any follow-up visit. However, corneal incisional solutions can be unpredictable due to factors including differences in nomogram, surgical techniques, and patient corneal biomechanics.
In order for a toric IOL to be the preferred option, it has to demonstrate consistent cylinder reduction and rotational stability.
This study compared the rotational stability of three different toric IOLs. The Envista and AcrySof platforms have a C-loop haptics design, whereas the FineVision has double C-loop 4-point-fixation design. The AcrySof has monofocal and multifocal toric models; the Envista has a monofocal toric model; and the FineVision has a multifocal toric model. We confined our analyses to rotational stability, cylinder correction, refractive outcomes, and distance vision measurements. Evaluation of presbyopia-correcting metrics were beyond the scope of this study.
Axis deviation and axis rotation have been used interchangeably and denote the shift in lens position from the time the IOL was implanted based on the axis recommended by the toric calculator to the time the IOL was evaluated at a specific time point after surgery, which in our study was a minimum of 3 months postoperatively. Any difference in IOL position was presumed to be caused by rotation after implantation.
To our knowledge, this is the first report of the Envista and FineVision toric platforms. Previous studies on other toric IOL platforms reported axis deviation to be between 0.9 to 4.42 degrees. The mean axis rotation was 2.47 degrees for Envista, 2.66 degrees for AcrySof, and 2.75 degrees for FineVision. These findings were consistent with the standards set by the other platforms of toric IOLs. There was no significant difference in the rotational stability of these 3 IOLs. All (23/23) eyes in the Envista, 98% (32/33) in the AcrySof, and 92% (11/12) in the FineVision groups had axis rotation of 10 degrees or less. It is believed that every 10 degrees of axis shift will cause a reduction in the cylinder correction of the lens by approximately 33%. We did not perform any IOL repositioning or IOL exchange in any eye included in this cohort.
In addition to rotational stability, astigmatism correction was significant in all three toric lenses, with mean cylinder reductions ranging from 33% to 67%.Mean postoperative astigmatism ranged from 0.56 to 0.93 diopters. Refractive and visual outcomes were, likewise, excellent.
It is worthwhile to note that the greatest reduction in cylinder was observed in the FineVision group. We theorized that due to the four-point fixation design, the lens remained stable once it was implanted and, therefore, suffered less loss of astigmatism-correcting capability due to post-implantation rotation. Intraoperative observation supported this hypothesis because during the removal of viscoelastic, the FineVision toric lens had less spinning motion compared to the C-loop designs. In addition, C-loop lenses can only be rotated clockwise; so during positioning, if the surgeon overshoots the axis of alignment, he has no choice but to rotate the lens 180 degrees to try to realign the toric marks again. On the other hand, the POD-F design of the FineVision and the plate-haptic design of the Zeiss and Oculentis lenses allow the surgeon to rotate the lens into place in a clockwise or counter-clockwise direction. With equally effective outcomes, ease of use may play a role in the choice of which toric lenses to use.
The common sources of error in axis placement were inconsistent markings, cyclotorsion of the eye, and induction of surgically-induced astigmatism during creation of clear corneal incisions. An iris registration and automated guidance system in conjunction with intraoperative aberrometry are recommended to help increase the accuracy of toric IOL placement and outcomes.
In summary, all three IOLs demonstrated good rotational stability and cylinder reduction. Use of any of the three IOLs (Envista, AcrySof, and FineVision) can give good refractive and visual outcomes.
REFERENCES
1. Hoffer KJ. Biometry of 7,500 cataractous eyes. Am J Ophthalmol 1980;90:360-368; correction, 890.
2. Ninn-Pedersen K, Stenevi U, Ehinger B. Cataract patients in a defined Swedish population 1986-1990. II. Preoperative observations. Acta Ophthalmol (Copenh) 1994;72:10-15.
3. Raoof-Daneshvar D, Mian SI. Femtosecond laser-assisted astigmatism correction. In Goggin M (eds), Astigmatism – Optics, Physiology and Management. Rijeka: Intech; 2012.
4. Venter J, Blumenfeld R, Schallhorn S, Pelouskova M. Non-penetrating femtosecond laser intrastromal astigmatic keratotomy in patients with fixed astigmatism after previous refractive surgery. J Refract Surg 2013;29:180-186.
5. Carvalho MJ, Suzuki SH, Freitas LL, et al. Limbal relaxing incisions to correct corneal astigmatism during phacoemulsification. J Refract Surg 2007;23:499-504.
6. Barraquer CC, Gutierrez MAM. Results of laser-in-situ keratomileusis in hyperopic compound astigmatism. J Cataract Refract Surg 1999;25:1198-1204.
7. Kymionis GD. Correcting astigmatism with the excimer laser. Cataract Refrac Surg Today Eur 2010;Sept:25-27.
8. Grabow HB. Early results with foldable toric IOL implantation. Eur J Implant Refract Surg 1994;6:177-178.
9. Grabow HB. Toric intraocular lens report. Ann Ophthalmol 1997; 29:161–163.
10. Werblin TP. Do three-piece PMMA IOLs rotate after implantation in the capsular bag? J Refract Surg 1995;11:468-471.
11. Sun XY, Vicary D, Montgomery P, Griffiths M. Toric intraocular lenses for correcting astigmatism in 130 eyes. Ophthalmology 2000;107:1776-1781; discussion by RM Kershner, 1781-1782.
12. Ruhswurm I, Scholz U, Zehetmayer M, et al. Astigmatism correction with a foldable toric intraocular lens in cataract patients. J Cataract Refract Surg 2000;26:1022-1027.
13. Gerten G, Michels A, Olmes A. Torische Intraokularlinsen; klinische Ergebnisse und Rotationsstabilita¨ t. [Toric intraocular lenses; clinical results and rotational stability.]. Ophthalmologe 2001;98:715-720.
14. Leyland M, Zinicola E, Bloom P, Lee N. Prospective evaluation of a plate-haptic toric intraocular lens. Eye 2001;15:202-205.
15. Till JS, Yoder PR Jr, Wilcox TK, Spielman JL. Toric intraocular lens implantation: 100 consecutive cases. J Cataract Refract Surg 2002;28:295-301.
16. Chang DF. Early rotational stability of the longer Staar toric intraocular lens; fifty consecutive cases. J Cataract Refract Surg 2003;29:935-940.
17. De Silva DJ, Ramkissoon YD, Bloom PA. Evaluation of a toric intraocular lens with a Z-haptic. J Cataract Refract Surg 2006;32:1492-1498.
18. Gills JP, Van der Karr M, Cherchio M. Combined toric intraocular lens implantation and relaxing incisions to reduce high preexisting astigmatism. J Cataract Refract Surg 2002;28:1585-1588.
19. Viestenz A, Seitz B, Langenbucher A. Evaluating the eye’s rotational stability during standard photography; effect of determining the axial orientation of toric intraocular lenses.J Cataract Refract Surg 2005;31:557-561.
20. Weinand F, Jung A, Stein A, et al. Rotational stability of a single piece hydrophobic acrylic intraocular lens: new method for high precision rotation control. J Cataract Refract Surg 2007;33:800-803.
21. Mendicute J, Irigoyen C, Aramberri J, et al. Foldable toric intraocular lens for astigmatism correction in cataract patients. J Cataract Refract Surg 2008; 34:601-607.
22. Ruíz-Mesa R, Carrasco-Sánchez D, Díaz-Alvarez SB, et al. Refractive lens exchange with foldable toric intraocular lens. Am J Ophthalmol 2009;147:990-6, 996.e1.
23. Venter J, Pelouskova M. Outcomes and complications of a multifocal toric intraocular lens with a surface-embedded near section. J Cataract Refrac Surg 2013;39:859-866.
24. Bascaran L, Mendicute J, Macias-Murelaga B, et al. Efficacy and stability of AT TORBI 709 M toric IOL. J Refract Surg 2013;29:194-199.
25. Tsinopoulos IT, Tsaousis KT, Tsakpinis D, et al. Acrylic toric intraocular lens implantation: a single-center experience concerning clinical outcomes and postoperative rotation. Clin Ophthalmol 2010;4:137-142.
26. Venkataraman A, Kalpana. Visual outcome and rotational stability of open-loop toric intraocular lens implantation in Indian eyes. Indian J Ophthalmol 2013;61:626-629.
27. Shah GD, Praveen MR, Vasavada AR, et al. Rotational stability of a toric intraocular lens: influence of axial length and alignment in the capsular bag. J Cataract Refract Surg 2012;38:54-59.
28. Hirnschall N, Maedel S, Weber M, Findl O. Rotational stability of a single-piece toric acrylic intraocular lens: a pilot study. Am J Ophthalmol 2014;157:405-411.
29. Daya SM, Bellucci R. Assessment of postoperative vision and cylinder correction. Cataract Refrac Surg Today Eur 2014; Nov:30-33.
30. Alberdi T, Macías-Murelaga B, Bascarán L, et al. Rotational stability and visual quality in eyes with Rayner toric intraocular lens implantation. J Refract Surg 2012;28:696-701.
31. Visser N, Bauer NJC, Nuijts RMMA.Toric intraocular lenses in cataract surgery. In Goggin M (eds), Astigmatism – Optics, Physiology and Management. Rijeka: Intech; 2012.
32. Strenn K, Menapace R, Vass C. Capsular bag shrinkage after implantation of an open-loop silicone lens and a polymethyl methacrylate capsule tension ring. J Cataract Refract Surg 1997;23:1543-1547.
33. Titiyal JS, Khatik M, Sharma N, et al. Toric intraocular lens implantation versus astigmatic keratotomy to correct astigmatism during phacoemulsification. J Cataract Refract Surg 2014;40:741-747.

