A 10-Year Retrospective Study on the Presentation, Treatment, and Outcomes of Retinoblastoma Patients in a Philippine Tertiary Hospital
Maria Socorro M. Torno MD, Miriam Joy F. Tan MD, Allyson Rose C. Facundo MD,
Emilio L. Macias III MD, Catherine B. Valconcha-Adraneda MD
Department of Ophthalmology, Jose R. Reyes Memorial Medical Center, Manila
Correspondence: Maria Socorro M. Torno, MD
Clinic Address: Department of Ophthalmology, Jose R. Reyes Memorial Medical Center, San Lazaro Compound, Rizal Avenue, Sta. Cruz, 1012 Manila, Philippines
Clinic Telephone Number: (8)711-9491 local 266
Email Address: mariastorno@gmail.com
Disclaimer: The investigators of this study have no financial relationships or any conflicts of interest to report.
When presented with a child with leukocoria, strabismus, or proptosis, it is imperative to rule out retinoblastoma (RB), a masquerading syndrome that is the most common primary ocular cancer in children. It is diagnosed at a mean age of 2 years old, with an estimated 5,000 to 8,000 new cases worldwide each year.1 About 60% of the cases present unilaterally with no gender predilection. Bilateral involvement is suspected to be associated with a germline mutation in the tumor-suppressing retinoblastoma susceptibility gene RB1 and is heritable with a higher risk for secondary tumors such as pineoblastoma, a condition known as trilateral retinoblastoma. In contrast, unilateral cases are often sporadic and non-heritable.2
Due to rapid advancements in treatment and multispecialty collaboration, RB has one of the highest cure rates among childhood cancers, with a 5-year survival rate of 96%.2 However, this is not the case in developing countries where the mortality rate remains high.3 In the Philippines, the lack of healthcare facilities significantly contributes to the delay in providing treatment for RB patients, with 80% of total healthcare delivery time being spent on gaining access to tertiary care.4 Other factors include financial burden and misdiagnosis.5 This lag between the onset of symptoms and initiation of therapy correlates to the progression of the tumor beyond the globe, portending a more dismal prognosis.4-8
This study aimed to report the epidemiology, clinical characteristics, and survival outcomes of patients diagnosed with RB at a single institution. Results from this study may contribute to the limited available local studies, with the goal of establishing a standardized registry and treatment protocol for RB patients in the Philippines.
METHODS
This was a retrospective review of medical records of all patients diagnosed with RB between January 2011 to December 2020 at Jose R. Reyes Memorial Medical Center (JRRMMC). The list of patients diagnosed with RB was collected from the hospital patient census. Medical charts from the Ophthalmology and Pediatrics departments were reviewed and the following data were collected: the place of residence, age at diagnosis, sex, initial clinical presentation, laterality, and clinical diagnosis based on the International Classification of Retinoblastoma (ICRB). Eyes with unclear diagnosis or those that had the Reese-Ellsworth classification were reclassified to ICRB. The type of treatment received whether laser indirect ophthalmoscopy, chemotherapy, radiotherapy, enucleation, or exenteration was also noted. The last known status of the patient whether alive, expired, or lost to follow-up by study endpoint on November 30, 2021 was recorded. Attempts were made to contact and trace the patients with missing data and those who were lost to follow-up.
Statistical Analysis
Descriptive statistics were used to summarize the clinical characteristics of the participants. This included median and range to describe age, and frequency and proportion for all other variables. All valid data were included in the analysis. Missing data were noted as a separate variable. STATA 15.0 was used for data analysis.
RESULTS
A total of 31 patients (37 eyes) with RB were included in the study. This corresponds to an average of 3 new cases per year. The median age at diagnosis was 2 years (range 2 months to 8 years). Males comprised slightly over half (55%). Most came from outside of Metro Manila (52%), with 2 cases coming from the Visayas. The majority (81%) had unilateral disease, with left and right eyes affected almost equally. Four (13%) were diagnosed with bilateral RB and 2 (6%) with trilateral RB. The most common initial clinical presentation was leukocoria (19%), followed by periorbital swelling (10%) and eye redness (6%) (Table 1).
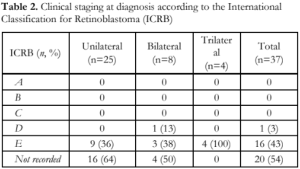
Affected eyes were classified according to ICRB. Based on the ICRB classification, there were 16 eyes (43%) in group E, and 1 eye (3%) in group D. Twenty eyes (54%) had insufficient data for proper classification (Table 2).
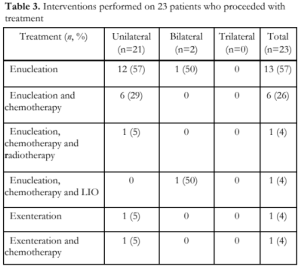
A total of 23 (74%) out of 31 patients diagnosed with RB underwent treatment in our institution. Enucleation was the most frequent intervention and was performed on 21 patients (91%). Enucleation was combined with chemotherapy in 6 patients (26%), with chemotherapy and radiotherapy in 1 patient (4%), and with chemotherapy and LIO in 1 patient (4%). Exenteration was performed in 1 patient (4%) and exenteration combined with chemotherapy in another patient (4%) (Table 3). Eight patients (25%) did not continue with treatment.

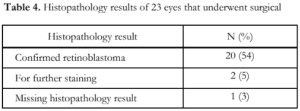
Among the 37 eyes clinically diagnosed with RB, 21 eyes (57%) were enucleated, while 2 eyes (5%) were exenterated. Of these 23 eyeballs submitted for histo-pathological evaluation, 20 eyeballs (87%) showed histo-pathological confirmation of RB. The diagnosis of 2 eyeballs (9%) remained unconfirmed and required additional staining. The data for 1 eyeball (4%) could not be retrieved. This allowed a clinico-pathological correlation of 54% (20/37) of all eyes diagnosed with RB (Table 4).
Information on survival outcome, whether alive or expired, was known for 12 patients only (39%). Four (33%) were alive while there were 8 (67%) recorded mortalities. Of these 8 deaths, 3 patients did not undergo any form of treatment, 2 underwent enucleation alone, while 3 had both enucleation and chemotherapy. Intracranial metastasis was the most common cause of death. Four patients who were alive had either completed or were receiving ongoing treatment. There was no information on the survival outcome of 19 patients (61%) (Table 5).

DISCUSSION
The Philippines is listed as one of six countries anticipated to account for 40% of the estimated global burden of RB in 2023.9 Given the predicted increase in RB cases, there is a pressing need to gather comprehensive and accurate data on the disease in our region.10 This study reported an average number of 3 new cases per year, which is consistent with a study done in Baguio General Hospital and Medical Center, a government tertiary center in Northern Luzon.11 The comparatively low number of cases at our facility may be due to the fact that Philippine General Hospital, recognized as the national referral center for RB, is located in the same city. The latter has reported an average of 15 cases per year, a rate similar to Southern Philippines Medical Center, a government treatment and referral center for RB in Mindanao.4-6
The median age of presentation in this study was 2 years old, mostly composed of unilateral cases (81%), consistent with local and international data.4,5,7,11-15 In contrast, studies conducted in Taiwan, Thailand, Singapore, and Western countries reported that patients mostly presented at an earlier age before 2 years old.12,15-16 A large portion of the patients in this study was diagnosed in the advanced stage, falling under ICRB Group E (43%), while none belonged to Group A-C. This pattern of late diagnosis is consistent with the findings of other local studies and the situation in the countries previously mentioned, where earlier stages are rarely seen, except in bilateral cases.5,11,13 The variability in the age of presentation and corresponding stage of disease across nations underscores the significance of early medical care, as it can affect the prognosis and outcome of RB.15,17,18 This study did not include factors that delayed consultation, which is an important detail that should be obtained during history taking.
As in other studies, leukocoria (19%) was the most common presenting ocular sign that prompted medical consult.5,7,11,12,14,19 Extraorbital signs such as periorbital swelling and proptosis were also observed, which is a late manifestation more commonly seen in patients in developing countries.4,5,11,14,15 The lack of parental awareness of the disease is a crucial factor, as symptoms such as eye redness and swelling can be easily downplayed as conjunctivitis. Therefore, primary care physicians have an essential role in conducting a thorough examination to detect early signs of RB. To further increase the knowledge and understanding of this disease, our department has been actively organizing RB awareness webinars for both medical practitioners and the general public, distributing informative pamphlets at the outpatient department and other high-traffic areas within the hospital, and participating in health education advocacies of the Philippine Academy of Ophthalmology. National efforts to improve awareness are also in place, with the Department of Health placing a spotlight on 8 childhood cancers which include RB, and incorporating Cancer in Children Awareness Month in the Philippine Cancer Control Program.6,9 It is important to improve Filipinos’ health-seeking behavior by addressing misconceptions and emphasizing that RB is curable, especially when detected and treated early in its course. 7,8
The majority of patients in our study required drastic measures such as enucleation (91%) or exenteration (8%). Among the 31 patients, 8 (26%) refused to receive any treatment or failed to follow up. Poor compliance with treatment was also observed in the study by Tan et al., where 81% underwent enucleation or exenteration, while 25% declined surgery.11 An investigation on the potential psychosocial factors that negatively influenced parental decision-making regarding enucleation revealed reasons such as the belief that cancer is a fatal disease, apprehension with unsatisfactory cosmetic results following surgery, and the cost of treatment.8 While we do not have data on the timing of dropouts in our setting, it is evident that parents of the patients experience difficulties shortly after receiving the diagnosis, such as feeling overwhelmed or discouraged.8 In addition, there has been a deviation from requesting computed tomography scans for RB to minimize the risk of secondary malignancies.20 Magnetic resonance imaging (MRI) under sedation is preferred; however, it has been a challenge in our institution to schedule pediatric patients for MRI because of the long waiting time. A pediatric anesthesia-compatible machine for the MRI is also not readily available. Consequently, some patients are advised to have imaging done outside our institution which involves additional expenses and inconvenience.
We recorded 8 cases of mortality secondary to intracranial metastasis. Similarly, metastasis was the primary cause of death in an earlier local study on outcomes of RB patients with high-risk histopathologic features.21 The second published local study on RB outcomes reported an overall survival rate of 53%, with a poorer prognosis when extraocular involvement was present.11 Unfortunately, determining the survival rate and identifying contributing factors in our study was a challenge due to a considerable number of patients with unknown survival status and missing post- enucleation histopathology results.
A limitation of this study is its retrospective nature. Inadequate standardized data collection, documentation, and poor record keeping may have resulted in the skewing of values towards lower estimates. We recommend the formation of a centralized digital database in our institution that would address these issues and allow for better- quality research in the future.
In summary, our study has shown preliminary data on poor outcomes in RB management prior to the formation of a multidisciplinary retinoblastoma team, the establishment of a registry, and the introduction of advanced treatments such as intra-arterial chemotherapy. To improve the management of RB in our locality and across the Philippines, collaboration among various institutions and specialties is key to creating a national treatment program. By pooling resources and expertise, conducting joint research initiatives, and providing training and education for healthcare providers, we can ensure that every child with RB receives the best possible care and has the greatest chance for a successful outcome.
ACKNOWLEDGMENTS
The authors would like to acknowledge 101 Health Research for the statistical analysis and consultation, and Dr. Evelyn S. Morabe for her invaluable assistance and guidance in the preparation of this paper.
REFERENCES
- Abramson DH. Retinoblastoma in the 20th Century: Past Success and Future Challenges The Weisenfeld Lecture. Invest. Ophthalmol. Vis. Sci. 2005; 46(8): 2684-2691.
- American Cancer Society. Cancer Facts & Figures 2020. Atlanta: American Cancer Society 2020; 12-13.
- Shields CL, Shields, JA. Diagnosis and Management of Retinoblastoma. Cancer Control. 2004; 11(5), 317–327.
- Malabanan-Cabebe CG, Gonzales-Sy JJ. Health Care Timeline for Patients with Retinoblastoma Seen in Southern Philippines Medical Center: Brief Report. SPMC J Health Care Serv. 2021; 7(2): 7.
- Noguera SI, Mercado GJ, Santiago DE. Clinical Epidemiology of Retinoblastoma at the Philippine General Hospital 1998-2008. Philipp J Ophthalmol. 2011; 36(1): 28- 32.
- Perandos-Astudillo CM, Roño RC. Health Care Timeline for Patients with Retinoblastoma Seen in Southern Philippines Medical Center: Policy Notes. SPMC J Health Care Serv. 2021; 7(2): 8.
- Rahmat J, Sunder R, Alagaratnam J, Goh P. Retinoblastoma Registry report-Hospital Kuala Lumpur experience. Medical J Malaysia. 2010; 65 Suppl A:128-130.
- Domingo RE, Toledo MS, Mante BV. Psychosocial Factors Influencing Parental Decision to Allow or Refuse Potentially Lifesaving Enucleation in Children with Retinoblastoma. Asia Pac J Oncol Nurs. 2017; 4: 191-6.
- Usmanov RH, Kivelä T. Predicted Trends in the Incidence of Retinoblastoma in the Asia-Pacific Region. Asia Pac J Ophthalmol. 2014; 3: 151-157.
- Mercado GJ, Tan RJ. Addressing the Need for Complete and Updated Data on Retinoblastoma in the Philippines. Philipp J Ophthalmol 2022.
- Tan RJD, Ballesteros KFB. Retinoblastoma Outcomes in a Tertiary Hospital in Northern Luzon, The Philippines: A 15-Year Experience. South Asian J Cancer. 2022; 11(2); 160- 163.
- Jain M, Rojanaporn D, Chawla B, et al. Retinoblastoma in Asia. Eye 2019. 33: 87-96
- Singh U, Katoch D, Kaur S, et al. Retinoblastoma: A Sixteen-Year Review of the Presentation, Treatment, and Outcome from a Tertiary Care Institute in Northern India. Ocul Oncol Pathol. 2018; 4: 23-32.
- Subramaniam S, Rahmat J, Rahman NA, et al. Presentation of Retinoblastoma Patients in Malaysia. Asian Pac J Cancer Prev. 2014; 15(18), 7863-7967.
- Global Retinoblastoma Study Group. Global Retinoblastoma Presentation and Analysis by National Income Level. JAMA Oncol. 2020; 6(5) 685-695.
- Li S-Y, Chen SC-C, Tsai C-F, et al. Incidence and Survival of Retinoblastoma in Taiwan: A Nationwide Population- based Study 1998-2011. Br J Ophthlamol. 2016; 100: 839- 842.
- Tomar AS, Finger PT, Gallie B, et al. Global Retinoblastoma Treatment Outcomes: Association with National Income Level. American Joint Committee on Cancer Ophthalmic Oncology Task Force. Ophthalmology. 2021; 128(5): 740–753.
- Chawla B, Hasan F, Azad R, et al. Clinical Presentation and Survival of Retinoblastoma in Indian children. Br J Ophthlamol. 2015; 100: 172-8.
- Duangnate R, Taweevat A, Wimwipa D, et al. Clinical Presentations and Outcomes of Retinoblastoma Patients in Relation to the Advent of New Multimodal Treatments: A 12-Year Report from Single Tertiary Referral Institute in Thailand. J Ophthalmology. 2020; 4231841.
- Almater A, Alfaleh A, Alshomar K, AlMesfer S. Retinoblastoma: Update on Current Management. September 19, 2019: http://dx.doi.org/10.5772/intechopen.88624 (accessed April 16, 2023).
- Cabrera PE, Mercado GJ, Domingo RE, et al. Outcome of Retinoblastoma Patients with High-risk Histopathological Features in a Tertiary Hospital. Philipp J Ophthalmol 2013; 38: 43-49.

