A Study Protocol on the Situational Analysis on the Current Practice of Screening and Treatment of Retinopathy of Prematurity (ROP)
Karina Q. De Sagun-Bella, MD, Theresa Gladiola B. Merca, MD, Jane Melissa L. Lim, MD, Alvina Pauline D. Santiago, MD, Pearl Tamesis-Villalon, MD, Andreas Mueller, PhD, MPH, Leo D.P. Cubillan, MD, MPH
INTRODUCTION
According to the World Health Organization (WHO), childhood blindness refers to a group of conditions occurring in childhood, which could result in blindness or severe visual impairment, and are likely to be untreatable later in life. Severe visual loss in childhood can affect productivity, education, and employment opportunities, thereby reducing the quality of life for visually impaired children.
The major causes of blindness in children vary according to socio-economic development. Various diseases such as measles, vitamin A deficiency, ophthalmianeonatorum and malaria, high risk factors such as malnutrition, and lack of health care facilities with appropriate personnel and equipment for treating eye diseases plague the system for treating eye diseases in developing countries. Despite these, even in these countries, ROP is emerging as an important cause of childhood blindness.
Retinopathy of Prematurity (ROP), previously known as retrolental fibroplasia, is an ischemic retinopathy affecting premature and low birth weight infants, which may cause some degree of visual loss, ranging from mild to severe. There is altered development of the retinal vascularization leading to abnormal new vessels that may lead to dire consequences like vitreous hemorrhage and retinal detachment. ROP can also lead to complications such as refractive errors, amblyopia, strabismus, glaucoma, blindness and phthisis. Some of the risk factors for the disease are degree of prematurity, low birth weight, poor weight gain, sepsis and exposure to fluctuating supplemental oxygen.
Historically, two epidemics of retinopathy of prematurity have been described in industrialized countries. The first epidemic occurred in the 1940’s to 1950’s which affected babies in the USA and Western Europe. The principal risk factor for this epidemic was the unmonitored indiscriminate use of supplemental oxygen, affecting babies with mean birth weight of 1370g in both the United Kingdom (UK) and the United States (US). The second epidemic was seen in industrialized countries in the 1970’s due to the higher survival rates in extremely premature babies. A “third epidemic” has been described in developing countries as survival rates of premature and low birth weight infants are improving. If appropriate screening and treatment guidelines are implemented, however, ROP as a cause of blindness can be a potentially avoided. Prompt and timely intervention is necessary to optimize the long-term outcome of the child’s vision.
In this study protocol, the current situation in a selected area as regards ROP management will be evaluated by providing an overview of policies followed by vitreo-retina specialists and pediatric ophthalmologists in Metro Manila. Likewise, an estimate of the proportion of childhood blindness or visual impairment that is caused by ROP will be obtained by information gathered from local schools for the blind. In addition, Neonatal Intensive Care Units (NICUs) in a selected area will be surveyed to provide an estimate of the number of premature babies at risk for ROP.
METHODOLOGY
The study protocol is a descriptive, cross sectional study using survey questionnaire. The primary objectives of the study are to provide an overview of the current practice of screening and treatment of ROP in a selected area, to estimate the proportion of childhood blindness due to ROP in the area and assess the number of premature babies at risk for ROP. All qualitative data will be reported by frequency distribution and percentages and extrapolation will be done.
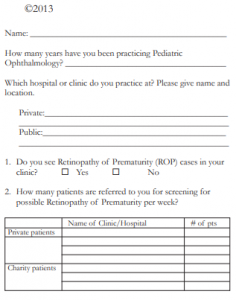
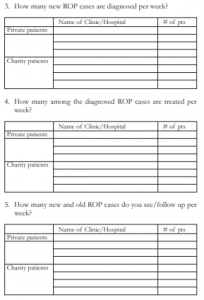
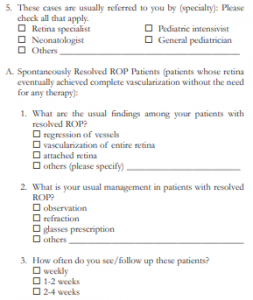
Pediatric Ophthalmologists and Vitreo-Retina specialists
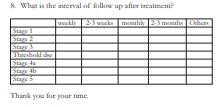
A list of the practicing pediatric ophthalmologists and vitreo-retina specialists practicing in the selected area will be retrieved from the local ophthalmological society. Questionnaires will be sent out to all pediatric ophthalmologists and vitreo-retina specialists in the area. The prepared forms include questions on the estimated number of ROP cases seen, diagnosed and treated by consultants, screening and treatment criteria used, the kind of treatment modality used for ROP cases in need of treatment and referral to other subspecialist after treatment. Information about the timing of screening and techniques of examination will also be gathered. Respondents will be contacted via phone or email regarding additional information or clarifications. (Appendices 1 and 2)
Estimate the proportion of ROP
A database search of local blind school/s in the area will be done to estimate the proportion of childhood blindness or visual impairment identified as due to ROP. Student records and clinical abstracts, when available, will be reviewed from the different schools for the blind in the area. Clinical diagnoses were tallied and the percentage of ROP will be taken. For diagnosed ROP cases, data on the age of gestation, birth weight, course in the NICU and previous treatment will be noted.
Neonatal Intensive Care Units
Hospitals with NICU facilities in the area are listed. A survey on the Neonatal Intensive Care Units (NICU) will done using questionnaire forms to be sent to the Division Heads of these hospitals. The forms include questions on the estimated number of premature babies admitted to the NICU by birth weight and gestational age, survival rates of premature infants, presence of necessary equipment and personnel in the NICU, ROP screening policies in their institution and criteria used for referral of infants with high risk for ROP. For additional information and clarifications, respondents will be contacted by the researchers through telephone or email. (Appendix 3)
International studies on ROP screening and treatment in other countries and international societies will be reviewed for comparison with the ROP guidelines set by the local subspecialty societies. Local national programs regarding ROP, if present, will also be reviewed.
All qualitative data will be presented in frequency distribution and percentages and will be presented in tabular form.
DISCUSSION
ROP is considered as an important and emerging cause of childhood blindness. This study aimed to show the current practices of specialists in ROP screening and treatment, the estimated proportion of childhood blindness caused by ROP and the number of premature babies at risk. This proposal aims to establish the proportion of ROP in a selected area and the show the magnitude of the disease in the area though extrapolation. By assessing the NICU prematurity incidence and survival rates, the number of babies at risk for the development of ROP can be determined. The study protocol aims to show the importance of timely screening and treatment of ROP cases to prevent complications of ROP such as visual impairment and blindness. An advantage of using the survey questionnaire in this study design is the practical way of colleting large information from a large number of specialists in a short period of time and in a cost effective way. However, survey questionnaires are limiteddue tolow response rates, responses based on recollection or estimates and are based on their interpretation of the question. The responses will be limited to the amount of information being asked without further explanation.
CONCLUSION
Results from study designs like this can provide the framework for recommendations for programs aimed providing criteria for timely screening and treatment of ROP to prevent complications such as childhood visual impairment and blindness in the country.
APPENDIX I TOOL FOR ASSESSMENT OF RETINOPATHY OF PREMATURITY (ROP) SCREENING AND TREATMENT PROGRAMS
FOREWORD
Retinopathy of prematurity (ROP) is an ocular disorder involving abnormal vascular proliferation in the retina of premature infants which can progress to visual impairment or blindness. Severe visual loss in childhood can affect productivity, education and employment opportunities, thereby reducing the quality of life for visually impaired children. According to WHO, childhood blindness refers to a group of conditions occurring in childhood, which could result in blindness or severe visual impairment that are likely to be untreatable later in life. The major causes of blindness in children vary according to socioeconomic development and accessibility of primary health care. In middle-income countries, retinopathy of prematurity is emerging as an important cause of childhood blindness. The aims of this tool are:
- To provide an estimate of the prevalence of childhood blindness or visual impairment that is caused by Retinopathy of Prematurity (ROP)
- To provide an overview of existing national ROP guidelines, policies and recommendations and their utilization
- To assess the current capacity of NICUs with ROP screening programs and treatment facilities
The purpose of the study is to evaluate the current situation of the country in regards to ROP management. Information collected will be intended for planning a national ROP screening and treatment programs.
APPENDIX II TOOL FOR ASSESSMENT OF RETINOPATHY OF PREMATURITY (ROP) SCREENING AND TREATMENT PROGRAMS
FOREWORD
Retinopathy of prematurity (ROP) is an ocular disorder involving abnormal vascular proliferation in the retina of premature infants which can progress to visual impairment or blindness. Severe visual loss in childhood can affect productivity, education and employment opportunities, thereby reducing the quality of life for visually impaired children. According to WHO, childhood blindness refers to a group of conditions occurring in childhood, which could result in blindness or severe visual impairment that are likely to be untreatable later in life. The major causes of blindness in children vary according to socioeconomic development and accessibility of primary health care. In middle-income countries, retinopathy of prematurity is emerging as an important cause of childhood blindness.The aims of this tool are:
- To provide an estimate of the prevalence of childhood blindness or visual impairment that is caused by Retinopathy of Prematurity (ROP)
- To provide an overview of existing national ROP guidelines, policies and recommendations and their utilization
- To assess the current capacity of NICUs with ROP screening programs and treatment facilities
The purpose of the study is to evaluate the current situation of the country in regards to ROP management. Information collected will be intended for planning a national ROP screening and treatment programs.



APPENDIX III
TOOL FOR ASSESSMENT OF RETINOPATHY OF PREMATURITY (ROP) SCREENING AND TREATMENT PROGRAMS
FOREWORD
Retinopathy of prematurity (ROP) is an ocular disorder involving abnormal vascular proliferation in the retina of premature infants which can progress to visual impairment or blindness. Severe visual loss in childhood can affect productivity, education and employment opportunities, thereby reducing the quality of life for visually impaired children. According to WHO, childhood blindness refers to a group of conditions occurring in childhood, which could result in blindness or severe visual impairment that are likely to be untreatable later in life. The major causes of blindness in children vary according to socioeconomic development and accessibility of primary health care. In middle-income countries, retinopathy of prematurity is emerging as an important cause of childhood blindness.The aims of this tool are:
- To provide an estimate of the prevalence of childhood blindness or visual impairment that is caused by Retinopathy of Prematurity (ROP)
- To provide an overview of existing national ROP guidelines, policies and recommendations and their utilization
- To assess the current capacity of NICUs with ROP screening programs and treatment facilities
The purpose of the study is to evaluate the current situation of the country in regards to ROP management. Information collected will be intended for planning a national ROP screening and treatment programs.
Name: ____________________________________________
How many years have you been practicing as a Neonatologist?
__________________________________________________
Hospital Name: _____________________________________
Private
Public
1. Estimate Number of Total Admissions in the NICU per
month? _________________________________________
2. Estimate number of premature babies admitted to the NICU
per month by:
Birth weight category: # %
i. ≤ 1500 grams _______ _________
ii. ≤ 2500 grams _______ _________
Gestational Age: # %
i. ≤ 30 weeks ________ _________
ii. ≤ 37 weeks ________ _________
3. Estimate number of surviving premature babies admitted in
the NICU per month by:
Birth weight category: # %
i. ≤ 1500 grams _______ _________
ii. ≤ 2500 grams _______ _________
Gestational Age: # %
i. ≤ 30 weeks ________ _________
ii. ≤ 37 weeks ________ _________
4. Estimate number premature babies admitted in the NICU
per month by:
i. those with prolonged oxygen therapy _____ (# and %)
ii. those with stormy course in the NICU (intubated, sepsis,
pneumonia, blood transfusion etc) _________ (# and %)
iii. those with poor weight gain _____________ (# and %)
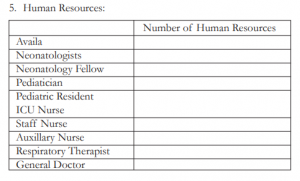
i. Please provide an estimate number of human resources
available in the NICU:
ii. How many preterm babies are supervised by each nurse?
_____________________________________________
6. Infrastructure and Equipments:
i. Are these equiptments available in your NICU?
Cots Yes No
Vital Signs Monitors Yes No
Ventilators Yes No
Oxygen blenders Yes No
Humidifier Yes No
Flowmeter Yes No
7. Does the NICU in your institution have an established referral
system for ROP patients to the ophthalmologists?
Yes No
8. To whom do you refer Retinopathy of Prematurity patients:
(please check all that apply)
General Ophthalmologists
Vitreo-Retina specialists
Pediatric Ophthalmologists
Fellows of the Ophthalmology Department
Others ______________________________________
9. What criteria do you use for referral of ROP patients?
Age:
≤ 28 weeks AOG
≤ 30 weeks AOG
≤ 32 weeks AOG
Others (please specify) ________________________
OR
Birth weight
≤ 1250 grams
≤1500 grams
≤1800 grams
Others (please specify) ________________________
OR
Other criteria
older babies / larger babies with prolonged oxygen
therapy
stormy course in the NICU (intubation, sepsis,
pneumonia, blood transfusion etc)
poor weight gain
parents request
10.Does your hospital have the facilities for treatment of these
ROP patients? Yes No
Thank you for your time.