Clinical Profile and Outcomes of Ocular Dermoid Cysts at the Philippine General Hospital
Justin Alan A. Yao, MD1, Mary Ellaine S. Diaz, MD1, Ruben Lim Bon Siong, MD1,2
1Department of Ophthalmology and Visual Sciences, University of the Philippines-Philippine General Hospital, Manila, Philippines
2Eye Institute, St. Luke’s Medical Center, Quezon City, Philippines
Correspondence: Justin Alan A. Yao, MD
Office Address: Department of Ophthalmology and Visual Sciences, Sentro Oftalmologico Jose Rizal, University of the Philippines– Philippine General Hospital, Taft Avenue, Ermita, Manila, 1000 Philippines
Office Phone Number: +63285548400 local 8502
Email Address: jayao@up.edu.ph
Disclosures: The authors report no conflict of interest.
Ocular dermoid cysts are the most common congenital ocular masses in children, occurring in 1- 3 per 10,000 births.1 They are considered to be a form of slow-growing, congenital, cystic teratomas from epidermal inclusions due to defective embryonal facial cleft closure. They may also be classified as choristomas, which are normal embryonic tissues located in an abnormal site.2 Although these dermoid cysts are all firmly adherent to the globe itself, they often vary in size, location (corneal/epibulbar, or limbal), and composition.1 They may include appendices such as hair follicles, sebaceous glands and sweat glands, nerves, smooth muscle, fat, fibrous tissue, and blood vessels.
Ocular dermoid cysts may present as an isolated lesion, but they may also be associated with other congenital malformations. One commonly identified pattern of association is that of Goldenhar syndrome, which are dermoid cysts that appear in conjunction with malformations of the ear (e.g., pre-auricular appendages, pretragal fistulas), face, skull, and vertebrae.1,3 Goldenhar syndrome has recently been classified as the oculo-auriculo-vertebral spectrum of craniofacial microsomia.1
Due to variability in presentation of ocular dermoid cysts, their degree of severity can also differ. Most commonly, they are usually solitary, unilateral lesions that straddle the limbus at the inferotemporal quadrant.3 Small and peripherally located dermoids may not significantly affect visual acuity and may be treated conservatively; or they may be removed for cosmetic reasons. However, larger or more centrally located dermoids may influence development of problems such as sensory deprivation amblyopia, high astigmatism (>1.5D), ocular motility problems, as well as significant deformity.1 If these conditions are present, surgical management can be considered.4
A wide variety of surgical techniques may be employed for dermoids. Among the major considerations as to which technique to employ would be the depth, size, and location of the lesion. These can range from simple shave excision or superficial keratectomy, to more complicated procedures such as excision with corneal tattooing and limboconjunctival autografting, amniotic membrane transplant, and lamellar (i.e., deep lamellar anterior keratoplasty) or penetrating keratoplasty.2,5,6,7 Adequate cosmetic results may be achieved from complete excision of the lesion; however, the possibility remains that the bed may opacify over time. It is also important to note that the patient’s amblyopia may still persist depending on the timing of the surgery.
At the Philippine General Hospital (PGH), the variability of presentation of patients with ocular dermoid cysts seems to hold true. Some patients are brought in for consultation as early as during their neonatal stage, while some patients have their initial consults in their teenage years. In a local study reviewing the different tumors of the eye and ocular adnexa, dermoids were determined to be the second most common type of benign conjunctival tumors.8 There was no overwhelming sex predilection, and a large majority of patients presented with unilateral lesions only.8 However, the study did not mention whether the dermoids were seen as an isolated finding, or whether there were other associated systemic malformations or treatments done and what their outcomes were. The aim of this study was to describe the clinical profile and outcomes of patients with ocular dermoid cysts who were seen at the PGH.
METHODS
This was a single-center, retrospective, cross- sectional study conducted at the External Disease & Cornea (ED/Cornea) Clinic of the Department of Ophthalmology and Visual Sciences, PGH utilizing medical records of patients diagnosed with ocular dermoid cysts from January 2012 to June 2023. This study was approved by the University of the Philippines Manila Research Ethics Board and was conducted in compliance with the World Health Organization Standards and Operational Guidance for Ethics Review of Health-related Research with Human Participants (2011), the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (2016), and the National Ethical Guidelines for Health and Health-related Research (2017).
The list of potential study participants was obtained by reviewing the census of the ED/Cornea Clinic and the surgical pathology logbooks of the Philippine Eye Research Institute (PERI). Records of patients of the ED & Cornea Clinic, PGH with clinical and/or histopathological diagnosis of ocular dermoid cyst were included. Records with more than 50% missing data and those with any concomitant corneal, neuro-ophthalmic, glaucomatous or retinal pathology, and other ocular conditions unrelated to ocular dermoid cysts were excluded. In addition to reviewing their ED/Cornea records, patients’ data in the other co-managing ophthalmology subspecialty clinics (Pediatric Ophthalmology and Strabismus Clinic, Plastic-Lacrimal Clinic, and the Orbit Clinic) were also reviewed, when available.
The following clinical data were collected from the initial clinic visit: sex, age at initial consultation at the ED/Cornea Clinic, reason for delayed consult, best-corrected visual acuity (BCVA), refraction, other ocular/congenital malformations, and dermoid characteristics (laterality, size, and location). For those who underwent surgery, the surgical procedure done was noted, the histopathological reports from PERI were reviewed, and the final diagnosis was recorded. The rest of the patient records were reviewed, with pertinent information, such as the recurrence of the dermoid or development of other ocular findings, listed down. The findings at the most recent consultation were recorded, which include refraction, BCVA, as well as presence of amblyopia. Duration of their entire treatment course was also noted.
Visual acuity (VA) was converted to LogMAR. For pre-verbal pediatric patients, visual acuity of “positive dazzle/reacts to light” and “central, steady, maintained” (CSM) were assigned corresponding LogMAR values of 1.30 and 0.30, respectively.9,10 In this study, amblyopia was defined as having visual acuity ≤20/30 (LogMAR ≥0.18).11,12 Improvement of VA was defined as an increase in Snellen VA by at least 1 line on the latest visit compared to the initial consult, while worsening of VA was defined as a decrease in Snellen VA by at least 1 line on the latest visit compared to the initial consult.
Statistical Analyses
Patient characteristics were summarized. Data wrangling and statistical analyses were performed in R and RStudio (Version 2023.09.1+494). Continuous variables with normal distribution were presented as means with standard deviations (SD); otherwise, median with interquartile range [Q1, Q3] were presented. Key variables were tested for normality by examination of distribution and QQ plots. Categorical variables were presented as counts and percentages (%). All possible categories were presented, and missing values were provided for truly missing data. To assess the difference in BCVA on follow-up between patients managed non-surgically compared to patients surgically, Wilcoxon rank-sum non-parametric test was performed. BCVAs were grouped into LogMAR value categories where the difference between non-surgical and surgical patient groups was tested using Fisher exact test. Hypothesis testing p-value <0.05 for two-tailed comparisons was considered statistically significant.
RESULTS
A total of 63 medical records were identified. Forty-seven (47) were paper charts and 16 were passcode-protected electronic medical records (EMR). Of the 47 paper charts, only 22 records were located. A total of 38 records or 60% (38/63) were included for review.
Forty-two (42) eyes of 38 patients were analyzed in this study. A summary of their baseline characteristics is presented in Table 1. The mean age at initial consultation at the ED/Cornea Clinic was 8.3 + 7.5 years old (range 3 weeks to 28 years old). Mean duration of symptoms prior to consult was 99 + 89 months (range 0.75 to 342 months). No sex predilection was observed with 20 male (52.6%) and 18 female (47.4%) participants. Majority of participants (n=20 or 52.6%) were seen by other doctors prior to being referred or deciding to seek consult at PGH. Thirty-four (34) or 89.5% of the dermoids were unilateral, with an almost even distribution between right (47.4%) and left (42.1%) eyes. Bilateral dermoids were only seen in 4 patients (10.5%). Twenty-four (24) participants (63.2%) had BCVA of LogMAR >0.18 and 14 participants (36.8%) had BCVA of LogMAR ≤0.18 on initial consult. Mean duration of follow-ups was at 14.8 + 21.5 months, ranging from 0 months (single visit only) to 91 months.
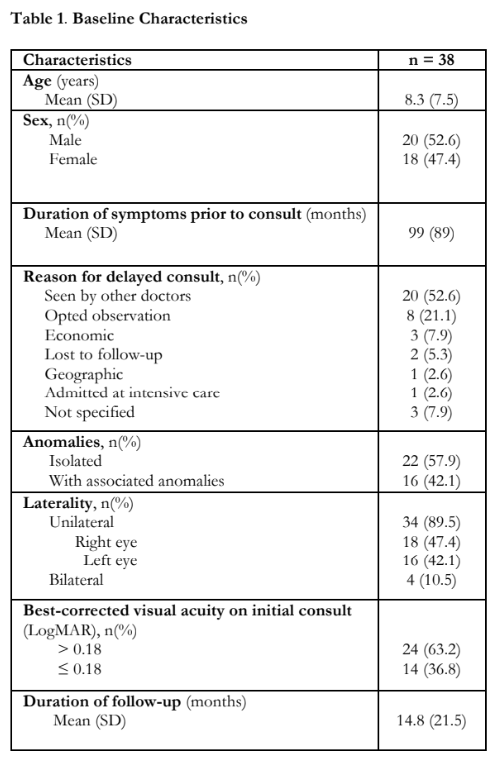
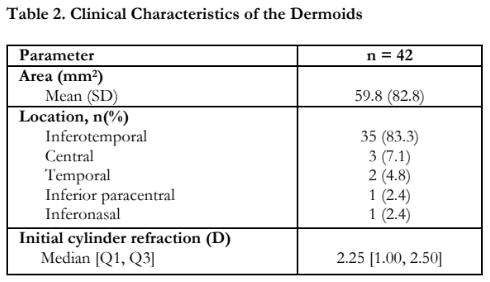
Table 2 shows the clinical characteristics of the dermoids. Mean area was 59.8 mm2, (range 3 to 400 mm2). No area measurements were obtained for 9.5%. A large majority of the dermoids were located at the inferotemporal quadrant (35/42 or 83.3%). The median astigmatism on initial refraction was 2.25 diopter (D) cylinder, ranging from 0.00 D to 11.00 D. Initial refraction was not done for 38.1% on initial consult.
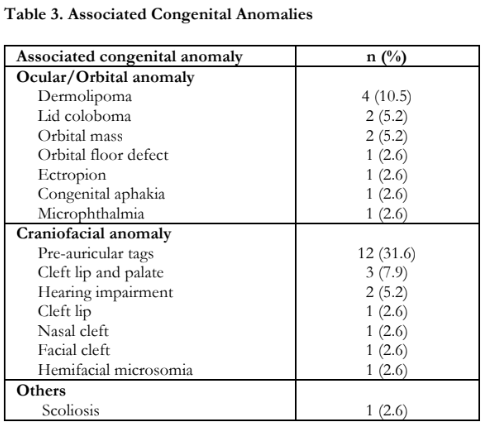
Twenty-two (22) or 57.9% of the patients presented with isolated dermoids, while 16 (42.1%) had associated congenital anomalies. The congenital anomalies identified in the patients are presented in Table 3. Dermolipomas (10.5%) were the most commonly observed ocular congenital anomaly, while pre-auricular tags (31.6%) were the most common craniofacial congenital anomaly. Of note, all 4 participants who had bilateral dermoids had other congenital anomalies.
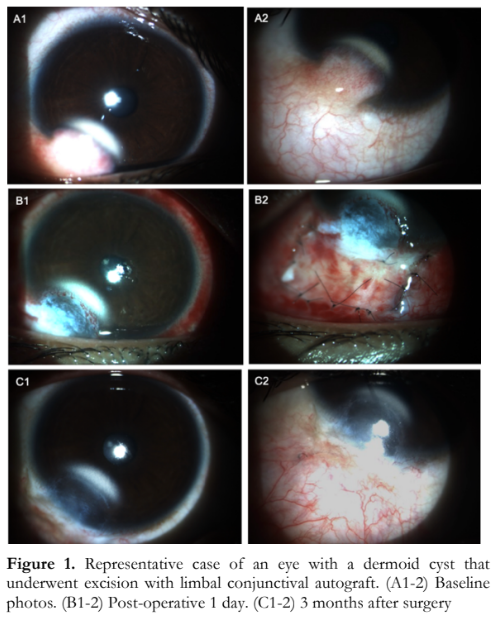
Among the 38 patients, 25 (65.8%) underwent surgery. All 4 bilateral cases underwent surgery (2 bilateral surgery, 2 unilateral surgery). A total of 27 specimens were sent for histopathology. Mean age at surgery was 8.6 years, ranging from 3 months to 28 years old. Mean interval between initial consult and surgery was 8 months (range 1 week to 36 months). As shown in Table 4, the most common initial surgical procedure performed was excision with limbal conjunctival autograft (48.1%), followed by simple excision with or without corneal tattooing (29.6%). Pictures of a representative case are shown in Figure 1.
Of the 25 participants who underwent surgery, the mean duration of follow-up after surgery was 12.1 months (range 2 weeks to 82 months). Fourteen (14) patients or 56.0% had a postoperative follow-up duration of at least 3 months. Out of the 27 eyes that underwent surgery, there were 2 documented cases of recurrence of the dermoid. One recurrence was noted 62 months after the initial surgery, while the other recurrence was noted 4 months after surgery. Pseudopterygium was noted in 5 of the patients who underwent simple excision without limbal conjunctival autograft (Table 4).

Among the 27 eyes that underwent surgery, 26 (96.3%) had a final histopathological diagnosis of dermoid. One specimen was identified as a fibroepithelial polyp.
Of the 27 eyes that underwent surgery, 22 (81.5%) had a LogMAR BCVA >0.18 and 5 (18.5%) had a LogMAR BCVA ≤ 0.18 on follow-up visit. Among the 15 eyes that did not undergo surgery, 5 (33%) had a LogMAR BCVA >0.18 and 2 (13.3%) had a LogMAR BCVA ≤0.18 on follow-up visit. Although 8 patients (53.3%) in the no surgical intervention group did not have any follow-up visits with repeat BCVA, majority of patients who had follow-ups had no change in their BCVA (5 or 33.3%). In the surgical intervention group, 11 patients (40.7%) had no change in BCVA, while 8 patients each (29.6%) had improved or worsened BCVA.
For the patients in the no surgical intervention group, the latest median cylinder refraction was -0.50 D cyl, ranging from 0.00 D to -4.00 D. Majority in this group also had no change in cylinder refraction from baseline to their last visit. In the surgical group, the most recent median cylinder refraction was -2.00 D, ranging from -0.50 D to -8.00 D. There was a decrease in the cylinder refraction in 4 (36.4%) patients who underwent surgery, however 16 (59.3%) patients did not have refraction repeated during their latest post-operative consultation. These values are seen in Table 5.

The BCVA for the no surgical intervention group was missing on follow-up in 8 (53.3%) patients. Cylinder refraction on follow-up was missing in 11 (73.3%) patients in the no surgical intervention group and 16 (59.3%) of patients in the surgical intervention group. Baseline cylinder refraction for comparsion with follow-up refraction was not done in 1 (25%) participant in the no surgical intervention group and 5 (45.5%) patients in the surgical intervention group.
DISCUSSION
This study described the clinical profile and outcomes of 38 patients with ocular dermoid cyst seen in a single referral center in the Philippines over a 2012-2023 period. Our study findings showed an almost even distribution among the male and female participants. This is in contrast to several studies that demonstrated a female preponderance in the occurrence of dermoids.1,4,13 Only one study did not find sex predilection among the 50 participants.14
Majority (89.5%) of the lesions in our study were unilateral, with an almost even distribution between the right and left eye. Most of them were also noted in the inferotemporal quadrant (83.3%). This is similar to the findings reported by del Rocio Arce Gonzales et al. and by Nevares et al., although specific laterality and location of corneal dermoids were not reported in both studies.4,14 In contrast, a study by Walker et al. revealed a larger proportion of patients with bilateral lesions at 21% with only 47% located at the inferotemporal position.1
In our study, 42.1% of the patients presented with other congenital anomalies apart from the dermoid, which is similar to other studies.4,14 Goldenhar syndrome, also known as craniofacial microsomia (CFM), was found to be the most common syndromic association in three previous studies.1,4,14 In this study, however, not all patients with findings consistent with Goldenhar syndrome have received formal diagnosis, but they have been referred to the Pediatric Department for further systemic evaluation. Dermolipoma was the most common associated ocular/orbital anomaly in our study. Other studies reported eyelid colobomas and oblique astigmatism as the most common ocular anomaly.1,14 Lastly, the most common associated craniofacial anomaly in our study was pre-auricular tags, which was similar to the Walker study.1 Pirouzian et al. described an anatomic grading classification of dermoids to aid in the approach of these patients.5 Grade I dermoids are superficial lesions localized to the limbus that measure less than 5 mm. Grade II dermoids are larger lesions that span most of the cornea and extend deep into the stroma to the Descemet membrane without its involvement. Lastly, grade III dermoids are lesions that involve the entire cornea that extend up to the pigment epithelium of the iris. Based on the descriptions and figures on the medical records, a large number of the dermoids seen in our study would appear to be classified as Grade I lesions in terms of the perilimbal location or Grade II in terms of the size. However, this classification cannot be applied retroactively due to the lack of descriptions pertaining to the depth of the lesions. The young age of some of the patients precludes examination of the lesion, especially when ascertaining depth of involvment. In these cases, intraoperative ultrasound biomicroscopy (UBM) has been recommended during the surgical planning. It is not routinely done at our institution.
On presentation, 63.2% of patients had a visual acuity of LogMAR >0.18, corresponding to a Snellen VA of worse than 20/30. Regardless of treatment done, whether non-surgical or surgical, only 7 patients (23.3%) had a visual acuity of LogMAR ≤0.18 during their follow-up. This may be due to the relatively small number of patients who underwent amblyopia management and the inadequate follow- up period of several patients in order to detect the effect of the amblyopia therapy. Moreover, a study by Hussein and colleagues showed poor initial VA of ≤20/200 (LogMAR ≥1.00) and astigmatism of ≥1.50 D were risk factors for functional failure of amblyopia therapy. They also stated that increased treatment failure risk was also noted if intervention was instituted after 6 years of age.15 In our cohort, majority had astigmatism of greater than -1.50 D and 8.3 years was the mean age of the patients.
We also noted no improvement in the astigmatism of our post-surgery cohort. This is similar to the study by Fan and colleagues wherein no statistically significant change was found in baseline astigmatism of the 66 patients with ocular dermoids who underwent lamellar keratoscleroplasty.16 It has been postulated that the long-standing molding or alteration in the corneoscleral wall anatomy from the growth of the dermoid results in mass-induced astigmatism that cannot be fully corrected after surgery.
Although dermoids are lesions that are not typically known to recur, there were 2 documented cases of recurrence of the dermoid in our study. One recurrence was noted 62 months after the initial surgery, while the other recurrence was noted 4 months after. There were also 2 patients who had unilateral recurrent dermoids that had previously undergone surgery at other facilities. Pseudopterygium was also noted in 5 patients who underwent surgery, all of which had excision without limbal conjunctival autograft. Other complications that have been reported in literature include persistent epithelial defects, dellen, peripheral corneal neovascularization, and scarring due to a focal limbal stem cell deficiency.13
Jeong and colleagues described a surgical technique wherein excision of grade I dermoids was combined with corneal tattooing and sutureless limbal conjunctival autograft.13 The endpoints of this surgery were complete removal of the lesion while maintaining the corneoscleral plane and masking the residual corneal opacity with ink. Conjunctival defects that ensued after the surgery were covered by a conjunctival patch graft from the superior conjunctiva and secured using fibrin glue. A bandage contact lens was applied and maintained for 1-2 weeks. Out of 24 patients who underwent this procedure, there was only one case of recurrence of a pre-operative pseudopterygium over 3 years.
At our institution, simple excision with or without corneal tattooing was performed on 7 cases from 2012 to early 2019. From 2019, there was a shift in the surgical technique to include limbal conjunctival autograft due to a presumed focal limbal stem cell deficiency at the area of the dermoid. Since then, with the exception of 2 cases, 15 cases had limbal conjunctival autografting done.
Despite the inherent limitations of retrospective studies specifically on the completeness of clinical information, our data showed that ocular dermoids seen at the PGH had no strong sex predilection. Most were isolated, unilateral masses at the inferotemporal limbus resulting in significant astigmatism and amblyopia which are the frequently reported visual complications of ocular dermoids. Due to incomplete data on BCVA and refraction on presentation and on follow-up of a lot of the patients, an accurate conclusion regarding improvement or worsening of BCVA with or without surgical intervention cannot be drawn. Nevertheless, we highly recommend that aggressive amblyopia management be instituted especially in the early pediatric age group. Referral to pediatric ophthalmologists for co-management will be helpful. For surgical management, excision with limbal conjunctival autograft should be the procedure of choice to prevent the subsequent development of pseudopterygium.
ACKNOWLEDGMENT
Appreciation is extended to Greco Mark B. Malijan, MD, MSc for his invaluable assistance with the statistical analysis of this study.
REFERENCES
- Walker BA, Saltzman BS, Herlihy EP, Luquetti DV. Phenotypic characterization of epibulbar dermoids. Int Ophthalmol 2017;37(3) 499–505.
- Villalón ML, Leal MDLÁ, Chávez JR, et al. Recurrent epibulbar dermoid cyst treated with amniotic membrane implant a case report. BMC Surg 2018;18:98.
- Baum JL, Feingold M. Ocular aspects of Goldenhar’s syndrome. Am J Ophthalmol 1973; 75(2):250–257.
- del Rocio Arce Gonzalez M, Navas A, Haber A, et al. Ocular dermoids: 116 consecutive cases. Eye Contact Lens 2013;39(2):188–191.
- Pirouzian A. Management of pediatric corneal limbal dermoids. Clin Ophthalmol 2013;7: 607–614.
- Jeong J, Song YJ, Jung SI, Kwon JW. New surgical approach for limbal dermoids in children: Simple excision, corneal tattooing, and sutureless limboconjunctival autograft. Cornea 2015;34(6):720–723.
- Choudhary DS, Agrawal N, Hada M, Paharia N. Massive corneal-epibulbar dermoid managed with pre-descemetic DALK and SLET. GMS Ophthalmol Cases 2021;11:Doc05.
- Domingo RED, Manganip LE, Castro RM. Tumors of the eye and ocular adnexa at the Philippine Eye Research Institute: A 10-year review. Clin Ophthalmol 2015:9:1239– 1247.
- Lyons CJ, Lambert SR. Taylor and Hoyt’s Pediatric Ophthalmology and Strabismus, 6th ed. India: Elsevier, 2023; 42.
- Kothari M, Bhaskare A, Mete D, et al. Evaluation of central, steady, maintained fixation grading for predicting inter-eye visual acuity difference to diagnose and treat amblyopia in strabismic patients. Indian J Ophthalmol 2009;57(4):281-284.
- Zagui, RMB. Amblyopia: Types, diagnosis, treatment, and new perspectives. June 25, 2019: https://www.aao.org/education/diseasereview/amblyopi a-types-diagnosis-treatment-new-perspectiv (accessed February 1, 2024).
- Williams C. Amblyopia. BMJ Clini Evid 2009; 0709.
- Jeong J, Rand GM, Lee JY, Kwon, JW. Novel limbal dermoid surgery for visual acuity and cosmesis improvement: A 7-year retrospective review. PloS one 2023;18(6): e0286250.
- Nevares RL, Mulliken JB, Robb RM. Ocular dermoids. Plast Reconstr Surg 1988;82:959-964.
- Hussein MA, Coats DK, Muthialu A, et al. Risk factors for treatment failure of anisometropic amblyopia. J AAPOS 2004 Oct;8(5):429-34.
- Fan X, Hong J, Xiang J, et al. Factors predicting long-term changes in refraction after lamellar keratoscleroplasty in children with limbal dermoids. Eye 2021;35(6):1659–1665.

