Clinical Profile of Keratoconus Patients at the Philippine General Hospital
Pablito F. Sandoval Jr., MD1,2, George Michael N. Sosuan, MD1, Reginald Robert G. Tan, MD1,3, Ruben Lim Bon Siong, MD1,3
1Department of Ophthalmology and Visual Sciences, Philippine General Hospital, University of the Philippines Manila, Philippines
2Department of Ophthalmology, Ospital ng Maynila Medical Center, Manila, Philippines
3Eye Institute, St. Luke’s Medical Center, Quezon City, Philippines
Correspondence: Pablito F. Sandoval Jr., MD
Office Address: Department of Ophthalmology and Visual Sciences, Sentro Oftalmologico Jose Rizal, Philippine General Hospital, University of the Philippines Manila, Taft Avenue, Ermita, Manila, Philippines
Office Phone Number: +63285548400 local 8502
Email Address: pabs.sandoval@gmail.com
Disclosures: The authors report no conflict of interest.
Keratoconus is a combination of the Greek word keras/kerato- (horn) and the Latin word conus (cone). It is a relatively common ectatic disorder wherein progressive thinning and protrusion of the central and paracentral cornea results in a cone- shaped cornea.1
Globally, the prevalence and incidence rates of keratoconus show significant variation. Estimates from different epidemiological studies revealed a global prevalence rate of 0.2% or 4,790 per 100,000 persons and an incidence rate of 1.5% or 25 per 100,000 persons/year.2 Studies from Caucasian populations report a prevalence and incidence rate of 1,000 per 100,000 persons and 2 to 4 per 100,000 persons/year, respectively. Asian and Middle Eastern populations had higher reported prevalence and incidence rates of 1,500 and 5,000 per 100,000 persons and 20 per 100,000 persons per year, respectively.2 The variation in prevalence may be due to environmental factors, as regions with hotter weather and populations that are more exposed to sunlight reported a higher disease prevalence than populations living in cooler climates.3 Prior to this study, there was no locally published data on the prevalence and incidence rates of keratoconus.
Keratoconus manifests mainly as steepening of the cornea, most commonly located inferiorly. Important findings in this disease include thinning of the corneal apex, scarring at the level of the Bowman’s layer, deep stromal stress lines that disappear when pressure is applied to the globe (Vogt’s striae), a ring of iron deposition in the corneal epithelium at the base of the cone (Fleischer’s ring), an arrowhead pattern of light at the nasal limbus when a light beam is shone from the temporal cornea (Rizutti’s sign), and an oil-droplet like reflex in the area of the cone using a direct ophthalmoscope with the pupil dilated (Charleaux’s sign). Other findings include a scissoring reflex on retinoscopy, and protrusion of the lower eyelid on downgaze (Munson’s sign). The abrupt rupture of the Descemet’s membrane with acute overhydration of the cornea may result in corneal hydrops and, over time, an apical corneal scar.4 The presence of corneal scarring on slit-lamp biomicroscopy is strongly associated with advanced disease and higher keratometric readings.
Keratoconus causes severe visual morbidity. When the disease is caught at its later stages, the management becomes more challenging, often needing surgery. Currently, there is no locally published data on the clinical profile of patients with this debilitating disease. This study aimed to describe the clinical profile of patients with keratoconus at the External Disease and Cornea Clinic of the Department of Ophthalmology and Visual Sciences at the Philippine General Hospital (PGH). It focused on population-related features of the disease and how the results can help put into practice methods for early screening, diagnosis, and treatment of keratoconus. Results of this study could serve as the foundation for a keratoconus registry in the country, which will be helpful in priority alignment and policy making.
METHODS
This study was a single-center, retrospective, cross-sectional study involving patients with keratoconus who were evaluated at the External Disease and Cornea Clinic of PGH. Medical records of all patients with keratoconus from January 2015 to August 2022 were reviewed. Eyes diagnosed with keratoconus by an external disease and cornea specialist based on clinical and topographical and/or tomographical changes were included. Eyes with history of ocular surgery prior to the initial consult, medical charts with more than 50% incomplete data or without corneal topography and tomography were excluded from the study.
The following clinical data were recorded: age in years, sex, laterality, history of ocular allergy/atopy, history of eye rubbing, chief complaint, ocular history, refraction history, past medical history, family history, review of symptoms, previous consults, and, if present, reasons for the delay in consult. The following physical findings were recorded: baseline uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), and corrected visual acuity with pinhole (PHCDVA) converted to LogMAR. Best manifest refraction values were recorded. Each eye was staged using the Amsler-Krumeich grading system. In the absence of corneal tomography and pachymetry, the parameters of induced myopia/astigmatism, average K value, and presence of corneal scarring were used in the Amsler-Krumeich grading system. If the eye fitted the criteria of more than 1 stage, it was classified in the higher stage. In addition, presence of the following slit-lamp exam findings were also recorded: papillary conjunctival reaction, corneal stromal thinning, corneal conical protrusion, Fleischer ring, Vogt’s striae, Rizutti’s sign, hydrops, and apical corneal scar. For bilateral cases, each eye was analyzed separately.
When available, print-outs of the Oculus Keratograph (Oculus, Wetzlar, Germany) and Pentacam (Oculus, Wetzlar, Germany) scans were reviewed and the following data were collected: the anterior radius of curvature (Kmax within the 3mm zone in millimeters [mm]), the posterior radius of curvature (Kmax within the 3mm zone in mm), and pachymetry reading at the thinnest area (in microns [μm]). The data from the Pentacam and the PHCDVA were used in disease staging using the Belin ABCD grading system.5 Type of intervention whether medical, refractive (spectacles, soft contact lens, or rigid contact lens), or surgical (collagen cross- linking, implantable intracorneal ring segments, deep anterior lamellar keratoplasty [DALK], penetrating keratoplasty [PKP]), was also collected.
The study was approved by the University of the Philippines Manila Research Ethics Board.
Statistical Analyses
Descriptive statistics such as mean and standard deviation were used for continuous variables including age, UDVA, CDVA, PHDVA in LogMAR, and corneal tomography values. Frequencies and percentages were used for the categorical data variables such as sex, chief complaint, clinical data, type of intervention, and disease severity staging. Statistical tests were performed using the software Stata 13 (StataCorp, Texas, USA).
RESULTS
Forty (40) out of the 63 medical charts with a diagnosis of keratoconus that fulfilled the screening criteria were included. Twenty-three (23) charts were excluded due to incomplete data or absence of corneal topography and tomography. The mean age at first visit was 21.4 ± 4.8 years, with an age range of 11-36 years. Figure 1 shows that most patients were 21 to 30 years of age at the time of first diagnosis with keratoconus. In this study, 29 (72.5%) were males and 11 (27.5%) were females. There were 39 patients (97.5%) who had bilateral disease, and only 1 (2.5%) had unilateral disease. Out of the 39 patients with bilateral disease, 22 (55.5%) were affected asymmetrically, and 17 (42.5%) were affected symmetrically. A total of 79 eyes of 40 patients were analyzed.
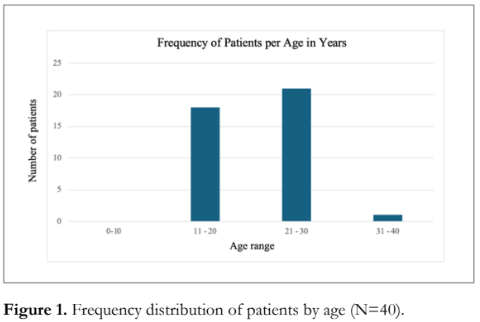
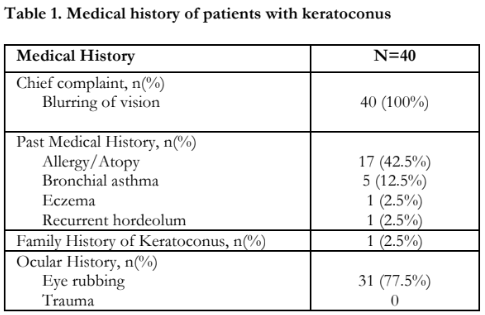
Table 1 lists the medical history of our study patients. Atopy was present in 23 patients (57.5%), with ocular atopy seen in 17 (42.5%) patients, bronchial asthma in 5 (12.5%) patients, and eczema in 1 (2.5%) patient. History of vigorous eye rubbing was present in 31 (77.5%) patients. Only 1 (2.5%) had a positive family history of keratoconus.
The average time from onset of symptoms to consult at PGH was at 46.4 ± 33.4 months. Half (n=20) had prior consults elsewhere where the diagnosis of keratoconus was missed. Of these, 17 had a previous diagnosis of error of refraction and were managed with spectacles, and 3 were previously diagnosed with amblyopia. Seventeen (42.5%) had no previous ophthalmologic consult.
Table 2 shows the visual acuity at initial visit. The mean UDVA of patients was LogMAR 1.0 ± 0.5 (Snellen equivalent of 20/219). Mean CDVA was LogMAR 0.6 ± 0.4 (Snellen equivalent of 20/78). Mean PHCDVA was LogMAR 0.5 ± 0.4 (Snellen equivalent of 20/59). The mean spherical refraction was -5.2 D ± 6.4 D with a range of +12.0 D to -20.5 D. The mean cylindrical refraction was -4.6 D ± 3.3 D, with a range of -0.5 D to -11.5 D. Mean spherical equivalent was at -7.5 D ± 7.0 D (range +5.3 to -26.5 D).
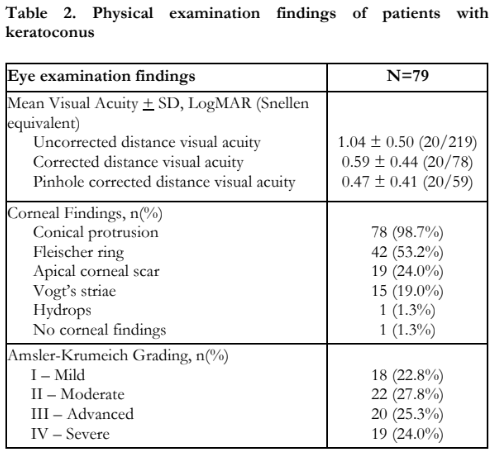
Corneal protrusion was seen in 78 eyes (98.7%) [Table 2]. Other biomicroscopic findings were Fleischer ring which was present in 42 eyes (53.2%), apical corneal scar seen in 19 eyes (24%), and Vogt’s striae seen in 15 eyes (19%) [Table 2]. Only 1 eye (1.3%) had hydrops at the time of consultation. Papillary conjunctival reaction was seen in 40 eyes (50.6%). Only one eye (1.3%) had no corneal findings.
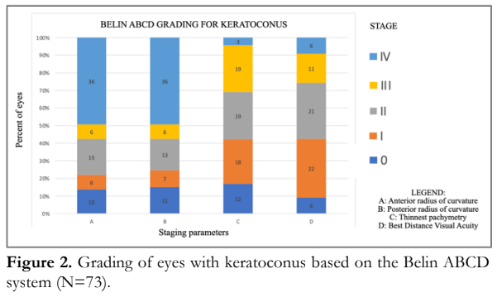
Table 2 also shows the distribution of eyes according to keratoconus severity based on the Amsler-Krumeich grading system. Notably, 39 eyes (49.3%) were classified as advanced-severe keratoconus. There were 73 (92.4%) eyes that had Pentacam results. Figure 2 shows the staging of keratoconus using the Belin ABCD grading system. Half (n=36) of eyes presented with steep anterior curvatures of >55.0D or <6.15mm (Stage IV). Half (n=36) had a steep posterior radius of curvature >68.5D or <4.95mm (Stage IV). A third (n=22) (30%) had a corneal thickness of <400μm (Stage III, IV). Seventeen eyes (23%) had a best distance visual acuity of less than 20/100 (Stage III, IV).
Half of the patients (n=20) received medical treatment in the form of topical antihistamine-mast cell stabilizer for allergic conjunctivitis. Another 3 patients (7.5%) received topical steroids for conjunctival inflammation. One patient (2.5%) received topical hypertonic saline solution for the corneal hydrops. Rigid contact lens was planned for 60 eyes (75.9%) and spectacle correction for 2 eyes (2.5%). Sixty-two eyes (78.5%) were candidates for collagen cross-linking. There were 10 eyes (12.7%) for deep anterior lamellar keratoplasty and 2 eyes (2.5%) for penetrating keratoplasty.
DISCUSSION
Keratoconus is an ectatic corneal disease that may lead to significant visual morbidity. Our study demonstrated the clinical profile of 40 patients with keratoconus. The demographic profile of our patients was similar to that reported in other Asian countries.3,6-8 The mean age of patients at diagnosis was typically in the second to third decade of life.3,6- 10 In a study done in India, the mean age of patients at diagnosis was 20 years, which is comparable to the Asian population but lower than Western counterparts.3 The average age of patients at the time of diagnosis was similar to the clinical profile reported in China, Nepal, and India, but was younger than that seen in Iran, the United Kingdom (UK), and United States (US).3,6-10 Similar studies also reported a male predilection of the disease.3,6-10 Almost all of the patients seen at our institution had bilateral disease. This data was comparable to the profile of patients seen in Iran, India, and the UK. This phenomenon was probably due to the long duration from the onset of symptoms to consultation.3,6-10
Vigorous eye rubbing is known to be a common associated risk factor for keratoconus. Our results showed that 77.5% of patients reported vigorous eye rubbing. This percentage was comparable to that reported in China and was higher than the ones reported in India, UK, and the US.3,6,9,10 In our study, atopy was present in almost half of the patients, with papillary conjunctival reaction present in 50.6% of the eyes, which was also comparable to the studies in India, the UK, and the US.3,9,10 Family history remains to be a controversial risk factor in keratoconus.3,6,9,10 Only 1 patient in this study had a family history of keratoconus.
The mean interval from onset of symptoms to consult at PGH was at 46.4 ± 33.4 months. In half of the patients, the diagnosis of keratoconus was missed by prior eye care professionals. Most of the patients were previously diagnosed with error of refraction (50%), and a few with amblyopia (7.5%). The patients sought consult or were referred to our institution when the visual acuity was severely affected. During the interval between the time of onset of symptoms and consult at our institution, no ophthalmologic diagnostic tests were performed. This points to a big gap in knowledge regarding keratoconus in the community, which may have led to delays in diagnosis and management.
Only one eye included in this study had no corneal findings on slit-lamp examination and was diagnosed using corneal tomography. In India, 7% of keratoconus patients had no corneal signs on slit- lamp biomicroscopy, while 14% and 15% in American and European studies, respectively, did not present with clinical findings.3,9,10 This result means that we were diagnosing patients with keratoconus at a more advanced stage than our international counterparts. Vogt’s striae and Fleischer ring are the two most common slit-lamp examination findings in keratoconus.3,9,10 Vogt’s striae were present in just 19% of our study eyes, lower than the findings seen in other studies.3,9,10 The presence of Fleischer ring was comparable to international studies.3,9,10 The presence of apical corneal scarring in 24% of eyes was comparable to that seen in the UK study but was higher than in India.3,9,10
Based on disease severity using the Amsler- Krumeich grading system, 49.3% of eyes seen at our institution were classified as advanced-severe. This percentage was comparable to that of US patients, but was higher than those seen by our Asian counterparts.3,6,7,8,10 In India and Iran, most of the patients presented with moderate keratoconus.3,7 Nepal, however, reported almost an equal distribution of patients with regard to disease severity.8
Our reported mean PHCDVA was similar to those of other Asian countries such as Iran (20/39) and Nepal (20/59). The mean refraction, however, was higher compared to the findings in both countries.7,8 The higher myopic refraction seen in our institution was probably due to the higher percentage of patients presenting with advanced-severe stages of keratoconus.
In comparison to the Amsler-Krumeich grading system, the Belin ABCD grading utilizes corneal tomography to separately classify the posterior corneal curvature where early signs of keratoconus can be seen before anterior corneal curvature changes. If corneal tomography is available, staging using Belin ABCD grading is useful in determining the disease progression of keratoconus and corneal changes after cross-linking.11 Based on the Belin ABCD grading, half of the eyes seen were classified as A4 and B4. The most frequent stages of corneal pachymetry were C2 and C3. The most frequent stage of visual acuity was D1. These results were comparable to those of a study done in Germany where more eyes were classified as A4, B4, and D1.11 However, the corneal pachymetry results in this study were thinner than those of the German study where most eyes were classified as C0.11
Panelists from the Global Consensus on Keratoconus and Ectatic Diseases stressed the use of corneal cross-linking in patients with progressive ectasia, regardless of age or level of vision.12 In our study, 62 (75.9%) eyes were candidates for collagen cross-linking. Eyes with significant apical corneal scarring that were for keratoplasty and eyes with less than 400um thinnest corneal pachymetry prior to the sub-400 μm protocol in 2021 were not advised to undergo collagen cross-linking.13 DALK remains the preferred surgical procedure unless there is a compromise in the Descemet’s membrane.
One of the study limitations was its smaller sample size compared to other published studies. Moreover, since this study was conducted in a tertiary national university referral hospital, the results may not necessarily reflect the actual disease profile in the community. The cases seen and referred to our institution were usually in advanced stages. Information that can be provided from retrospective studies is inherently limited to the data available in the medical charts. This underscores the need for a keratoconus registry in the country.
In conclusion, this study shows that keratoconus was most frequently seen in young male patients and asymmetrically affects both eyes. Patients seen at PGH had keratoconus at a more advanced stage compared to patients in other countries. Improving awareness on keratoconus among the general public and eye health professionals may facilitate earlier detection of the disease.
ACKNOWLEDGEMENTS
The authors thank the Department of Ophthalmology and Visual Sciences of the University of the Philippines Manila – Philippine General Hospital for the support in making and completing this paper.
REFERENCES
- Hashemi H, Heydarian S, Hooshmand E, et al. The Prevalence and Risk Factors for Keratoconus: A Systematic Review and Meta-Analysis. Cornea 2020;39(2):263-270.
- Santodomingo-Rubido J, Carracedo G, Suzaki A, et al. Keratoconus: An updated review. Cont Lens Anterior Eye. 2022;45(3):101559.
- Agrawal VB. Characteristics of keratoconus patients at a tertiary eye center in India. J Ophthalmic Vis Res. 2011;6(2):87-91.
- Sugar J, Garcia-Zalisnak D. Keratoconus and Other Ectasias. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019: v. 4, chap. 18: 254-257.
- Belin MW, Kundu G, Shetty N, et al. ABCD: A new classification for keratoconus. Indian J Ophthalmol 2020;68(12):2831-2834
- Yang K, Xu L, Fan Q, et al. A hospital-based study on clinical data, demographic data and visual function of keratoconus patients in Central China. Sci Rep. 2021;11(1):7559.
- Rafati S, Hashemi H, Nabovati P, et al. Demographic profile, clinical, and topographic characteristics of keratoconus patients attending at a tertiary eye center. J Curr Ophthalmol. 2019;31(3):268-274.
- Rana RS, Bajracharya L, Gurung R. Clinical Profile on Keratoconus Presenting at A Tertiary Eye Care Centre- Tilganga Institute of Ophthalmology. Nepal J Ophthalmol 2019;11(22):138-144.
- Weed K, MacEwen C, Giles T, et al. The Dundee University Scottish Keratoconus study: demographics, corneal signs, associated diseases, and eye rubbing. Eye 2008; 22:534–541.
- Zadnik K, Barr JT, Edrington TB. Corneal scarring and vision in keratoconus. A baseline report from the Collaborative longitudinal evaluation of keratoconus study (CLEK). Cornea 2000;19(6):804–812.
- Flockerzi E, Xanthopoulou K, Goebels SC, et al. Keratoconus staging by decades: a baseline ABCD classification of 1000 patients in the Homburg Keratoconus Center. Br J Ophthalmol 2021;105(8):1069- 1075.
- Gomes J, Tan, D, Rapuano, Christopher J, et al. Global Consensus on Keratoconus and Ectatic Diseases. Cornea 2015;34(4):359-369.
- Hafezi F, Kling S, Gilardoni F, et al. Individualized Corneal Cross-linking With Riboflavin and UV-A in Ultrathin Corneas: The Sub400 Protocol. Am J Ophthalmol 2021;224:133-142.

