Bilateral Frontalis Sling for Surgical Correction of Unilateral and Bilateral Severe Congenital Ptosis with Poor Levator Function
Reynaldo M. Javate, MD, FICS
University of Santo Tomas Hospital Eye Institute and Department of Ophthalmology, University of Santo Tomas Hospital, Manila
Correspondence: Reynaldo M. Javate, MD, FICS
Clinic Address: Rm. 501, Doctors’ Clinics, 5th Floor, Clinical Division, University of Santo Tomas Hospital, España Blvd, Sampaloc Manila, Philippines 1008
Clinic Phone Number: +632-296-3636/ +632-731-3001 local 2516
E-mail: rmjavatemd@gmail.com
Disclosure: The authors reports no financial relationship or conflict of interest.
The correction of congenital ptosis in young children is one of the most difficult cosmetic surgeries to perform. Many authors have reported difficulty not only with adequately correcting ptosis, but also with functional and cosmetic results. There are currently several surgical options and materials used for the treatment of congenital ptosis: silicone rods, mesh, polytetrafluoroethylene (PTFE) and grafts such as fascia lata.1 Selection depends on several factors including the experience and comfort level of the surgeon and the degree of ptosis and levator muscle function in the patient.2
Sling surgery with autogenous fascia lata, the gold standard procedure for congenital ptosis, has a long-lasting effect on upper eyelid elevation. However, the main disadvantage of this procedure is the need for a second surgical site to harvest the fascia with possible risks of infection, hematoma and scar formation at the donor site and cicatricial contracture of the upper eyelid.3 Expanded PTFE (ePTFE) is a viable alternative to traditional sling materials for ptosis repair. Ease of use, durability, and safety are a few advantages of this technique. Compared with other materials, ePTFE is easier to place, requires less surgical time, and provides excellent lid contour and function with minimal bulk in the eyelid.4 On the other hand, silicon sling is known for its versatility and for its lesser tendency to induce scar tissue around the sling.5 The ease of adjusting the silicone rod slings makes it an excellent suspensory material in cases of blepharoptosis that more frequently require postoperative adjustment. It is also the new material of choice for patients with ptosis from neurologic causes.6,7
To our knowledge, no study has been published on the technique of Callahan using ePTFE or silicone rod in bilateral frontalis suspension in patients with unilateral or bilateral severe congenital ptosis. This procedure termed the “Chicken Beard” was described by Alston Callahan where the frontalis suspension is performed bilaterally but the levator muscle on the less ptotic eyelid remains intact.8 Recognition that true unilateral congenital ptosis is a rare condition and that more commonly there is some alteration of function in the other eyelid that appears to be more “normal” is also a useful concept in managing congenital ptosis. Sometimes, better symmetry may be achieved by performing bilateral surgery, combining frontalis suspension on the more ptotic lid and conjunctival Mueller’s muscle resection ptosis repair on the lid that appears to be less ptotic. This could be nicknamed the “Chicken Katowitz”.9 In this study, we evaluated the functional and cosmetic results of patients who underwent bilateral frontalis sling repair for severe congenital ptosis with poor levator function (“Chicken Beard Callahan Technique”)8 using the ePTFE and silicone rod.
METHODS
This was a retrospective, noncomparative, interventional case series involving patients with unilateral or bilateral severe congenital ptosis and poor levator function who underwent frontalis sling using an expanded PTFE (Ptose-up ®, FCI, 20-22 rue Louis Armand, 75015 Paris, France) or silicone rod (Ptosis sling, FCI, 20-22 rue Louis Armand, 75015 Paris, France) at the University of Santo Tomas Hospital (USTH) from February 2012 to November 2018. A single surgeon (RMJ) performed all the operations after informed consent for the surgery was obtained from the patients’ parents or legal guardians. This study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of the USTH.
Only medical records of patients with simple congenital ptosis unassociated with any other anomaly were included in the study. The diagnosis of congenital ptosis was made when the drooping of the upper lid was noted at birth or during the first year of life. Severe ptosis is diagnosed when the margin to reflex distance or MRD1 is 0 millimeter (mm) or the upper eyelid completely droops >4 mm. Poor levator function is defined as levator muscle movement of 2 mm or less and no more than 6 mm by various authors.10,11,12 In this study, for any degree of ptosis with levator function of 4mm or less, frontalis or brow suspension procedure was performed.13 Patients with blepharophimosis, Marcus-Gunn jaw- winking ptosis, or history of ocular or orbital surgery were excluded from the study. Patients who had less than 6 months follow-up after surgery were also excluded.
Bilateral frontalis sling repair was performed on all patients regardless of unilateral or bilateral involvement following the Chicken Beard Callahan procedure. In patients with severe unilateral ptosis and levator function of < 4mm, bilateral frontalis suspension is recommended. The parents, however, made the final decision. If the parents were opposed to perform surgery on the normal eyelid, unilateral suspension was done but they were excluded from the study.
The following pre-operative data were collected: measurement of MRD1 in primary gaze with the frontalis muscle at rest, amount of levator function, presence of Bell’s phenomenon, and lagophthalmos. In addition, the following data postoperatively were recorded: MRD1 in the primary position, contour, frontalis material used, lid height after procedure and presence of complications such as lagophthalmos and corneal exposure. Preoperative and postoperative photographs in primary gaze and downgaze were reviewed and compared for contour.
The primary study outcomes were the rating of eyelid height postoperatively based on the criteria by Tarbet et al. (“Frontalis suspension for severe unilateral congenital ptosis with poor levator function,” presented at the American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS) Annual Meeting, New Orleans, Louisiana, 1998) and eyelid contour. Eyelid height was judged to be excellent if MRD1 measured > 2 mm or if the difference in MRD1 between the two eyelids (asymmetry) was < 1 mm. It was rated good if MRD1 was 1-2 mm or if asymmetry was 1.5-2 mm, and poor if MRD1 measured < 1 mm or if asymmetry was > 2 mm.14 Eyelid height was assessed in primary gaze with the frontalis muscle relaxed wherein MRD1 was measured in primary gaze without any request for additional eye opening which is termed Habitual MRD.15 Eyelid contour was rated satisfactory if there was no peaking, lagophthalmos and asymmetry and unsatisfactory if it was peaked, asymmetric, or there was lagophthalmos.
Complications of infection, exposure of sling material, granulomas, undercorrections, overcorrections, exposure keratopathy, or poor cosmesis were observed at every visit.
RESULTS
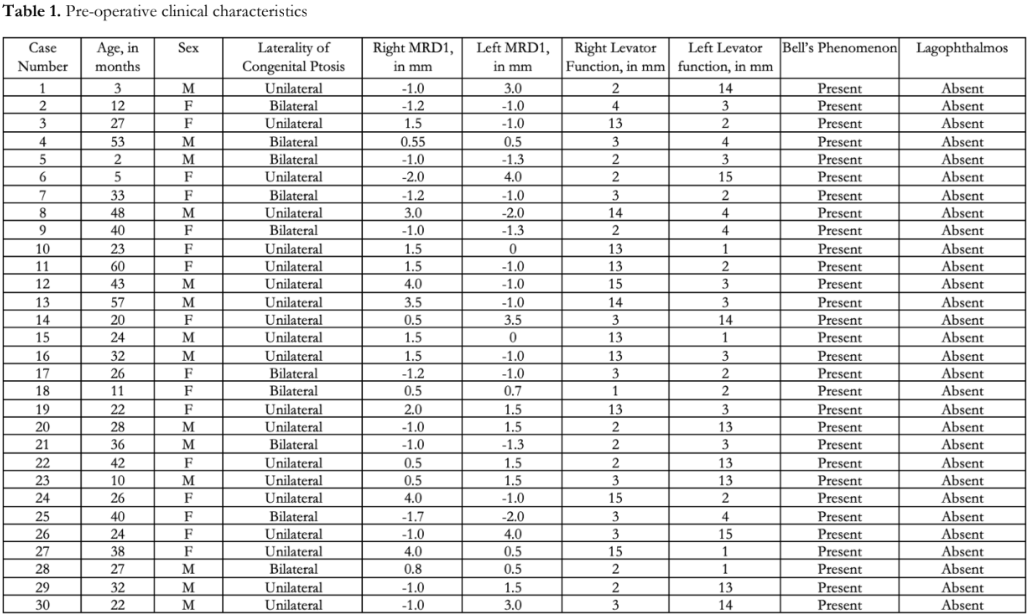
Thirty (30) patients with congenital ptosis who underwent bilateral frontalis suspension were included in the study. The mean age was 28.9 ± 15.2 months (range: 2 – 60 months). There were 18 (60%) males. Majority (n=20, 67%) had unilateral ptosis while 10 patients (33%) had bilateral ptosis. Table 1 shows the pre-operative clinical characteristics of each patient. MRD1 ranged from 0.5-2.0 mm while levator function ranged from 2-4 mm. Bell’s phenomenon was observed in all eyes and none had lagophthalmos.
Half of the patients (n=15 or 50%) underwent ePTFE surgery while the other half (n=15 or 50%) had the silicone rod. The patients were followed up for a mean period of 15.6+6.9 months with a range of 9 to 36 months. Table 2 shows the post-operative cosmetic outcomes. Postoperative MRD1 values ranged from 2-4 mm. All had satisfactory eyelid contours (100%). Excellent eyelid height was achieved in 16 patients (53%). Good eyelid height was achieved in 14 patients (47%).
Figure 1 shows representative pre- and postoperative photos of a child with bilateral congenital ptosis who underwent ePTFE surgery. Figure 2 are representative photos of a child with unilateral congenital ptosis who underwent bilateral silicone rod surgery. In both cases, excellent eyelid height and satisfactory lid contours were achieved.



Majority of patients (90%) did not develop any complications with the use of these materials except for 1 case of silicone rod exposure secondary to trauma to the brow area which occurred 1 month post-surgery and 2 patients with silicone rod who had ptosis recurrence. There were no reports of infection or granuloma formation.
DISCUSSION
The goals of surgical correction of congenital ptosis include clearing the visual axis, correcting the unsightly droopy appearance, and creating symmetry between the two eyelids. Ideally, all of these should be accomplished without compromising the protective function of the eyelid. However, attaining all these surgical goals in every case is not always possible and the surgical technique usually includes some compromise.
Frontalis suspension, a popular surgical procedure to correct congenital ptosis, is aimed at achieving the cosmetically required eyelid height when the eyebrow is raised, a habit usually acquired a few months following surgery. The procedure requires the eyelid to be attached with a sling material to the frontalis muscle. Sling materials can be autogenous fascia lata or synthetic materials such as non-absorbable synthetic suture, monofilament, nonabsorbable polypropylene suture mesh, ePTFE, polybutylate-coated braided polyester, and silicone. Some studies have shown that synthetic materials achieved less favorable outcomes when compared to fascia lata. Synthetic materials have a higher tendency for complications, such as granuloma formation, exposure, and recurrence of ptosis. However, they remain popular because the synthetic materials are readily available and do not require or are not limited by graft harvesting. ePTFE also has shown great potential for long-term biocompatibility. It is reportedly nonantigenic and both biologically and chemically inert. Steinkogler et al. reported only one case of recurrent ptosis requiring surgical repair and one rejection requiring surgical excision with ePTFE.16 They stated that the use of ePTFE would obviate the need for fascia lata in frontalis suspension surgery. There was also no recurrence of ptosis in up to 18 months of follow-up.17 Compared with other materials, ePTFE is easier to place, requires less surgical time, and provides excellent lid contour and function with minimal bulk in the eyelid.4 It is a biocompatible, porous, solid, and smooth material leading to less potential for infection, granuloma, and extrusion.18 It also has the lowest incidence of ptosis recurrence.19
On the other hand, silicone rod has elastic properties which preserve eyelid closure function and result in lower degree of lagophthalmos. Therefore, it is commonly used in young children or patients who have a high risk of corneal exposure and those with inadequate Bell’s phenomenon. Kim et al. described its use as safe, simple, easy, and effective. However, recurrence was the most challenging problem.20
Currently, there is an argument with regard to the surgical options for unilateral ptosis with abnormal levator muscle function. The ideal treatment of unilateral blepharoptosis with poor or asynchronous levator muscle function has yet to be established. Although oculoplastic surgeons agree on the need for frontalis suspension of the affected eyelid, management of the contralateral eyelid remains controversial. Technically, the problem with the unilateral sling is that the good eye can be opened without frontalis muscle use; thus, there is little incentive for the patient to use the frontalis to elevate the ptotic eyelid. Beard reported asymmetry between the suspended and contralateral eyelids, advocating excision of the normal levator muscle to create bilateral ptosis.13 Surgical correction with bilateral frontalis slings was performed resulting in good upper eyelid symmetry in all positions of gaze, although there was equal lagophthalmos in downgaze. The biggest problem with this approach is that most parents of patients are reluctant to destroy a normal levator for the sake of cosmesis. Callahan suggested bilateral slings, but with preservation of the contralateral levator muscle. This produces symmetrical lag in downgaze but allows the functioning levator muscle on the nonptotic side to elevate the eyelid in primary position.8 Seiff recognized that more surgeons prefer to leave the normal levator alone.21 Symmetry is achieved in the primary position and downgaze as movements of both normal and abnormal eyelids are restricted by the sling in these positions. However, there is still asymmetry in upgaze.22
To better address the ongoing argument and to determine the effectiveness of Callahan’s procedure among patients with unilateral congenital ptosis, it is recommended in the future to compare the postoperative results of patients with unilateral congenital ptosis who underwent unilateral frontalis sling to those who underwent bilateral frontalis sling in a large number of patients with long term follow-up.
Our study findings show that good to excellent lid height and satisfactory eyelid contour can be achieved by either use of silicone rod or ePTFE in the correction of congenital ptosis. Silicone sling is a safe and effective method of correcting congenital ptosis with poor levator function.14 The main advantages of the biomaterial are that they involve no harvesting of autogenous tissues and its related morbidity and that they are packaged and ready to use, all of which are considerable time savings. The elimination of morbidity related to harvesting of autogenous materials is a great advantage in everyday surgery. Thus, not only do the materials have to be non-carcinogenic, non-allergenic, non-immunogenic and infection-resistant to some extent, but it is also preferable that they integrate with the organism (i.e.. be colonized and be replaced by the cells of the organism).23 As mentioned, ePTFE provides excellent lid contour and function and also has the lowest incidence of ptosis recurrence. There were 2 cases of ptosis recurrence in the silicone rod group. Ptosis recurrence is due to the cheese wiring effect or cutting of suture materials through the tissue.24
Most importantly, with the “Chicken Beard Callahan Technique” performed on 30 patients, better symmetry is achieved on primary position, and downgaze, as movements of both normal and abnormal eyelids are restricted by the sling in these positions without destruction of the normal levator; thus, it is theoretically more acceptable to parents of patients.8
In conclusion, bilateral frontalis suspension in patients with severe congenital ptosis, whether bilateral or unilateral, results in good to excellent functional and cosmetic outcomes using expanded polytetrafluoroethylene and silicone rod.
REFERENCES
- Sternberg I, Seelenfreund MH, Stenberg N. A new sling material for ptosis patients. Ophthalmic Surg. 1988;19(1):64- 6.
- Takahashi Y, Leibovitch I, Kakizaki H. Frontalis suspension surgery in upper eyelid blepharoptosis. Open Ophthalmology J. 2010;4:91-97.
- Balkan RJ, Ellis G, Eustis S. At the Crossings: Pediatric Ophthalmology and strabismus: childhood ptosis: an oculoplastic perspective. Netherlands: Kugler Publication, 2004; 267-282.
- Meszaros L. New material for ptosis repair offersease of placement, good results. November 1, 2003: https://www.ophthalmologytimes.com/view/new- material-ptosis-repair-offersease-placement-good-results (accessed August 1, 2023).
- Bernardini FP, de Conciliis C, Devoto MH. Frontalis suspension sling using a silicon rod in patients affected by myogenic blepharoptosis. Orbit .2002;21:195-8.
- Van Sorng AJ, Devoglaere T, Sotodeh M, et al. Exposure kerapopathy following silicon frontalis suspension in adult neuro- and myogenic ptosis. Acta Ophthalmol. 2010; 8:1-5.
- Carter SR, Meecham WJ, Seiff SR. Silicon frontalis slings for the correction of blepharoptosis: indication and efficacy. Ophthalmology. 1996;103:623-30.
- Callahan A. Correction of unilateral blepharoptosis with bilateral eyelid suspension. Am J Ophthalmol. 1972;74:321- 6.
- Foster JA, Kherani JA. Aesthetic Considerations in Pediatric Oculoplastic Surgery. In Katowitz JA, Katowitz KR, eds. Pediatric Oculoplastic Surgery. New York: Springer New York, 2017;279-290.
- Lee JH, Kim YD. Surgical treatment of unilateral severe simple congenital ptosis. Taiwan J Ophthalmol. 2018;8(1):3-8
- SooHoo JR, Davies BW, Allard FD, Durairaj VD. Congenital ptosis. Surv Ophthalmol 2014;59(5):483-492.
- Kasaee A, Aliabadi M, Najafi L, Jamshidian-Tehrani M. Severe unilateral congenital ptosis with poor levator function: tarsoconjunctival mullerectomy plus levator resection vs frontalis sling procedure. Int J Ophthalmol. 2022;15(8):1254-1260.
- Beard C. A new treatment for severe unilateral congenital ptosis and for ptosis with jaw-winking. Am J Ophthalmol. 1965;59:252-8.
- Choudhary U, Sharma S. Frontalis sling surgery using silicon rod: Results in congenital unilateral ptosis among north indian population. International Journal of Medical and Biomedical Studies. 2019;3(12):226-228.
- Khwarg SI, Tarbet KJ, Dortzbach RK, Lucarelli MJ. Management of moderatre to severe Marcus Gunn jaw winking ptosis. Ophthalmology. 1999;106:1191-6.
- Steinkogler FJ, Kuchar A, Huber EA, Rocker- Mettinger E. Gore-Tex soft tissue patch frontalis suspension technique in congenital ptosis and in blepharophimosis-ptosis syndrome. Plast Reconstr Surg. 1993;921057-1060.
- Wasserman BN, Sprunger DT, Helveston EM. Comparison of materials used in frontalis suspension. Arch Ophthalmol. 2001;119:687-691.
- Wei YH, Liao SL. Frontalis suspension using expanded polytetrafluoroethylene: results of different surgical designs. J Formos Med Assoc. 2009;108(12):943–949.
- Kokubo K, Katori N, Hayashi K, et. al. Frontalis suspension with an expanded polytetrafluoroethylene sheet for congenital ptosis repair. J Plas Reconstr Aesthet Surg. 2016;69(5):673–678.
- Kim CY, Son BJ, Son J, Hong, J, et al. Analysis of the causes of recurrence after frontalis suspension using silicone rods for congenital ptosis. PloS One. 2017;12(2): e0171769.
- Seiff S. Commentary on Unilateral Frontalis Sling for the Surgical Correction of Unilateral Poor-function Ptosis. Ophthal Plast Reconstr Surg 2005;21(6):416-7.
- Buttanri IB, Serin D, Karslioglu S, Akbaba M, et al. Effect of suturing the silicone rod to the tarsal plate and the suture material used on success of frontalis suspension surgery. Ophthal Plast Reconstr Surg. 2013;2(2):98–100.
- Ruban JM, Burillon C, Tabone E, et. al. A new material in ptosis surgery with brow suspension: wide porous expanded polytetrafluoroethylene: Analysis of our first 75 cases. Orbit. 1996;15(2):67-76.
- Al Abdullah BA, Hatif MB. Evaluation of Mehta’s modification of the Crawford technique for Frontalis Sling Surgery with Silicon rod in Severe Ptosis. Iraqi Natl J Med. 2020;2(2):85-94

