Translation and Validation of the Tagalog Trust in Ophthalmologist Scale
Daphne Viel Cruzat-Tsuru, MD, Jose Ma. D. Martinez, MD, MBA
Department of Health Eye Center, East Avenue Medical Center, Quezon City
Correspondence: Daphne Viel Cruzat-Tsuru, MD
Clinic Address: DOHEC, East Avenue Medical Center, Quezon City
Clinic Phone Number: (632) 89280611 local 757
Email Address: dvctsurumd@gmail.com
Disclaimer: The authors have no financial interests or conflicts of interest to disclose.
Trust is an essential foundation in every relationship including that between physicians and patients. As a multidimensional construct influenced by an individual’s set of inherent beliefs, there are many ways to define ‘trust’ and several measures have been developed to determine its importance in current healthcare practices. What makes determination of trust levels of patients essential, especially in cases wherein long-term management is necessary, is that patients who trust their physicians are more satisfied with their providers and more likely to adhere to the treatment plan advised.1
Determining the level of trust of patients in their physicians is an issue among different stakeholders in the healthcare community. Several behaviors of the physician such as advocacy, compassion, empathy, reliability and dependability, clear and complete communication, ample time given in consultation, appropriate and effective treatment, and honesty and respect towards the patient have been associated with patients’ trust.2 A 2014 systematic review evaluated 7 measures of trust in physician: the Trust in Physician Scale (TiPS), Trust Scale for the Patient-Physician Dyad (TSPPD), the Wake Forest Physician Trust Scale (WFPTS) and its short form, the Abbreviated Wake Forest Physician Trust Scale (A-WFPTS), the Health Care Relationship Trust Scale (HCRTS) and its revision, the Health Care Relationship Trust Scale Revised (HCRTS-R), and lastly, the Trust in Oncologist Scale (TiOS).3 The TiOS was the only population-specific scale developed from the WFPTS which measured cancer patients’ trust in their oncologist. All these measures were assessed using the Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) checklist for quality of design, methods, and reporting of psychometric properties. For the quality of psychometric properties, the Terwee criteria used in the assessment of health status questionnaires and for designing validation studies was applied. The TiOS is an 18- item scale primarily developed in Dutch and subsequently translated into English and validated in English-speaking patients.4,5 It measures a 4-dimensional model of patients’ trust in their physician namely competence, fidelity, honesty, and caring. The scale was developed with consideration of all the relevant dimensions of trust as determined by different studies. Among all the other trust scales, TiOS received the best rating for psychometric properties for the quality of its design, methods, and reporting in accordance with the criteria set by the COSMIN checklist and Terwee criteria, making it an ideal measure to adapt for assessment of trust in ophthalmology patients for this study.3
Psychometric tests are used to objectively assess human behavior or complex ideas such as trust. The process of scale development involves determining the domain to be assessed which in our case is trust, generating items or questions that will help assess it, and validating the initial output to determine its applicability to the population we intend to assess. Validation is then carried out to determine the psychometric properties using statistical techniques such as item analysis and factor analysis.
In this research, we adopted an existing trust scale which was developed for oncology patients and translated it into Tagalog for validation on ophthalmology patients. A useful questionnaire or test scale must be reliable and valid, with the latter being more important. The process of translation and validation of an existing psychometric test or questionnaire is not as cumbersome as the initial test development, but nevertheless it still requires statistical methods to assess the reliability and validity of the questionnaire which will be further discussed in the methodology section.
Permanent visual impairment or vision loss has a significant effect on the quality of life (QOL) of patients and may require life-long visual rehabilitation and follow-up. Because of the impact of visual disabilities, patient trust in the physician provider is deemed important. A study by Muir et al. determined the level of trust of glaucoma patients in their ophthalmologist using the TiPS questionnaire.6 To the best of our knowledge, no population-specific measure in English or Filipino language has been validated to determine the trust of patients in their ophthalmologists. The objectives of this study were to translate and validate the Tagalog version of TiOS and to determine the level of trust of patients in their ophthalmologists. The results of the validated questionnaire may be used by Filipino ophthalmologists on their Tagalog-speaking patients to serve as feedback on their professional relationship as well as to gain insight into their patients’ tendency to comply with the treatment plan.
METHODS
A cross-sectional survey validation design was used in this study. The research protocol had 2 steps namely (1) translation of the TiOS into Tagalog to produce the TTOS and (2) validation of the TTOS.
This study adhered to the basic principles of the Declaration of Helsinki and conformed with the guidelines set forth by the International Council for Harmonization-Good Clinical Practice (ICH-GCP). The hospital Institutional Ethics Review Board approved this research project.
Preparation and Translation of the Test Instrument
The TiOS by Hillen is a self-reported measure designed to determine the level of trust of cancer patients in their physicians. It consists of 18 non-specific questions with a 5-point Likert answering scale; hence, the possibility of its applicability in ophthalmology. It measures four domains namely fidelity, competence, honesty, and caring. The mean trust score is calculated by getting the average of the responses. To test for construct validity, the Filipino Patient Satisfaction Questionnaire (PSQ-18) which likewise has a 5-point Likert answering scale was also administered.7
The translation of the TiOS into Tagalog was carried out following the guidelines outlined by Sousa et al. for translation of scales for use in health care research (Figure 1).8 Permission from the original author to use TiOS questionnaire and adapt it for administration among ophthalmology patients was secured.

For the forward translation, two bilingual translators with excellent fluency in both English and Tagalog languages produced the Tagalog translations. The produced forward translations in Tagalog were then back translated to English by two other bilingual translators. A committee reviewed all translations and determined whether the translated and original versions of the questionnaire achieved semantic, idiomatic, and conceptual equivalence.
Preliminary Testing of Translated Test Material
The pilot testing of the translated material was performed on 30 patients from the Department of Health Eye Center (DOHEC) of the East Avenue Medical Center (EAMC) based on the acceptable sample size for pretesting of questionnaires.9,10,11 After completing the self-administered questionnaire, each respondent was interviewed about what each question meant to ensure that the items retained the same meaning as the original questionnaire. All respondents understood each translated question without difficulties hence the questionnaire was finalized for validation.
Validation Process
The participants for the validation process were Filipino patients from the DOHEC-EAMC. A convenience sampling method was employed with a sample size of 180 patients as determined by a subject-to-item ratio of 10:1.11 Inclusion criteria were adult patients of the DOHEC-EAMC who had been evaluated by ophthalmology residency trainees in at least 3 clinic visits, are able to read and understand written Tagalog, and can answer the questionnaire on their own or with minimal assistance from a relative or companion. Patients who were unable to answer the questionnaire for cognitive or psychiatric reasons, or those who were unable to give consent for participation were excluded from the study.
The following information were collected: (1) socio-demographic data which included gender, age, marital status, level of education, and religion; (2) disease characteristics namely duration of illness, number of consultations at the DOH Eye Center, and number of consultations at outside institutions; (3) whether the patient will likely recommend their ophthalmologist to their friends or family; and (4) how much they trust the Philippine health care system.
A predetermined number of study participants underwent retesting 4 weeks after the initial administration of the questionnaire.
Statistical Analysis
Statistical analyses were performed using the SPSS Version 27 (IBM, USA) and JASP software (University of Amsterdam, the Netherlands). Exploratory factor analysis (EFA) was done for the 18 questionnaire items to explain all variance in the data set and was compared with the original TiOS. The minimum factor loading criteria was set to 0.50. The communality of the scale which indicates the amount of variance in each dimension was also assessed to ensure acceptable levels of explanation. Kaiser-Meyer-Olkin (KMO) index of sample adequacy was determined and a value of > 0.8 was considered adequate. Bartlett’s test of sphericity was also determined with a set p-value of 0.05. Confirmatory factor analysis (CFA) was done to determine if the translated questions fit with the TiOS theoretical 4-dimension model consisting of competence, fidelity, honesty, and caring using the chi-square test and root mean square error of approximation (RMSEA).
Reliability
Internal consistency was measured using Cronbach’s. A value of at least 0.70 reflected adequate internal consistency. Test-retest reliability was measured using the Pearson’s coefficient (p < 0.01). The questionnaire sets that did not show any variance were removed from the statistical analysis since zero variance yielded an undefined Pearson’s coefficient. Inter-item correlations to determine correlation between test questions were computed. Corrected item-total correlation was derived to determine the correlation between individual test items and the total test score, with values not lower than 0.30 deemed acceptable.
Validity
A panel of 6 ophthalmologists determined the content validity of the measures. The item content validity index (I-CVI) was calculated by computing the number of raters with a relevant rating of 3 or 4 per question, divided by the total number of raters.12 Values range from 0 to 1, where a value > 0.79 is considered relevant, a value between 0.70-0.79 means the item needs revision, and a value < 0.70 means the item needs to be removed. Construct validity between trust and satisfaction using the PSQ-18, trust in the healthcare system of the Philippines, and willingness to recommend ophthalmologists to others was computed using Spearman’s correlation with p-value < 0.01.5,13
Exploratory analyses to correlate trust and the respondent’s sociodemographic data (i.e., age, gender, marital status, educational attainment, religion, duration of condition) were done using Spearman’s correlation.5 A p-value of < 0.05 was considered statistically significant.
RESULTS
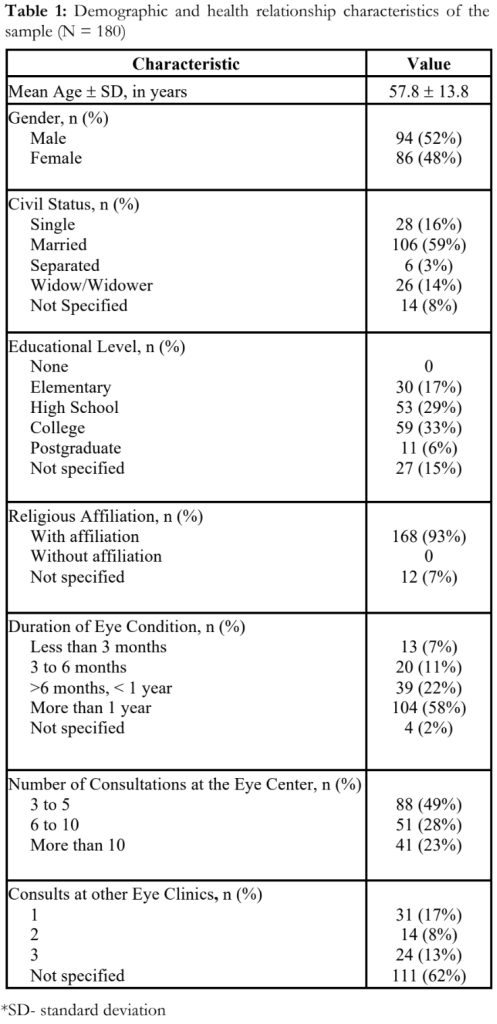
Two hundred (200) study participants answered the Tagalog questionnaire. Twenty (20) questionnaires were excluded due to incomplete data. The demographic data of the 180 study participants is summarized in Table 1.
Factor Analysis
The KMO index measure of sampling adequacy computed was 0.908 and the Bartlett’s test of sphericity was significant (2294.63, p-value < 0.001). EFA was done and a 3-factor model was produced. The criteria for a good model fit used by the TiOS was followed and indicated by a non-significant X2 (p-value < 0.01) and RMSEA <0.06.14 CFA using the theoretical 4-factor model showed a X2 of 174.34 (p- value < 0.001) and RMSEA of 0.07, while the 3- factor model had X2 of 314.02 (p-value < 0.001) and RMSEA of 0.107.
Reliability Test
Reliability of the TTOS was high at Cronbach α of 0.92. Each dimension also showed acceptable internal consistencies with α values of 0.68, 0.70, 0.86, and 0.67 for competence, honesty, fidelity and caring, respectively. Inter-item correlation values ranged from 0.16 to 0.84. Corrected item-total correlations for each question are all above 0.3 and are included in Table 2.
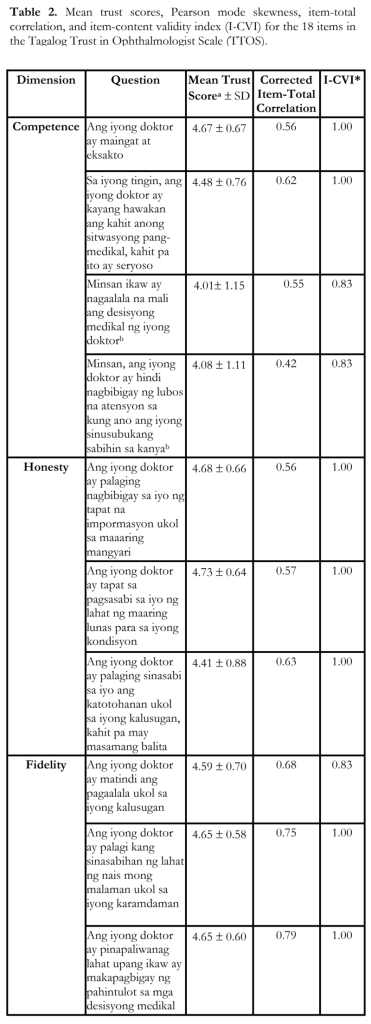
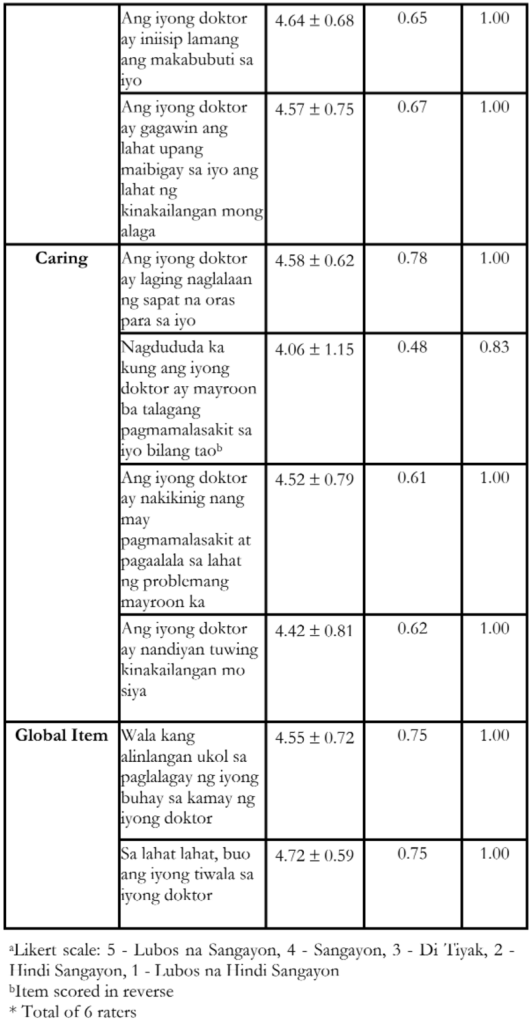
Validity Test
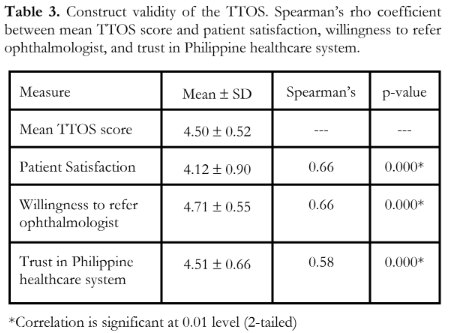
The I-CVI computed for the scale is included in Table 2. There was strong statistically significant positive correlation in the test-retest reliability indicated by Pearson coefficient of 0.84 (p = 0.001). Table 3 shows the construct validity of the TTOS. The Spearman’s rho between trust in ophthalmologist and trust in the healthcare system of the Philippines [rs = 0.58, p-value = 0.000], and willingness to recommend their ophthalmologist to others [rs = 0.66, p-value = 0.000] showed statistically significant positive correlation.
Exploratory Analyses
Spearman’s rho (rs) between mean TTOS score and age [rs = 0.081, p-value = 0.278], sex [rs = 0.126, p-value = 0.092], and duration of illness (rs = 0.030, p-value = 0.687] showed non-significant weak positive correlation. While the number of consults [rs = -0.63, p-value= 0.41], civil status [rs = -0.113, p-value = 0.065], religiosity [rs = -0.061, p-value = 0.209], and educational attainment [rs = -0.073, p- value= 0.332] showed non-significant negative correlation.
DISCUSSION
Several studies have reported that trust is essential in creating a positive patient-physician relationship.4,6.15 As healthcare systems evolve from being primarily an autonomous setup to a patient-centered approach to management, determination of trust has been the focus of several measures.
In this study, sampling was adequate as supported by a KMO value greater than 0.8. The p-value of the resulting Bartlett’s test of sphericity was lower than our set significance of 0.05 which translates to equality of the variance; hence, the dataset was deemed suitable for factor analysis.
Factor analysis is an important statistical step in validation of psychometric measures. It is used to determine if the questionnaire items can be grouped into factors which represent different dimensions of the construct being measured. Two types of factor analysis are available: EFA and CFA. If there is no data regarding the factor structure of the questionnaire, its factor structure can be analyzed using EFA. However, if there is prior analysis on the test questionnaire, a CFA is more appropriate to test if the data fits the existing factor structure.16 In our study, EFA was done to compare it with the TiOS. Results of the EFA showed good correlation between all items resulting to a 3-factor model. However, the questions grouped per statistical factor generated did not belong to the same groups in the theoretical model from the TiOS. CFA on the theoretical 4-factor model following the TiOS did not show a good fit with a significant X2 value and a higher RMSEA. On testing the 3-factor model derived from the EFA, values still did not show a good fit.
Similarly, in the TiOS, their theoretical 4-dimension model failed to converge on EFA suggesting a more appropriate one-dimensional model since meaningful dimensions of trust based on the statistical 3-factor outcome could not be determined. In simpler terms, the questions that were grouped statistically into the 3 factors were not coherent as a group, but when taken altogether, these items did measure ‘trust’. They performed CFA on the one-dimensional model which did not show a good fit, but upon testing the theoretical 4-factor model, a good statistical fit was noted. Because of these findings, they concluded that conceptually, a one-dimensional model gives a more meaningful explanation to their findings.5,15 With our findings, we agree that a one-dimensional model gives a more meaningful interpretation, and that further inquiry is needed to explain the differences in the quantitative findings versus the qualitative findings that patients can distinguish trust based on the preset dimensions.
Reliability of the test is considered as the consistency of the survey results which can be measured by its internal consistency (i.e Cronbach), test-retest reliability, and inter-rater reliability. The reliability of the TTOS was quite good as supported by a high Cronbach and there is also evidence for a test-retest reliability as shown by a good Pearson coefficient, meaning that there is a strong consistency in test results over time. The high corrected item-total correlation showed a good correlation between individual item scores and the overall assessment score of the questionnaire and reflects the reliability of the scale used. A value of at least 0.40 in the item-correlation test means each test question correlates well with the over-all scale and thus measures the same construct, which is trust, and in our analysis, all items have acceptable item- total correlation values.
Validity testing determines whether the test or instrument is measuring what it was designed to measure through content validity and construct validity assessment. Content validity as shown by a high I-CVI (>0.80) reflects that all items were relevant. Further analysis of the responses supported good construct validity of the TTOS as supported by significant correlation of scores with satisfaction, willingness to refer to their ophthalmologist, and trust in the Philippine healthcare system.
The exploratory analyses on mean TTOS scores and sociodemographic data of the participants all showed weak correlations which are statistically not significant.
These findings support the TTOS as a reliable and valid test to determine the trust of a Filipino patient in his or her ophthalmologist.
This study was performed at one government eye center and therefore the study findings may not apply in other institutions. In our eye center, patients are seen by rotating ophthalmology residents and consultants. Hence, the measured trust reflects the patients’ trust in the ophthalmology team as a whole and not specifically to a single ophthalmologist.
In conclusion, the TTOS is a reliable and valid tool in determining the level of trust of Filipino patients in their ophthalmologists. This test may be used in ophthalmology patients to help their physician improve their services and enhance their relationship with their patients.
REFERENCES
- Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728-39.
- Rolfe A, Cash-Gibson L, Car J, et al. Interventions for improving patients’ trust in doctors and groups of doctors. Cochrane Database Syst Rev. 2014;2014(3):CD004134.
- Müller E, Zill JM, Dirmaier J, et al. Assessment of trust in physician: a systematic review of measures. PLoS One. 2014;9(9):e106844.
- Hillen MA, de Haes HC, Smets EM. Cancer patients’ trust in their physician-a review. Psychooncology. 2011;20(3):227-41.
- Hillen MA, Koning CC, Wilmink JW et al. Assessing cancer patients’ trust in their oncologist: development and validation of the Trust in Oncologist Scale (TiOS). Support Care Cancer. 2012;20(8):1787-95.
- Muir KW, Santiago-Turla C, Stinnett SS et al. Glaucoma patients’ trust in the physician. J Ophthalmol. 2009;2009:476726.
- Dorado-Baesa M, Pumanes C. Development of a Filipino questionnaire on the factors affecting the level of patient satisfaction at the MDH-DFCM out-patient clinic (April, 2010 and September, 2010). The Filipino Family Physician. 2011;49(1):35-49
- Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross- cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. 2011;17(2):268-74.
- Perneger TV, Courvoisier DS, Hudelson PM, Gayet- Ageron A. Sample size for pre-tests of questionnaires. Qual Life Res. 2015;24(1):147-51.
- Nunnally J. An Overview of Psychological Measurement. In: Wolman B, ed. Clinical Diagnosis of Mental Disorders. 1st ed. New York, NY: Springer; 1978;119-133.
- Tsang S, Royse CF, Terkawi AS. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J Anaesth. 2017;11(Suppl 1):S80-S89.
- Zamanzadeh V, Ghahramanian A, Rassouli M, et al. Design and Implementation Content Validity Study: Development of an instrument for measuring Patient- Centered Communication. J Caring Sci. 2015;4(2):165-78.
- Strauss ME, Smith GT. Construct validity: advances in theory and methodology. Annu Rev Clin Psychol. 2009;5:1- 25.
- Hillen MA, Butow PN, Tattersall MH et al. Validation of the English version of the Trust in Oncologist Scale (TiOS). Patient Educ Couns. 2013;91(1):25-8.
- Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613-39.
- de Vet HC, Adèr HJ, Terwee CB et al. Are factor analytical techniques used appropriately in the validation of health status questionnaires? A systematic review on the quality of factor analysis of the SF-36. Qual Life Res. 2005;14(5):1203-1224.

