Capacity to Treat Retinoblastoma in the Philippines
Sandra Joan Worak-Tan MD1 , Ma. Theresa B. Sampang MD1 , Maria Victoria A. Rondaris MD2
1Department of Health Eye Center, East Avenue Medical Center, Quezon City
2University of Santo Tomas Hospital, Manila
Correspondence: Sandra Joan Worak-Tan MD1
Clinic Address: Department of Health Eye Center, East Avenue Medical Center, East Avenue, Quezon City Email Address: Sandee.worak@gmail.com
Clinic Phone Number: +639190043979
Disclosure: All authors report no financial disclosures or conflict of interest.
Retinoblastoma (RB) is the most common intraocular tumor in the pediatric age group. It has a published cure rate of more than 90% in high-income countries where diagnosis is made early.1 However, in low-to middle-income countries (LMIC), like the Philippines, late diagnosis and treatment delays are common, lowering the chance of survival to 50- 70%.2 The average diagnostic lag time of more than 3 months was 72.6% in unilateral cases and 50.9% in bilateral cases among RB patients studied at the Philippine General Hospital from 1998-2008.3 Other reasons for decreased survival rate in LMICs are inaccessibility to capable hospitals, misdiagnosis, referral delay, cultural beliefs, treatment abandonment, or receiving no treatment at all.
The Philippines is an archipelago consisting of 7,641 islands, divided into 17 regions wherein the greatest number of hospitals are located in the National Capital Region (NCR).4,5 Consequently, specialists are predominantly found in the NCR as well. Inaccessibility of RB healthcare to patients from farther regions adds to the disease burden. In addition, the Philippines, currently, does not have a national standard of care on RB yet. Treatment protocols are instituted in only a few hospitals.
Treatment capacity involves a multitude of factors that address every stage of RB care. It is the capability of a hospital to manage RB through the use of the available key personnel and technology in their institution. It also involves the utilization of information learned from experience and continuing education to properly treat RB. Treatment of RB necessitates a multidisciplinary approach, from diagnosis to treatment and rehabilitation. The St. Jude Children’s Research Hospital has formed a Retinoblastoma Global Alliance Group with members from certain hospitals from each continent, with Philippines as a member. The purpose of this alliance is to help each other improve on the knowledge and ability to treat RB patients. They were the first authors of an assessment survey done describing the capacity of the Middle Eastern Region in the management of RB. This survey served as a guide in this study.6
The Cancer Control Division of the Department of Health (DOH) formed a technical working group last 2021 to create a National RB Program to control RB cases in the Philippines. However, further research on the existing assets and gaps in knowledge is still needed. This study aimed to determine the capacity to treat RB in the Philippines by identifying hospitals that have the necessary human resources and technology in treating the patients. Hospitals under the DOH are known for delivering affordable and accessible healthcare across the country. Tertiary hospitals that are not under the DOH are also expected to have the infrastructure necessary for the treatment of different cancers. This study identified the different capacities of these hospitals that facilitate development of the different resources needed for the management of RB in each region. A referral network among the hospitals from the different regions can be created to serve as a guide for patients and attending physicians for a more timely and efficient diagnosis and treatment.
METHODS
This study was a cross-sectional analysis on the treatment capacity of RB in the country. This study was approved by the Institutional Ethics Review Board of the East Avenue Medical Center. It was conducted using an online questionnaire generated with the Qualtrics survey software (Qualtrics, Provo, UT). All Level 1, 2 and 3 hospitals, published in the DOH Hospital Profile directory, government-owned and controlled corporation (GOCC) hospitals and Level 3 private and public hospitals classified as tertiary hospitals, listed in the PhilHealth-accredited list of hospitals as of September 2021 were included.7,8 Four specialized hospitals that catered to specific patient-populations outside of ophthalmologic service were excluded from this study.
The questionnaire was taken from the St. Jude Children’s Research Hospital (U.S.A) Global Needs Assessment Survey which was used in the RB assessment study in the Middle Eastern region. The authors modified this questionnaire based on the availability of resources in our local setting and objective of the study. There was a total of 20 multiple choice questions and 3 dichotomous questions. The survey consisted of 3 main categories namely, (1) human resource capacity, (2) treatment capacity, and (3) education and network capacity. Human resource capacity had a follow-up question on each available key physician and hospital support staff, as to their availability on-site or in another hospital (off-site). For treatment capacity, availability, frequency of use, and confidence in using diagnostic modalities such as computed tomography (CT) scan, magnetic resonance imaging (MRI), ocular ultrasound (B-scan), pediatric retinal imaging, lumbar puncture, and grossing of specimens were assessed. Different routes of chemotherapy, as well as enucleation, ocular prosthesis, focal laser therapy, radiation therapy and autologous stem cell harvest were also evaluated. Level of confidence in using these modalities was measured as very confident, somewhat confident and not confident. Education and network capacity of the hospitals included the presence of clinical training program of specialists involved in RB care and ability to communicate with the multiple stakeholders involved in care of RB patients. The three dichotomous survey questions were about community awareness.
The survey link and QR code were emailed to 143 hospitals through the office of their respective medical director, which was then forwarded to their ophthalmologist who manages RB. An ophthalmologist actively practicing in that hospital was required to answer the survey in collaboration with other specialists involved in the treatment of RB patients. The survey ran from February 2022 to April 2022. Two more reminder e-mails and reminder text messages were sent requesting completion of the survey. Primary outcome measures were human resource capacity, treatment capacity, and education and network capacity. Hospitals were then categorized under an asset-based tier classification.
Asset-based Tier Classification
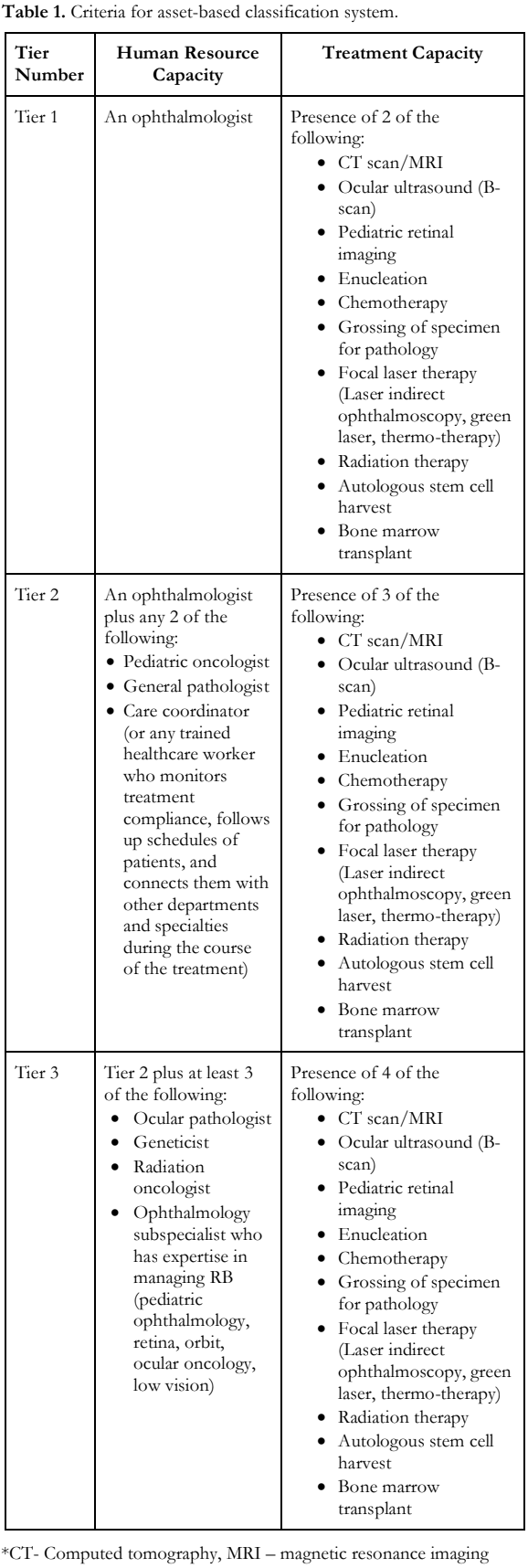
To better qualify treatment capacity, an asset- based tier classification of hospitals was created based on the availability of human resources capacity and treatment capacity (Table 1). Tier 1 refers to hospitals that had the capacity to diagnose RB by an ophthalmologist. Tier 2 are hospitals that can manage advanced cases of RB by enucleation and intravenous chemotherapy administered by a pediatric oncologist. Tier 3 are hospitals capable of ocular salvage and treating the different stages of RB with subspecialized care and rehabilitation thereafter.
Statistical Analyses
Primary outcomes were reported as categorical variables and described in terms of frequencies and percentages. A point map showing approximate locations of hospitals according to tier was developed, alongside a density map showing distribution of Tier 3 hospitals in the country per region.
RESULTS
Seventy (70) hospitals (49%) out of 143 institutions in all 17 regions responded (Table 2). Majority were from the NCR, followed by Central Luzon. Eastern Visayas (Region VIII), Zamboanga Peninsula (Region IX) and Caraga (Region XIII) had zero respondent. The rest of the regions had a response rate of 20 to 100% of the target response. There were 4 Level 1 and 66 Level 3 hospitals that responded. There were no respondents from Level 2 hospitals.
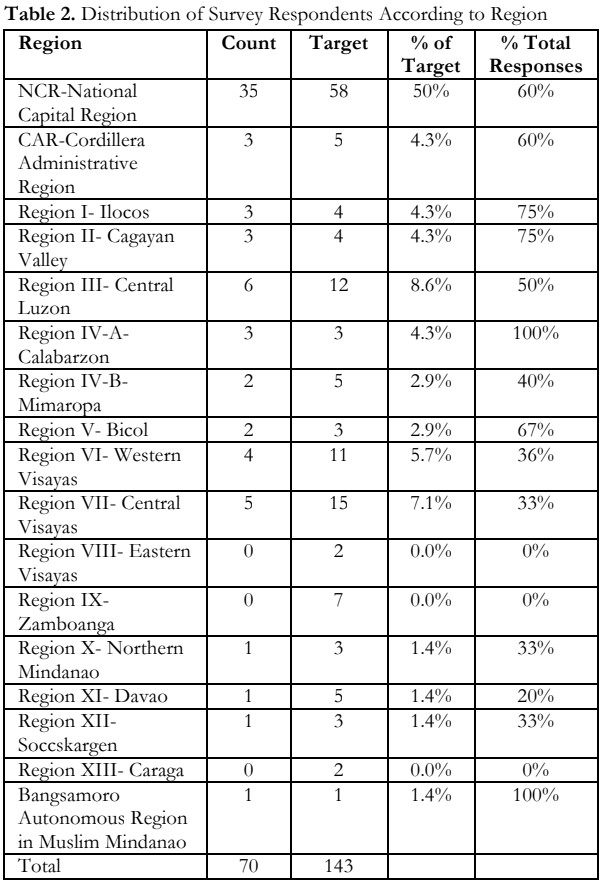
Figure 1 is a point map showing approximate locations of the hospitals color-coded by tier in the Philippines. Figure 2 is a density map which shows distribution of hospitals per region. Both maps show that majority of the hospitals are concentrated in Luzon.
Human Resource Capacity
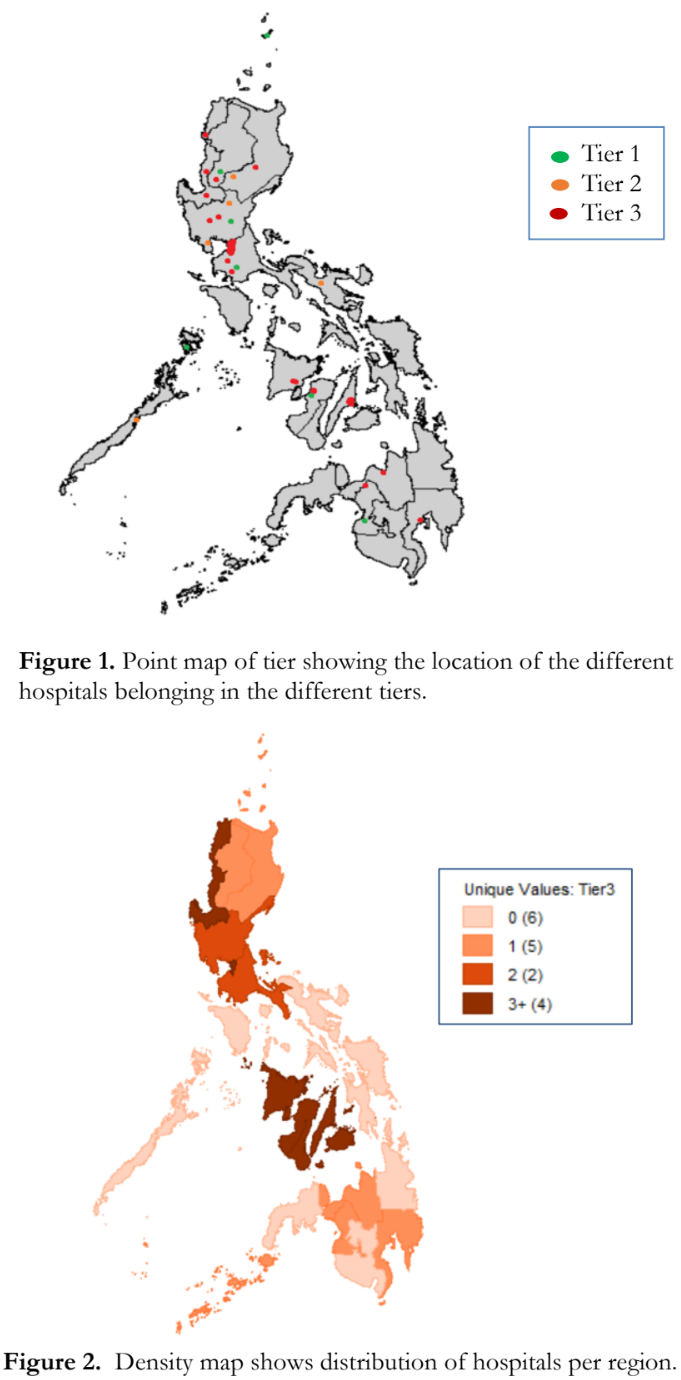
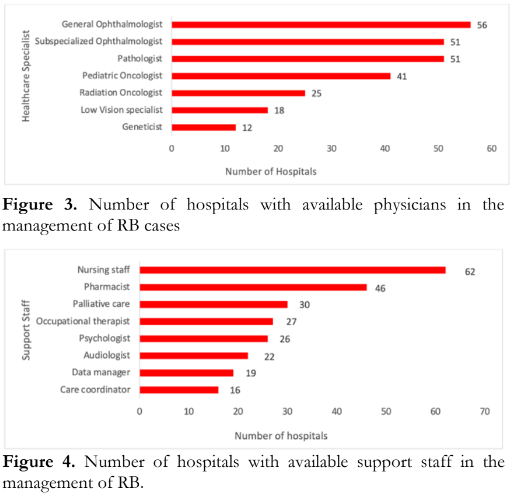
Available key personnel attending to RB patients in most hospitals were a general ophthalmologist (80%), a subspecialized ophthalmologist (71%), a pathologist (71%) and a pediatric oncologist (57%). A few hospitals had a radiation oncologist (35%), a low vision specialist (25%), and a geneticist (17%) [Figure 3]. Most support staff included nursing personnel (96%) and a pharmacist (73%). Palliative care was present in 30 (46%) of the hospitals, followed by occupational therapist, psychologist, audiologist, care coordinator and data manager (Figure 4). The top three healthcare specialists involved in the decision-making in the treatment of RB, are the ophthalmologist, pediatric oncologist and pathologist. Ninety-seven percent (97%) of the ophthalmologists who answered this survey reported being involved in the management of RB in their hospitals.
Treatment Capacity
Diagnosing Retinoblastoma
A CT scan was available in all the respondent hospitals (100%); whereas, lumbar puncture, MRI and ocular ultrasound were available in 89%, 71% and 70% of the hospitals, respectively. The least available technology was the pediatric retinal camera (30%). Occasional use of these modalities was reported by 50-70% of the hospitals. Frequent weekly users are from Philippine General Hospital (NCR), Baguio General Hospital and Medical Center (CAR) and Southern Isabela Medical Center (Region II). The ocular ultrasound or B-scan is the most frequently used diagnostic modality across the weekly, monthly and occasional users. About half of the respondents were very confident in using the CT scan (58%), MRI (55%) and ocular ultrasound (47%) in the diagnosis of RB. Less than a third were very confident with their usage of the pediatric retinal camera (25%) and lumbar puncture (30%). Only 3- 6% of respondents were not confident in using the CT scan, MRI and pediatric retinal imaging in the management of RB.
Treating Retinoblastoma
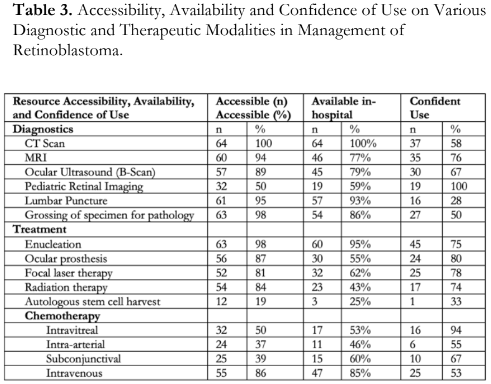
Intravenous chemotherapy (IVC) was the most available route of administration in 73% of respondents. Frequency of use of IVC was weekly in 14% of the respondents, monthly in 18% and occasionally in 38%. Respondents were also very confident (39%) in delivering IVC to RB patients. Enucleation was available in 94% of the respondent hospitals, but only 84% had the capability to tissue diagnosis by histopathology. Ocular prosthesis fitting capability was reported in 47%. In 41%, this service was made accessible off-site in other facilities. Half of the hospitals have focal laser therapy available, while radiation therapy was present in 36% of the hospitals. Quezon City General Hospital, The Medical City, and St. Luke’s Medical Center-Global City, all in the NCR, do autologous stem cell harvest in their hospital. Five percent (5%) of the hospitals perform enucleation on an average weekly basis together with grossing of specimen for pathology, while majority (77%) enucleated occasionally. Fitting of ocular prosthesis, focal laser therapy, radiation therapy and autologous stem cell harvest were reported to be performed occasionally by 70-80% of the respondents. Majority of the hospitals (74%) were very confident in doing enucleation of an eye with RB, but only 54% of the respondents were very confident in grossing of RB for pathologic reporting. About half of the respondents were very confident in fitting an ocular prosthesis (50%), doing focal laser therapy (58%), and giving radiation therapy (47%). A minority were somewhat confident in performing all these treatment modalities (21-33%). Fifty-eight percent (58%) of the respondents had the least confidence in performing autologous stem cell harvest. Summary of accessibility, availability and confidence use of the different diagnostic and therapeutic modalities are shown in Table 3. Accessibility is defined as availability of the hospital to provide the service to the patient whether in- hospital or off-site to another referral facility.
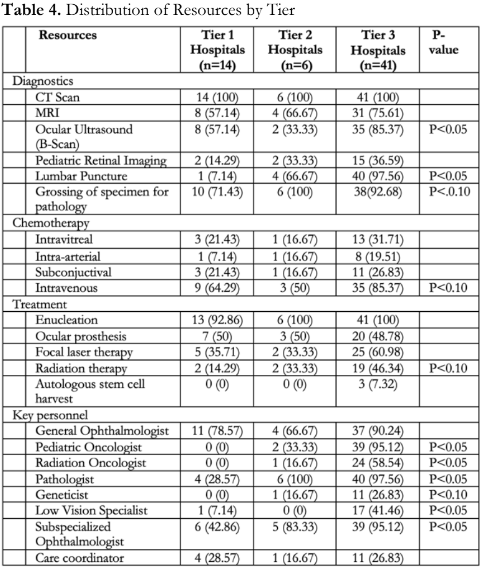
Table 4 shows the distribution of the diagnostic and treatment modalities across the different tiers. Certain resources such as the ocular ultrasound and lumbar puncture were significantly more available in the higher tiers. The availability of a pediatric oncologist, radiation oncologist, pathologist, low vision specialist and subspecialized ophthalmologist across hospital tiers showed a significant difference as well.
The hospital’s social service provided financial assistance for diagnostic procedures, enucleation, chemotherapy, examination under anesthesia (EUA) and palliative care. There were 5 hospitals that reported additional assistance, such as access to temporary housing facilities. National health insurance coverage in the form of the Philippine Health Insurance Corporation (PHIC) was available for enucleation (90%) and chemotherapy (62%). More than half of the hospitals (57%) rely on PHIC for their diagnostic work-up too. Most of the EUA procedures (76%) were financed by the hospital’s social service as it is not covered by PHIC.
Education and Network Capacity
Existing training programs relevant to the management of RB were fellowship programs in retina (43%), radio-oncology (36%), pediatric ophthalmology (33%), pediatric oncology (30%) and orbit and oculoplasty (23%). Ophthalmologists (76%) and pediatricians (60%) were the ones who primarily refer RB patients to hospitals. About half (52%) noted self-referrals from caregivers of RB patients. Others received patients from general practitioners, nurses or allied health professionals. Oncologists (12%) accounted for the least number of referrals.
There were 17 hospitals (26%) that have established a referral network in the population that they serve. Standardized RB treatment protocols were being used by only 15 hospitals (23%). There were 8 hospitals that conduct multi-disciplinary meetings to discuss RB cases. Majority (80%) were not aware of any RB programs in the community to promote awareness and early detection, and 90% were not aware of any program that involves the local government or any other local health administrators.
Only 8 respondents were able to fulfill all three capacities namely East Avenue Medical Center, Fatima University Medical Center, Philippine Children’s Medical Center, Rizal Medical Center, St. Luke’s Medical Center Quezon City and Global City, Southern Philippines Medical Center, and UP- Philippine General Hospital.
Asset-based Tier Classification
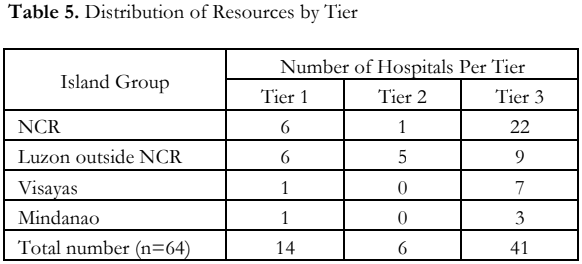
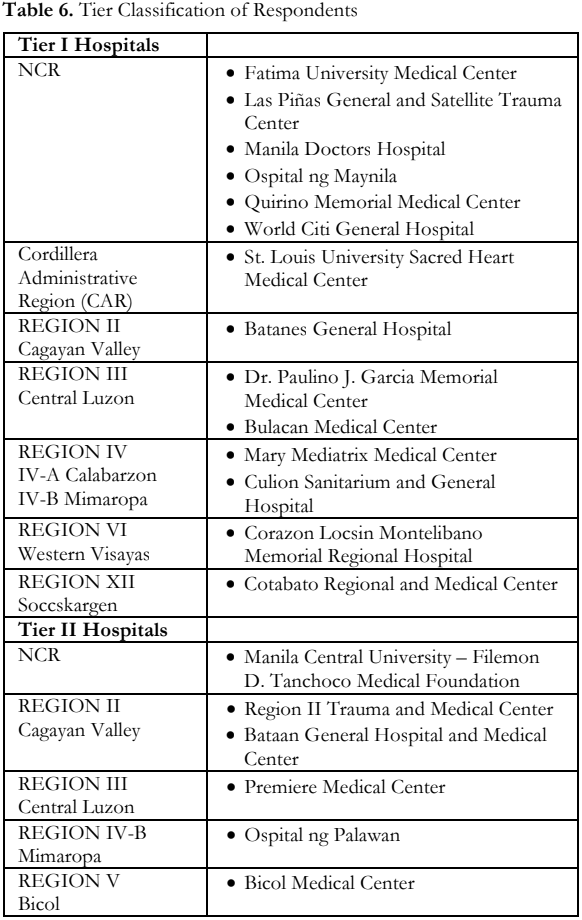
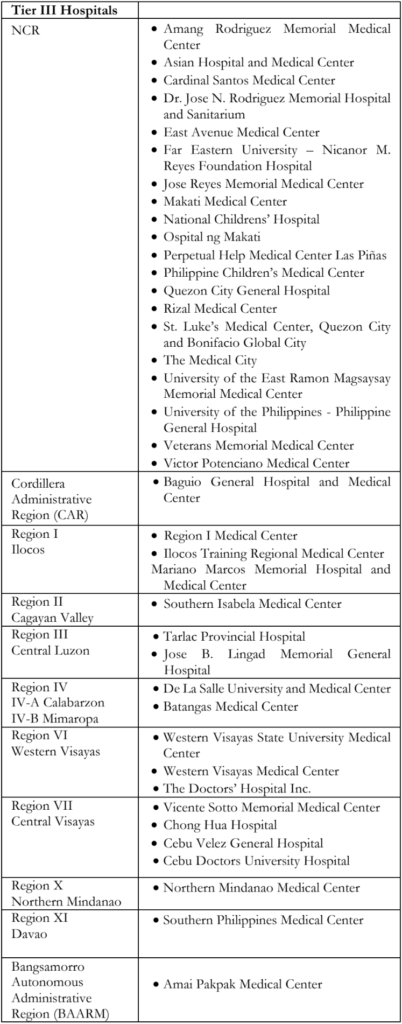
Majority of the respondents (n=61, 95%) were categorized by the asset-based tier classification. There were 14 hospitals categorized to tier 1, which had at least a general ophthalmologist and access to a CT or MRI machine. Six (6) hospitals were classified as tier 2, which had a general ophthalmologist and at least 2 more specialists (pediatric oncologist, general pathologist, or care coordinator). There were 41 hospitals that were classified under tier 3, 22 of which were located in the NCR (Table 5). Table 6 lists downs the participating hospitals according to tier classification and location.
DISCUSSION
This study is the first to report on capacity to treat RB on a national level. There was no response from Regions VIII (Leyte), IX (Basilan, Sulu, Zamboanga del Norte, Zamboanga del Sur), and XIII (Surigao del Norte, Surigao del Sur). Since this survey required an actively practicing ophthalmologist to answer the questionnaire, absence of correspondence from certain provinces may imply either the lack thereof or the method of online correspondence and surveys may not have
suited some physicians who are not adept with answering surveys through an online link or QR code. The first survey of this kind was published by Burges et al. that assessed the capacity to treat RB in the Eastern Mediterranean region.6 However, their survey was distributed to representatives from the Pediatric Oncology East and Mediterranean (POEM) group, naturally obtaining a 100% availability of pediatric oncologists. Our study included all hospitals under the DOH and all tertiary hospitals to avoid sampling bias. DOH hospitals are expected to complement other government-funded and private health facilities in delivering affordable and accessible quality health services. In 2020, the Global Retinoblastoma group published data from 278 RB treatment centers, where Asian countries represented 52% of the participants. They noted a 49% incidence of extraocular tumors at the time of diagnosis of RB patients from low-income countries versus a 2% incidence from high-income countries.9 Pediatric oncologists are more needed in delayed clinical presentations. In our study, 64% of the respondents reported the presence of a pediatric oncologist. The pediatric oncologist was one of the resources more available in the higher-tier hospitals. This maldistribution can affect a LMIC like the Philippines, where RB cases present in advanced stages requiring the care of a pediatric oncologist at the onset. The collaborative management between an ophthalmologist and a pediatric oncologist is critical in increasing the chances of survival of RB patients.
Pediatricians remain to be one of the main referring physicians on this survey. Early referral should be encouraged in this specialty. In Jordan, only 10% of 48 pediatricians were found to perform eye exams routinely.10,11 Pediatricians are the first- contact physicians of these very young patients. Their role cannot be overemphasized for earlier suspicion and prompt referral to any tier-leveled hospital for proper diagnosis by an ophthalmologist. The 80% availability of subspecialized ophthalmologists and pathologists reflects a good number even if they are significantly more available only in tiers 2 and 3 hospitals. Their expertise can guide general ophthalmologists in the proper medical and surgical treatment of RB. A vital support staff that is clearly lacking is a care coordinator, which was reported in only 16 hospitals around the country. A care coordinator can aid in keeping the caregivers and their patients on track with their treatment and directly communicate with them at any time in the management. Care coordination facilitates treatment compliance and surveillance of RB patients.12,14
Most diagnostic and treatment modalities are available in the 64 hospitals that completed the survey. Because RB patients are often managed in referral hospitals, availability of diagnostics and treatment modalities in other institutions does not reflect utilization. There were 41 tier 3 hospitals identified, which signify availability of specialized resources. Yet, there is a low confidence in using the CT scan (56%), lumbar puncture (28%), grossing of the eye for pathology (50%), and delivering intravenous (53%) and intra-arterial chemotherapy (54%). Conversely, although 100% confidence was noted in using a pediatric retinal camera, only 19 hospitals had one. Intravenous chemotherapy, which remains to be the mainstay of treatment in most hospitals (85%), requires experienced pediatric oncologists and treatment-guided protocols to increase the confidence in managing the different stages of RB and dealing with its complications. Skills transfer for grossing of a specimen and proper reporting by a general pathologist are needed for proper tissue diagnosis. Autologous stem cell harvest had the lowest reported confidence at 33% and was only available in 3 hospitals.
LMICs like the Philippines have limited overall funding for RB management. Since PHIC only covers for enucleation (90%), chemotherapy (62%), and select diagnostic tests (57%), other sources of financial assistance obtained by the respondents were from the following: Resources for the Blind Foundation, Malasakit Center, Rotary Club, Lions Club, Tzu Chi Foundation, House of Hope, Cancer Warriors and Mabuhay Deseret Foundation. Inclusion of this childhood cancer in the Z-package of PHIC would decrease the treatment burden on the caregivers.
RB management entails a multidisciplinary team approach. An integrated multidisciplinary workforce can be formed through frequent discussions on their RB cases. Fifteen hospitals are reported to be following a standardized treatment protocol, such as the Metro Manila Retinoblastoma Treatment Protocol. But RB treatment can be sometimes individualized based on the capacity of the attending physicians to provide treatment and the capacity of the patient to comply with the treatment. Tan and Ballesteros in 2020 reported their 15-year treatment outcomes of RB cases in their tertiary hospital in the Cordillera Administrative region (CAR). Improving their chemotherapy protocol was one of the factors which helped improve their survival rate by 12% in the recent years.13 Monitoring treatment outcomes, creating registries, and establishing practice guidelines may increase capacity in the management of RB.
One of Chantada’s recommendations in his Clinical Practice Guidelines – International Society of Pediatric Oncology (SIOP) – Pediatric Oncology in Developing Countries (PODC) study was to establish twinning programs between developing countries like the Philippines with centers in high- income countries.14 Qaddoumi et al. published a study sharing their experience in the First Eye Salvage Program in Jordan, in which they had improved their treatment outcomes for RB through team management, twinning with a center with higher expertise, such as the St. Jude Children’s Research Hospital, and telemedicine. Since then, their RB deaths have declined from 40% to 4% in 10 years.15,16 Successful twinning programs have been recognized between Indonesia and Netherlands, St. Jude Children’s Research Hospital with Central America and Jordan, as well as Canada with Kenya.16 Our survey has identified tier 3 hospitals that can serve as local twinning hospitals with a tier 2 and tier 1 hospital. These include hospitals in NCR, Ilocos, Cordillera Administrative Region (CAR), Cagayan Valley, Central Luzon, Calabarzon, Western Visayas, Central Visayas, Northern Mindanao, Davao and Bangsamorro Autonomous Region in Muslim Mindanao (BAARM). Network clusters can be formed in regions where there are hospitals that have the capacity to treat any stage of RB. Partnership and telemedicine programs already exist in 20% of the respondents. Building up links with a more experienced hospital can support other attending physicians in neighboring regions on their management of RB.17,18 RB patients from more distant regions can, therefore, receive proper care without the need to physically travel far which causes delay in treatment.
Limitation of this study include self-report bias and a low response rate of 49%. Despite these, the data gathered from this survey can be used to promote further improvement in capacity to treat RB. Regions without correspondence need further exploration of resources.
In conclusion, there is a disparity in human resource capacity to treat retinoblastoma across the regions, as most capable centers are located in the NCR. But there is potential to develop centers of excellence among the 41 tier 3 hospitals identified. Diagnostic and treatment modalities are accessible in 82% of the 17 regions. However, stakeholders should undergo continuing education in the management of RB as only 8 respondents were able to fulfill all three capacities.
REFERENCES
1. Steliarova-Foucher E, Colombet M, Ries L, et al. International incidence of childhood cancer, a population- based registry study. Lancet Oncol. 2017;18(6):19-731.
2. Chantada G, Quaddoumi I, Canturk S, et al. Strategies to manage retinoblastoma in developing countries. Pediatr Blood Cancer. 2011;56:340-348.
3. Noguera S, Mercado G, Santiago D. Clinical epidemiology of retinoblastoma at the Philippine General Hospital:1998- 2008. Philipp J Ophthalmol. 2011; 36(1):28-32.
4. Wikipedia. Geography of the Philippines. May 9, 2023: https://en.wikipedia.org/wiki/Geography_of_the_Philip pines#Further_reading (accessed August 8, 2023).
5. Napulan R, De Roxas D, Tonato R, Reyes A. DOH Hospitals Profile. October 2020. https://www.doh.gov.ph (accessed June 15, 2021).
6. Burges M, Qaddoumi, Brennan R, et al. Assessment of Retinobalstoma Capacity in the Middle East, North Africa and West Asia Region. JCO Global Oncol. 2020;6:1531-1539.
7. List of Accredited Health Facilities; Level 3 hospitals – Updated September 2021. https://www.philhealth.gov.ph (accessed October 10, 2021).
8. Lavado RE, Ulep VG, Pantig M, et al. Profile of Private Hospitals in the Philippines. Discussion Paper Series No. 2011-05. Philippines Institute for Development Studies. March 2011. Microsoft Word – Private hospital 20110309 (pids.gov.ph) (accessed August 8, 2021).
9. Fabian D, Abdallah E, Abdulahi SU, et al. Global Retinoblastoma Presentation and Analysis by National Income Level. JAMA Oncol. 2020;1;6(5):685-695.
10. Ababneh LT, Khriesat W, Dalu S, et al. Knowledge of and attitude to eye disorders among pediatricians in North Jordan. Ann Med Surg (Lond). 2021;67:102430.
11. Youseff YA, Alnawaiseh T, Aljabari R, et al. Retinoblastoma awareness among first contact physicians in Jordan. Ophthalmic Genet. 2019;40(3):191-195.
12. Okado I, Pagano I, Cassel K et al. Clinical Research Professional Providing Care Coordination Support:A Study of Hawaii Minority/Underserved NCORP Community Site Trial Participants. JCO Oncology Practice. 2022;18(7):e1114-e1121.
13. Tan RJD and Ballesteros KFB. Retinoblastoma Outcomes in a Tertiary Hospital in Northern Luzon in the Philippines: A 15-Year Experience. South Asian J Cancer. 2022; 11(2):160-163.
14. Chantada G, Luna-Fineman S, Sitorus RS, et al. SIOP- PODC Recommendations for Graduated-Intensity Treatment of Retinoblastoma in Developing Countries. Pediatr Blood Cancer. 2013; 60:719-727.
15. Arora, RS, Challinor JM, Howard S, Israelis T. Improving Care for Children with Cancer in Low-and Middle-Income Countries- A SIOP PODC Initiative. Pediatr Blood Cancer. 2016; 63:387-391.
16. Canturk S, Qaddoumi I, Khetan V, et al. Survival of retinoblastoma in less developed countries impact of socioeconomic and health-related indicators. Br J Ophthalmol. 2010; 94(11):1432-6.
17. Quaddoumi I, Nawaiseh I, Mehyar M, et al. Team management. Twinning and Telemedicine in Retinoblastoma: A 3-Tier approach implemented in the First Eye Salvage Program in Jordan. Pediatr Blood Cancer. 2008 Feb; 51(2):241-244.
18. Youseff Y.MD, Al-Nawaiseh I, Mehyar M, et al. How Telemedicine and Centralized Care Changed the Natural History of Retinoblastoma in a Developing Country. Ophthalmology. 2021;128(1):130-137.

