A Case Report of Scleral Buckle Implant Mimicking An Orbital Tumor
Lee Jerome F. Briones MD, Mark Anthony T. Imperial MD
Department of Ophthalmology, University of the East Ramon Magsaysay
Memorial Medical Center Inc., Metro Manila, Philippines
Corresponding Author: Lee Jerome F. Briones MD
Clinic Address: University of the East Ramon Magsaysay Medical Arts Building, 64 Aurora Boulevard, Quezon City, 1113, Philippines
Clinic Phone Number: +639178271894
Email Address: jerome.briones@gmail.com
Disclosure: The authors declare no conflicts of interest.
In the 1950s, Charles Schepens and colleagues developed the technique of scleral buckling to repair rhegmatogenous retinal detachment.1 The principle was to significantly relieve vitreous traction on the detached retina by indenting the sclera using silicone rubber to mechanically support the areas under traction.2 Complications related to silicone buckle include scleral necrosis, infection, migration, and extrusion.
In the mid-1980s, a new material made of hydrophilic polymer cross-linked with ethylene diacrylate was introduced to address the problems associated with silicone buckles.3 They were soft, pliable and could store and release antibiotics reducing the incidences of scleral erosions and buckle infections.1 However, enthusiasm over its use waned due to numerous reports of orbital discomfort and diplopia associated with swelling and fragmentation of the hydrogel implants. Eventually, its use was discontinued in 1995.4
We report a patient with a history of scleral buckling surgery for retinal detachment in 1990 who presented in the clinic complaining of blurring of vision and an incidental finding of restricted extraocular movement of the right eye.
CASE REPORT
A 75-year-old male complaining of gradual, painless blurring of vision of the right eye of four months duration consulted at our institution. The patient underwent retinal detachment repair of the right eye using a scleral buckle in 1990. The patient has medically controlled hypertension. He denied any family history of lacrimal gland neoplasms as well as previous history of stroke.
Best-corrected visual acuity was hand movement in the right eye and 20/100 in the left eye. On inspection, there was downward displacement of the right globe and marked restriction of ocular motility on all directions (Figure 1). On modified Krimsky test, a 30 prism diopter exotropia of the right eye was noted. There was no proptosis on Hertel’s exophthalmometry. Pupils were briskly reactive to light with no relative afferent pupillary defect. On slit lamp examination, both corneas were clear with deep anterior chambers. Visually-significant cataracts were noted in both eyes. On indirect ophthalmoscopy, the posterior pole was not visible on the right eye due to the cataract, while the left fundus was unremarkable.

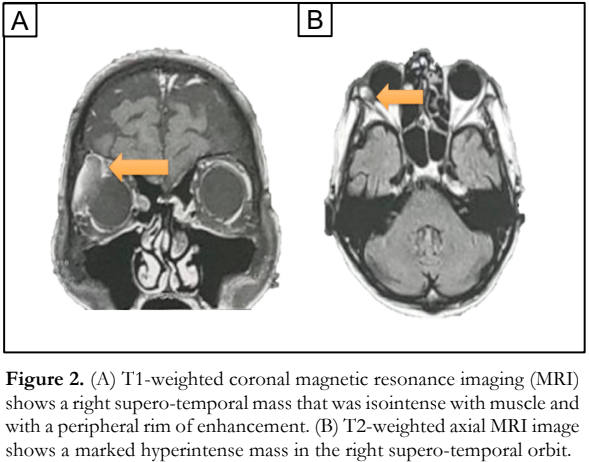
Based on the inferior displacement of the globe, a supero-temporal mass was considered. The patient had previous orbital imaging taken with a 1.5 Tesla magnetic resonance imaging (MRI) machine which showed a circumferential supero-temporal mass measuring 4.8 x 3.5 x 2.0 centimeters (cm) that was isointense on the T1-weighted images and hyperintense on the T2 weighted images (Figure 2). Although cavernous hemangioma is a common orbital tumor in the patient’s age group, his MRI findings was not consistent with this orbital tumor.
Lateral orbitotomy was performed which revealed an encapsulated mass adherent to the globe at the right supero-temporal region. Upon further dissection, a friable, gel-like, and translucent material was seen (Figure 3). Careful excision of the material was done ensuring its complete removal. Residual scleral buckle sutures were isolated and removed.
Intraoperatively, scleral thinning with calcifications underlying the buckle without vitreous leak were also noted. The patient’s wound was then sutured and packed with sterile gauze. He was started on antibiotic eye ointment and cold compress thrice a day. Histopathologic analysis of the specimen revealed an acellular, amorphous, granular, and eosinophilic material with no evidence of malignancy. He was discharged the following day without any complications.

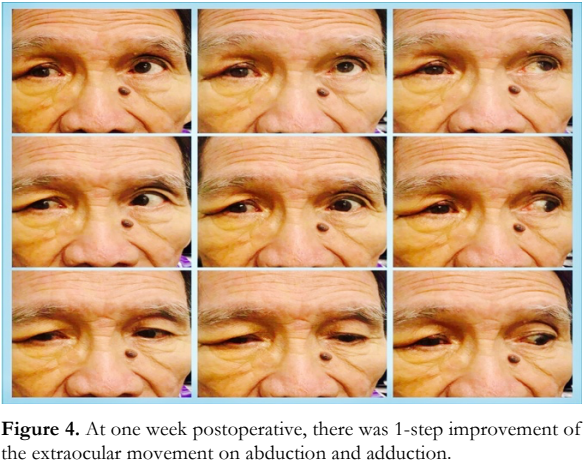
At 1-week follow-up, there was a slight improvement in extraocular muscle movement and resolution of the hypoglobus (Figure 4). Best- corrected visual acuity remained unchanged for both eyes.
DISCUSSION
This is the first case in the local literature of an elderly male who presented with a supero-temporal orbital mass due to a possible overexpanded hydrogel scleral buckle. We also report the longest interval from implantation to excision of a possible hydrogel scleral buckle. Previous reports of post-operative complications of expanded hydrogel implants include buckle extrusion, diplopia, orbital swelling, and orbital cellulitis.5 They may present with ocular pain or discomfort, ocular motility disturbance, scleral or conjunctival erosion, cosmetic problems, ptosis, corneal astigmatism, and tear film insufficiency.1
Hydrogel implants are composed of a low- molecular-weight hydrophilic material that was designed to store antibiotic agents reducing the incidence of scleral buckling infections.6 The buckle swells a little after implantation, increasing buckling effect which was deemed to be a desirable outcome. However, these implants had the tendency to absorb water over the years and enlarge dramatically in size. The mean time from implantation to presentation of symptoms was noted at 8.3 years with a range of 6 months to 14 years.7 The long-term complications of this implant ranged from non-tender subconjunctival mass to ocular erosion, extrusion, and migration of the buckle.2
Excision of a possible overexpanded hydrogel scleral buckle in this patient eventually led to improvement of his symptoms. Whereas the intraoperative record from his retinal surgery was not available, there was no evidence that this patient was implanted with a hydrogel buckle. But given the dramatic swelling of the implant, the timeline of his scleral buckling surgery, MRI findings, and the friable nature of the material intraoperatively, it was more likely than not. Our patient underwent scleral buckling surgery in 1990, when hydrogel implants were the predominant implant of choice. In addition, the MRI findings of the patient were consistent and comparable with other cases that had late complications related to hydrogel scleral buckling surgery. They typically appear as a circumferential mass surrounding the globe that is isointense with the extraocular muscles on T1-weighted images and hyperintense on T2-weighted images due to intrinsic swelling of the buckle with water. An enhanced capsule is also demonstrated surrounding the mass; such findings are similar to that of our patient.8 Furthermore, our intraoperative finding of a friable, gel-like, and translucent material is consistent with the suspected etiology.7
In contrast to hydrogel implants, silicone implants have fewer side effects leading to their continuous use today. Due also to advances in technique such as the replacement of diathermy with cryotherapy and the presoaking of buckle elements in antibiotic solution, complications of necrosis and infection have lessened.9
Hydrogel scleral buckle complications can be readily identified through a combination of clinical history, radiography, and gross examination alone. However, on certain occasions when clinical history is uncertain and material cannot be identified on gross inspection, a histopathologic examination is needed to confirm a diagnosis or to rule out alternative pathologies. For a more definitive diagnosis, we propose that the excised implant in this case be subjected to histopathologic studies with special stains such as Alcian blue and periodic acid-Schiff in order to distinguish them from other periorbital foreign materials and neoplasm.10
In conclusion, hydrogel scleral buckle expansion may mimic an orbital tumor. Excision of these implants through lateral orbitotomy not only relieves the signs and symptoms, but also confirms the etiology.
REFERENCES
- Crama N, Klevering BJ. The removal of hydrogel explants: an analysis of 467 consecutive cases. Ophthalmology. 2016; 123(1): 32-38.
- Lane JI, Randall JG, Campeau NG, et al. Imaging of hydrogel episcleral buckle fragmentation as a late complication after retinal reattachment surgery. AJNR Am J Neuroradiol. 2001; 22(6): 1199-1202.
- Das T, Namperumalsamy P. Scleral buckling with hydrogel implant. Indian J Ophthalmol. 1991; 39(2): 41-43.
- Thompson JT, Chambers WA. Good ideas gone bad: The MIRAgel saga. Ophthalmology. 2016; 123: 5–6.
- Bernardino CR, Fay AM, Rubin PA. A clinicopathological series of the spectrum of long-term complications from hydrogel scleral buckles – orbital cellulitis mimicry, prosthesis intolerance, and orbital pseudotumor. Invest Ophthalmol Vis Sci 2003; 44(13): 2234.
- Leibovitch I, Crompton J, Selva D. New onset diplopia: 14 years after retinal detachment surgery with a hydrogel scleral buckle. Br J Ophthalmol. 2005; 89(5): 640.
- Kearney JJ, Lahey J, Borirakchanyavat S, et al. Complications of hydrogel explants used in scleral buckling surgery. Am J Ophthalmol. 2004; 137(1): 96-100.
- Ashikaga R, Im S, Yagyu Y, et al. MR Imaging of Hydrogel Scleral Buckle as a Late Complication after Retinal Detachment Surgery. Acta Med Kinki Univ. 2013; 38(2): 111-113.
- Fallico M, Alosi P, Reibaldi M, et al. Scleral Buckling: A Review of Clinical Aspects and Current Concepts. J Clin Med. 2022; 11(2): 314
- Wolkow N, Jakobiec F. Histopathology of Hydrolyzed MIRAgel Scleral Buckles. Ocul Oncol Pathol. 2021; 7(4): 272- 279.

