Pars Plana Vitrectomy with Silicone Oil Tamponade as Primary Treatment of Myopic Foveoschisis with High Risk for Macular Hole
Patrick A. Santiago MD, Julia Mercedes C. Villalva MD
Department of Ophthalmology, Far Eastern University-Nicanor Reyes Medical Foundation Medical Center, Quezon City
Correspondence: Julia Mercedes C. Villalva MD
Clinic Address: FEU Eye Center Inc., 2nd Floor, FEU-NRMF, Quezon City, Metro Manila
Clinic Phone Number: +632-89838338 loc 1200
Email Address: juliavillalva@gmail.com
Disclosure: The authors report no conflict of interest. No financial support was received for the study.
Pathologic myopia, defined as the development of pathologic changes associated with myopia, is becoming increasingly prevalent across the globe and is one of the leading causes of vision loss and blindness.1 Pathologic features include myopic traction maculopathy (MTM) or myopic foveoschisis, where there is schisis-like thickening of the retina.2 This affects 9-34% of pathologic myopic eyes with or without staphyloma. The pathogenesis is believed to be multifactorial but involves anterior traction, the intrinsic rigidity of the internal limiting membrane (ILM), and progression of the posterior staphyloma.3 Diagnosis of MTM is confirmed with optical coherence tomography (OCT) scan of the macula.
To date, there is no consensus on the management of MTM. The natural course of MTM varies depending on the severity of the macular retinoschisis: some remain stable, while others progress to more serious complications. Several surgical techniques have been proposed including macular buckle, pars plana vitrectomy (PPV) with ILM peeling, PPV without ILM peeling, and PPV with retinal detachment and release of temporal retina.4 However, there are limited studies on visual and anatomic outcomes. This small case series aimed to describe a safe, effective, and novel surgical technique for the treatment of MTM.
METHODS
This is a small case series involving 3 eyes with MTM seen within the period of November 2018 to October 2021. All eyes had MTM confirmed by spectral-domain OCT. All eyes underwent PPV using the Constellation® Vision System (Alcon, Fort Worth, Texas, USA) with maximum cut rate of 5,000 cuts per minute (cpm) and injection of silicone oil 1,500 cSt (Aurosil, Aurolab, India) without ILM peeling by a single vitreoretinal surgeon. Repeat eye examination with OCT of the macula were performed during the post-operative period.
RESULTS
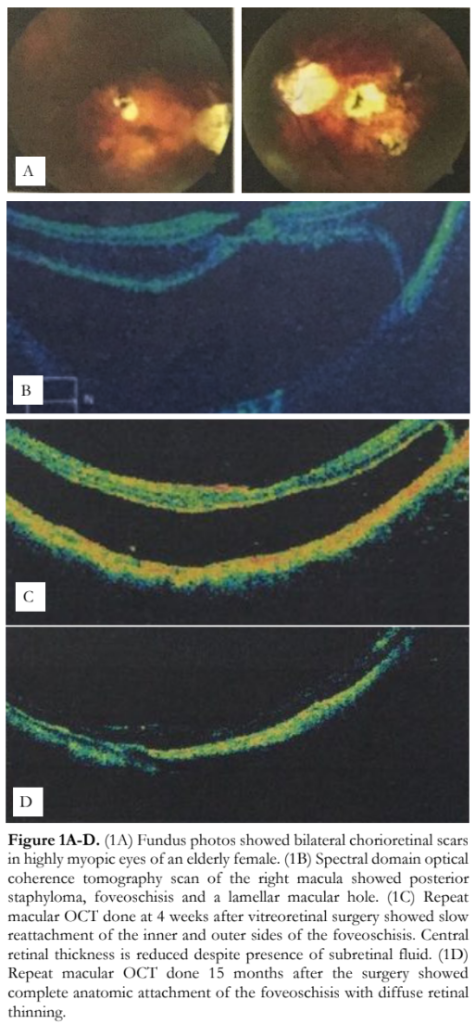
A total of 3 eyes diagnosed with MTM was included in the study. Case 1 is an 81-year-old woman who developed bilateral, sequential MTM. Her first consult was in 2018 for poor vision in the right eye. Best-corrected visual acuities (BCVA) were 20/400 OD and 20/200 OS. Axial lengths were 33mm OD and 30mm OS. Fundus findings revealed myopic degeneration with chorioretinal atrophic scars (Figure 1A). On OCT, the right eye had a central retinal detachment, retinoschisis, with a lamellar macular hole. The central foveal thickness was 321 microns with 6 of 9 subfields showing p>99% thicker than age-matched cohorts (Figure 1B). The left eye had cystic changes in the central macula on OCT.
The right eye underwent PPV without ILM peeling and silicone oil tamponade. Post-operatively, there was slow reattachment of the outer sides of the retinoschisis (Figure 1C). The patient was lost to follow-up due to the COVID-19 pandemic, but later consulted for blurring of vision of the fellow eye. Fortunately, the BCVA had improved to 20/50 OD, but the left eye was worse, even if the BCVA was the same at 20/200.
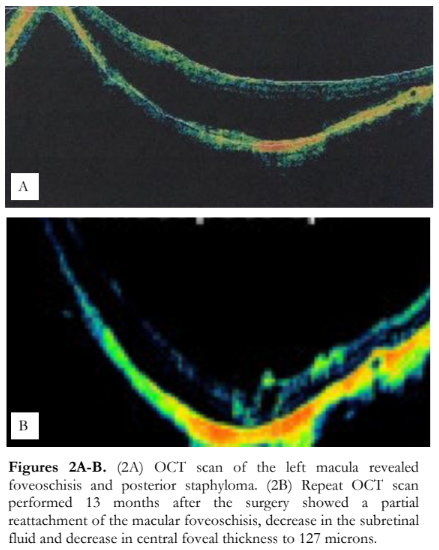
OCT scan of the right macula showed reattached foveoschisis, diffuse thinning of the macula with the central retinal thickness of 134 microns (Figure 1D). On the other hand, OCT scan of the left macula revealed myopic foveoschisis, diffuse thickening of the macula, and central retinal thickness of 582 microns (Figure 2A). The left eye underwent PPV, silicone oil tamponade without ILM peeling for MTM. At the last known post-operative follow-up, visual acuity had improved to 20/60 OS. Repeat OCT scan performed at 13 months after the surgery showed a partial reattachment of the macular foveoschisis, decrease in the subretinal fluid, and decrease in central retinal thickness at 127 microns (Figure 2B).
The third eye with MTM belonged to a 62-year- old man with retinitis pigmentosa and myopia with axial length of 23mm. He consulted for central vision loss of the left eye. Best-corrected visual acuities were 20/50 OD and counting fingers at 2 feet OS. Fundus findings revealed myopic degeneration with posterior staphyloma and prominent temporal peripapillary atrophy in both eyes (Figure 3A). Bony spicules were seen along the arcades and the periphery. OCT findings of the left eye showed myopic retinoschisis with vertical and horizontal traction from the partial separation of the vitreous from the retina. Central field thickness was 662 microns (Figure 3B). The patient underwent PPV with silicone oil tamponade as previously described. Twelve months post-operatively, OCT showed absence of the vitreo- macular traction and a smooth retinal contour but still with a persistent hypo-reflective space. Central field thickness was 373 microns (Figure 3C). At the last known follow-up, 16 months post-surgery, there was marked reduction in the amount of subretinal fluid on OCT with a near-normal central field thickness of 301 microns (Figure 3D). There were only 2 of 9 subfields with p>99% where the persistent fluid was located but most subfields were dry.

DISCUSSION
In this small case series of 3 eyes with MTM, surgical management with PPV and silicone oil injection was performed. In all 3 cases, the ILM was not peeled but extra steps were taken to make sure the cortical vitreous was entirely removed. Triamcinolone actenonide suspension was used to stain the vitreous to ensure its complete removal.
The first eye with MTM had a visual acuity of hand movement and remaining subretinal fluid on repeat OCT scan at 1 month after surgery. But by 3 years, visual acuity had dramatically improved to 20/50 with complete macular attachment. Slow reattachment of retinoschisis associated with MTM has been reported in a published case series and this is certainly true in this case.5
The second eye of the same patient showed more encouraging results with improvement in vision at 1 week postoperative and improved OCT findings at 13 months postoperative. Similar results were also observed in the third eye with MTM that underwent PPV with silicone oil tamponade.
Most cases of MTM with extensive foveoschisis typically progress to foveal detachment with development of a full-thickness macular hole.1,2 In these cases, surgery is the only reasonable option. The optimal timing of surgery remain/s controversial. Different techniques have been proposed.5,6,7 However, all remain challenging even in expert hands.
Nowadays, the standard procedure for MTM is PPV with fovea-sparing ILM peeling. Reports showed that eyes that underwent this method had good anatomic and functional outcomes. Additionally, the post-operative course was not complicated with iatrogenic full-thickness macular hole and foveal re-detachment.5,6 However, this surgical technique has several difficulties. First, the ILM over the fovea can get iatrogenically peeled as the vitreoretinal surgeon maintains his focus on peeling the off-center areas. Second, visualization of the ILM remains difficult even with the use of dyes as there is poor contrast against the atrophic and white retinal pigment epithelium (RPE). Third, ILM peeling can be complicated by trauma to the retinal tissue including inadvertent removal of the inner retinal side of the retinoschisis. This could be avoided with the use of intra-operative OCT; however, access to the equipment remains very limited.
Another innovative surgical technique for the treatment of MTM involves detachment of the macula and temporal retina with a gauge 40 needle, creation of a retinotomy in the temporal retina to loosen it, followed by re-attachment of the macula.4 This technique has a reported successful anatomic outcome of 94%.
While these two surgical techniques have good anatomic and functional outcomes, we propose a simpler technique that could be equally safe and effective in the treatment of MTM: PPV, silicone oil tamponade without ILM peeling. This method avoids the risk of retinal damage associated with ILM peeling. On the other hand, silicone oil tamponade facilitates re-attachment by exerting continuous pressure on the macula. Models have shown that if the eye is sufficiently filled, face-down positioning in the post-operative period is not necessary for the silicone oil to come in contact with the macula. Silicone oil also remains in the eye for several months which allow for slower but safer remodeling of the retina to the posterior staphyloma. This removes the risk of retinal tearing in trying to abruptly conform the retina to the staphyloma present in other techniques. Silicone oil may also help in the closure of full-thickness macular holes in eyes with MTM by preventing fluid from entering the macular hole and dissecting into the deeper layers of the retina. Although silicone oil carries inherent complications such as emulsification, anterior segment migration, glaucoma and others, it is safe in majority of cases. The 3 eyes in this case series had improved visual acuities and reduced central retinal thickness despite the presence of a little fluid on follow-up. No other complications were noted.
Limitations of this case series include differences in the follow-up period among the 3 eyes and use of multiple OCT machines. Further studies are clearly needed to establish the benefits of PPV with silicone tamponade in the treatment of naïve eyes with MTM. Nevertheless, we have shown that PPV, silicone oil tamponade without ILM may be a simple, effective, and safe surgical technique option for the treatment of MTM.
REFERENCES
- Champion MC, Shah VA, Kim LA, 2022. Myopic Traction Maculopathy. December 20, 2022: https://eyewiki.aao.org/Myopic_Traction_Maculopath y. (accessed April 26, 2023).
- Meng J, Chen Y, Cheng K, et al. Long-term progression pattern of myopic tractional maculopathy: outcomes and risk factors. Retina. 2023 Mar 27. Epub ahead of print.
- Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004; 122:1455–1460.
- Guerra RA, Flores V. The Retinal Glide: A new technique for myopic traction maculopathy with retinal detachment. April 19, 2022: https://www.youtube.com/watch?v=hX-zPI22Oso (accessed April 26, 2023)
- Uchida A, Shinoda H, Koto T et al. Vitrectomy for myopic fove oschisis with internal limiting membrane peeling and no gas tamponade. Retina. 2014;34:455-460.
- Figueroa MS, Ruiz-Moreno JM, Gonzalez Del Valle F, et al. Long-term outcomes of 23-gauge pars plana vitrectomy with internal limiting membrane peeling and gas tamponade for myopic traction maculopathy. A prospective study. Retina. 2015;35(9):1836–1843.
- Shimada N, Sugamoto Y, Ogawa M et al. Fovea-sparing internal limiting membrane peeling for myopic traction maculopathy. Am J Ophthalmol. 2012;154:693-701.

