Comparison of the Clinical Profile of Patients with Glaucoma Between Private and Government Clinics in the Philippines
Edgar Felipe U. Leuenberger, MD, DPBO,1 James Paul S. Gomez, MD, DPBO,1 Robert Edward T. Ang, MD, DPBO,1 Maria Imelda Yap-Veloso, MD, DPBO,1 Joseph Anthony J. Tumbocon, MD, DPBO,2 Jose Ma. D. Martinez, MD, DPBO,3 John Mark S. De Leon, MD, DPBO,3 Nilo Vincent FlorCruz, MD, DPBO,4 Rainier Victor A. Covar, MD, DPBO,4 Irene R. Felarca, MD, DPBO,1 Denise Polly Chao-Po, MD, DPBO,2 Shalam Siao-Mariano, MD, DPBO,3 Marie Joan Therese D. Balgos, MD, DPBO,4 Noel D. Atienza, MD, DPBO2
For the Philippine Glaucoma Society
1Asian Eye Institute, Makati City, Philippines
2Eye Institute, St. Luke’s Medical Center, Quezon City, Philippines
3The Department of Health Eye Center, East Avenue Medical Center, Quezon City, Philippines
4Department of Ophthalmology and Visual Sciences, Philippine General Hospital, Manila, Philippines
Correspondence: Edgar Felipe U. Leuenberger, MD, DPBO
Asian Eye Institute
9F Phinma Plaza, Rockwell Center, Makati City, Philippines
Disclosure: This study was funded by an unrestricted grant from Santen Pharmaceutical Co. Ltd. Supplemental support was received from the Philippine Glaucoma Society and the Asian Eye Institute. The corresponding author and study team independently conducted all phases of the research and assume full accountability for its content.
Glaucoma is one of the leading causes of irreversible blindness worldwide, and it is expected to affect 111.8 million individuals by 2040. In Asia alone, the number of individuals with primary open-angle glaucoma (POAG) and primary angle-closure glaucoma (PACG) is expected to increase to 42.32 and 24.50 million, respectively, by 2040.1
The estimates described above have been derived from pooled glaucoma prevalence calculations in population-based studies1 that did not include data from the Philippines. The prevalence of glaucoma as the third leading cause of blindness in the Philippines may have been underestimated in a previous study because the diagnosis was only based on optic nerve characteristics or a previous diagnosis or surgery.2 No other local studies have estimated the overall prevalence of glaucoma in the country, although individual reports from different hospitals are available. From 2000 to 2002, 836 patients in the Philippine General Hospital, the premiere government hospital of the country, were diagnosed with glaucoma, with PACG and POAG accounting for 29.5% and 14.4% cases, respectively. The remaining cases were diagnosed with various types of secondary glaucoma.3 Subsequently, data from St. Luke’s Medical Center, a private tertiary hospital, showed that 570 patients were diagnosed with glaucoma between 2010 and 2014, with PACG, POAG, and other glaucoma types accounting for 24.78%, 22.80%, and 52.42% cases, respectively.4 Despite these reports, the actual prevalence of this disease in the country has not been elucidated, and population-based studies are required to obtain estimates for the prevalence and incidence of glaucoma in the Philippines. Because such studies will require extensive planning, resources, and time, hospital-based studies can be conducted to derive initial data. Although data from such studies may differ from actual population estimates, they will provide a general overview or the initial information necessary for population-based studies.5,6
In 2017, the health expenditure in the Philippines was estimated to comprise 3.7% of the total income of families with a higher socioeconomic status (SES) and only 1.9% of the total income of families with a lower SES (bottom 30%).7 Considering that only a fraction of the total medical expenses are covered by the social health insurance in the Philippines, which is often not enough to cover for the expenses in private centers, a diagnosis of glaucoma may prove to be onerous for a regular Filipino family. As a result, families belonging to lower income classes usually opt for care in government centers. Currently, there are only 13 private and 13 government eye institutions that are officially accredited by the Philippine Board of Ophthalmology. Thus, considering a total population of 105 million individuals, only 16 ophthalmologists per million individuals are estimated to cater to eye health in the Philippines. Moreover, specialized care for glaucoma is received only by 52 members of the Philippine Glaucoma Society (PGS) and a few nonmembers, and there are only four glaucoma fellowship programs recognized by PGS.
An extensive review of online repositories for scholarly literature (Google Scholar, PubMed, and the Philippine Journal of Ophthalmology) did not yield prior studies that compared patients with glaucoma between government and private centers in the Philippines and abroad. Accordingly, the aim of the present study was to describe and compare the demographic and clinical characteristics of patients with glaucoma managed at private and government institutions in the Philippines between 2009 and 2014.
METHODOLOGY
We retrospectively reviewed the medical records of patients with glaucoma who were managed between January 2009 and December 2014 at two private [Asian Eye Institute (AEI), St. Luke’s Medical Center Eye Institute (SLMC-EI)] and two government [Department of Health Eye Center East Avenue Medical Center (DOH-EAMC), Philippine General Hospital Department of Ophthalmology and Visual Sciences (PGH-DOVS)] institutions in the Philippines. The five-year period was selected based on feasibility and availability of patient records from the four hospitals. At least 300 records were aimed to be included per center. Institutional Review Board (IRB)/Ethics Committee approval was obtained from all centers, and the study protocol conformed to the standards set by the Declaration of Helsinki. Data confidentiality was ensured at all times.
A research team comprising consultants and fellows associated with the respective institutions collected data for the study after selecting records by convenience sampling. We included subjects diagnosed with unilateral or bilateral glaucoma on the basis of the International Society of Geographic and Epidemiologic Ophthalmology classification.8 Glaucoma suspects (GS), defined by the presence of a family history, visual field defects, increased intraocular pressure (IOP), optic nerve abnormalities, and/or occludable angles without peripheral anterior synechiae, were also included. Subjects with incomplete data and those without documented structural or functional evidence of disease as per the clinical exam and ancillary procedures were excluded.
We encoded pertinent demographic data (age, gender, and ethnicity) as well as clinical data (ancillary examinations and treatments) in a standardized case report form. We included only one eye per patient in our analysis, selecting the eye with poorer visual acuity, higher IOP, and/or a larger cup-to-disc ratio (CDR) for cases with bilateral disease.
Statistics and Data Analysis
All data were statistically encoded using SPSS 16 (IBM Corporation, Armonk, New York, USA). Descriptive statistics (mean, range, percentages) were used to consolidate quantitative and qualitative variables. Data evaluation was done either through between-group analysis (B) or within-group analysis (W). To compare proportions between private and government institutions (B), we used the subtotals of each disease entity and other variables as denominator to compute for percentages. To compare proportions within each institution type (W), the subgroup totals were used. Results are labeled in the tables accordingly.
RESULTS
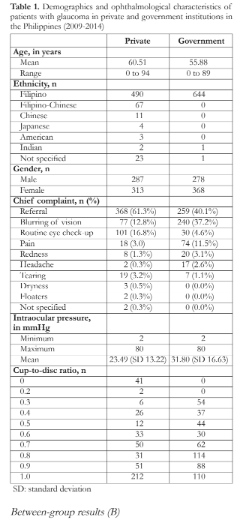
We analyzed a total of 1246 records (AEI: 300, SLMC-EI: 300, PGH-DOVS: 351, DOH-EAMC: 295). The majority of patients were women (55%) and Filipino (91%). Those of foreign descent were mostly seen in private institutions. The mean age at presentation was 60.51 and 55.88 years in the private and government groups, respectively. Half of the total number of patients had been referred to the glaucoma department (368 in the private institutions and 259 in the government institutions). Other reasons for the hospital visits included, in descending frequency, blurring of vision, routine eye check-up, pain, redness, headache, and tear, among others (Table 1).
In both institution types, IOP ranged from 2 to 80 mmHg, with mean values of 23.49 and 31.80 mmHg in the private and government groups, respectively. Of the 539 patients who underwent vertical CDR measurements in the government institutions, 17% (91) showed normal findings while 83.1% (448) showed a CDR of ≥0.5. Similarly, of the 423 patients with CDR measurements in the private institutions, 8.0% (34) and 91.9% (389) showed CDRs of 0.2–0.4 and ≥0.5, respectively. Forty-one (41) patients with a CDR of 0 in the private group were not included in our analysis because their CDR measurements were deemed possibly inaccurate (Table 1).
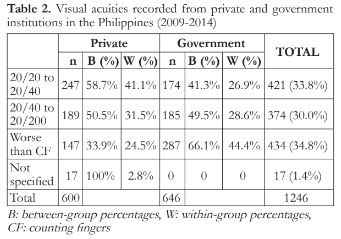
More private (58.7%) than government (41.3%) patients exhibited visual acuities (VAs) ranging from 20/20 to 20/40, while an almost equal number of private (50.5%) and government (49.5%) patients exhibited VAs from 20/40 to 20/200. Patients with VA worse than counting fingers were more frequent in the government (66.1%) than in the private institutions (33.9%) (Table 2).
Government institutions registered a larger number of patients with PACG (private: 40.2%, government: 59.8%) whereas private institutions registered more patients with POAG (private: 61.3%, government: 38.7%). Cases of normal tension glaucoma (private: 63.9%, government: 36.1%), ocular hypertension (private: 92.3%, government: 7.7%), and glaucoma suspect (private: 80.4%, government: 19.6%) were more frequent in the private institutions, whereas secondary glaucoma (private: 29.7%, government: 70.3%) were more frequent in the government institutions (Table 3).

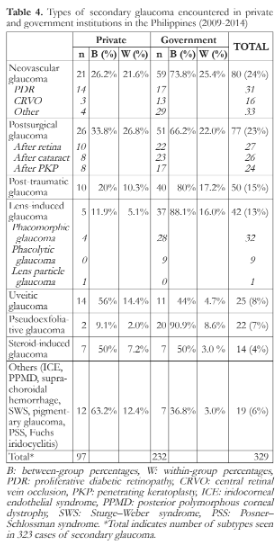
Government institutions (73.8%) had more cases of neovascular glaucoma (NVG) compared to private institutions (26.2%). NVG primarily occurred as a sequela of diabetic retinopathy or central retinal vein occlusion. Post-surgical glaucoma occurred after cataract surgery, retinal detachment surgery, or penetrating keratoplasty (private: 33.8%, government: 66.2%) (Table 4).
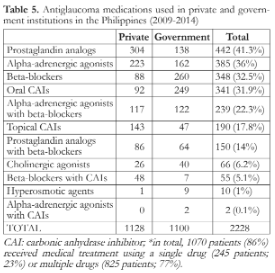
In total, 1070 patients (86%) received medical treatment using a single drug (245 patients; 23%) or multiple drugs (825 patients; 77%). The top 3 preferred medications in private centers were prostaglandin analogs (PGA), alpha-adrenergic agonists, and topical carbonic anhydrase inhibitors (CAI). The government institutions preferred beta-blockers, oral CAIs, and alpha-agonists as the top 3 medications (Table 5).
Laser iridotomy was found to be more frequently done in government institutions (52.5%) compared to private institutions (47.5%). Diode cyclophotocoagulation was also more frequent in government institutions (76.2%) compared to private institutions (23.8%). In contrast, laser trabeculoplasty was more frequent in private (87.8%) compared to government institutions (12.2%) (Table 6).

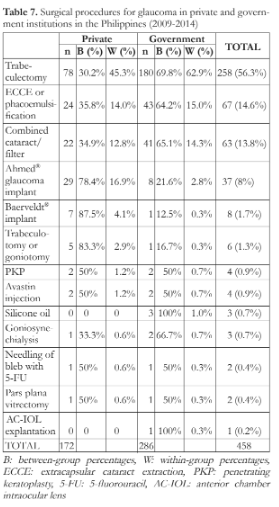
More trabeculectomy procedures were performed in government (69.8%) compared to private centers (30.2%). Lens extraction either by phacoemulsification or extracapsular lens extraction was also more frequent in government than private centers (private: 35.8%, government: 64.2%) as well as combined trabeculectomy with lens extraction (private: 34.9%, government: 65.1%). Notably, the implantation of glaucoma drainage devices was more common in the private institutions (Ahmed® implant: 78.4% in the private and 21.6% in the government groups; Baerveldt® implant: 87.5% in the private and 12.5% in the government group) (Table 7).
Within-group results (W)
Majority of patients in private institutions were recorded to have VA within 20/20 to 20/40 (41.1%). In contrast, most patients from government institutions had VA of worse than counting fingers (44.4%) (Table 2).
PACG was the most frequent glaucoma subtype in both private (27.3%) and government institutions (37.8%). This was followed by secondary glaucoma (private: 16.0%, government: 35.1%) and POAG (private: 26.7%, government: 15.6%) (Table 3).
Post-surgical glaucoma was the most frequent secondary glaucoma type in private institutions (26.8%) whereas NVG was the most frequent type in government institutions (25.4%). Other types of secondary glaucoma included post-traumatic glaucoma, lens-induced glaucoma, uveitic glaucoma, pseudoexfoliative glaucoma, steroid-induced glaucoma, and others (Table 4).
Laser iridotomy was the most commonly performed laser treatment in both institution types (private: 40.6%, government: 41.1%). The second most frequent laser treatment was diode cyclophotocoagulation in government institutions (32.8%) and laser trabeculoplasty in the private institutions (31.2%). Table 6 lists the other commonly used laser procedures.
In both institution types, trabeculectomy was the most commonly performed surgical procedure (private: 45.3%, government: 62.9%) followed by lens extraction (private: 14.0%, government: 15.0%). Other procedures done for glaucoma patients are listed in Table 7.
DISCUSSION
Studies describing the profile of glaucoma in private and government institutions are scarce, and to the best of our knowledge, the present study conducted in the Philippines is the first to compare the glaucoma profile between the two institution types using a single protocol involving one case report form. We hypothesized that the distribution of glaucoma types is unique to each institution type on the assumption that SES influences the healthcare-seeking behavior of patients. Those who seek consultation at government clinics exhibit delayed consultation because of a lower SES. These patients are expected to have poorer VA, a larger CDR, and end-stage glaucoma, which result in an increased rate of cyclodestructive procedures. On the other hand, private centers cater to patients with higher SES who have the means to consult more often and undergo earlier interventions. These patients are often found to be cases of ocular hypertension (OHT) or glaucoma suspects.9
We found that half of the patients in the private institutions were referred by nonglaucoma specialists. Referrals in government clinics were generally prescreened by the respective general ophthalmology departments. Although this differentiates the patient flow between the institution types, it emphasizes the role of general ophthalmologists in screening patients for possible glaucoma.
The clinical profile of the government patients in our study was similar to that of patients in the study by FlorCruz et al., who found that government patients do tend to have poorer VA, higher IOP, and a larger CDR at presentation. The authors concluded that patients who visit government centers tend to seek consultation only when the disease is symptomatic or late in the course of the disease because of financial constraints.3
Primary glaucomas accounted for the majority of cases in both private and government institutions. Within-group analysis showed that PACG was predominant in both institution types which is consistent with previous local studies.3,4 Between-group analysis showed that there were more cases of POAG in private institutions. If we assume that private patients have higher SES, their ability to have regular eye care visits increases the identification of POAG even during the early, asymptomatic stages.
In total, POAG (20.9%) was more frequent than NTG (6.7%) in both institution types. Conversely, population studies from Japan and Korea found that NTG (2.7%–3.6%) was more common than POAG (0.3%–0.8%) in adults.10,11 We also found that glaucoma suspects in the private institutions outnumbered those in the government institutions. This may be attributed to the larger proportion of eyes with a CDR of ≥0.5 in the private institutions, which also registered a larger number of patients with OHT. These findings are in agreement with previous observations that patients with higher SES were often diagnosed as cases of OHT or GSs, whereas those with advanced glaucoma subtypes exhibited a lower SES.9
The cumulative frequency of secondary glaucoma in our study was 25.9% from both institution types. In between-group analysis showed that more of these cases were seen in the government institutions, with NVG being the most common subtype. Most of these cases arose as complications of diabetes. This is in accordance with the findings of an international study where NVG occurred secondary to diabetic retinopathy in 39.7% cases.12 Socioeconomic factors such as low income and educational level have been attributed to the development of NVG in patients with diabetes; this may explain the higher frequency in government institutions.13 Within-group analysis showed that the leading cause of secondary glaucoma in private institutions was ocular surgery. This may be attributed to postoperative referrals by multiple eye doctors from other institutions.
Notably, the most frequently prescribed medications in the private institutions differed from those in the government institutions. PGAs, alpha-adrenergic agonists, and topical CAIs are presumed to be prescribed more often to private patients because they can afford more expensive medications. Medications such as beta-blockers and alpha-adrenergic agonists are often prescribed as cheaper alternatives in government centers. The use of oral CAIs in the government institutions in our study also reflects the severity of the glaucoma types seen in these institutions. A study in India found that the average cost of glaucoma medications was found to increase by 1.7 to 3.6-fold as the glaucoma severity progressed from asymptomatic to end-stage.9 In addition, the expenditure for long-term glaucoma therapy may consume as much as 123% of the monthly gross income of patients with a low SES.14
Cumulatively, laser iridotomy was the most frequent treatment modality in both institution types. This agrees with the results of FlorCruz3 and Martinez4 with the latter also showing predominance of iridoplasty. The high frequency of laser trabeculoplasty in the private institutions reflect the accessibility of this treatment for patients with a higher SES and the ability of private centers to acquire new equipment more readily than government centers, where audit processes may stall acquisition. Between-group analysis showed that the use of diode cyclophotocoagulation was more common in government institutions. However, the preference for this treatment modality is unknown.
Previous local studies found trabeculectomy to be the most common surgical procedure for glaucoma which aligns with our within-group analysis for both institution types.3,4 However, we found that implantation of glaucoma drainage devices was more frequent in the private institutions using between-group analysis. Again, this suggests that patients with a low SES may have limited access to appropriate and costly interventions.
Collectively, it is our impression that the differences between the private and government institutions may be attributed to the SES of the patients. Those with a lower SES tend to have advanced conditions and may be inclined to delay consultations in government centers. Those with a higher SES are often diagnosed with milder forms of glaucoma. SES also dictates the treatment, as shown by the discrepant choices of medications in the two institution types and the greater access to equipment-dependent procedures such as selective laser trabeculoplasty in the private institutions. Future studies are suggested to look into the association between SES, glaucoma severity, and KAP (knowledge, attitudes, and practices) of patients. Likewise, quality of care between government and private institutions should also be compared.
This study has several limitations. First, hospital-based studies, such as the present one, have limited ability to extrapolate the true prevalence of the disease for the entire population. Nevertheless, they can provide useful information for future epidemiological studies.5,15 Second, we used convenience sampling, wherein charts were gathered based on accessibility and availability at the time of data collection. Furthermore, it enabled us to achieve the sample size in a fast and inexpensive way. We acknowledge that this sampling method only assumes that members of the target population are homogenous and that there would be an inconsequential difference from findings obtained in a research-based on random sampling. However, we may have included outliers in the population and may not have quantified their probabilities, which increased the risk of selection bias.16 This limitation should be kept in mind when our findings are compared with those of studies based on randomly selected subjects. Finally, our data may not be representative of the different private and government institutions across the country. Furthermore, the comparison of individual institutions in this study was not part of our objective. The homogeneity of the subpopulations was not analyzed.
In conclusion, our findings suggest that the profile of patients with glaucoma differs between private and government institutions in the Philippines. PACG was found to be the most common glaucoma subtype in both private and government institutions. When frequencies are compared between groups, private centers had more cases of POAG, NTG, and OHT while government centers registered a larger number of PACG and secondary glaucoma. Although the generalizability of these findings to all private and government centers in the country may be limited, our study provides preliminary data that can aid in the formulation of adequate health policies, construction of a uniform standardized glaucoma registry, and execution of future population-based studies. We also believe that these findings can be used to improve the training of future practitioners through the provision of collaborative experience in both government and private glaucoma fellowship programs.
REFERENCES
1. Tham YC, Li X, Wong TY, et al. Global prevalence of glaucoma and projections of glaucoma burden through 2040. Ophthalmology. 2014;121:2081-2090.
2. Cubillan LDP and Olivar-Santos EO. Third national survey of blindness. Philipp J Ophthalmol. 2005;30(3):100-114.
3. FlorCruz NV, Joaquin-Quo R, Silva PAS, and Khu PM. Profile of glaucoma cases seen at a tertiary referral hospital. Philipp J Ophthalmol. 2005;30(4):161-165.
4. Martinez JM and Hosaka MA. Clinical profile and demographics of glaucoma patients managed in a Philippine tertiary hospital. Philipp J Ophthalmol. 2015;40:81-87.
5. Obeidan SA, Dewedar A, Osman E, and Mousa A. The profile of glaucoma in a tertiary ophthalmic university center in Riyadh, Saudi Arabia. Saudi Journal of Ophthalmology. 2011;25:373-379.
6. Ruano-Ravina A, Perez-Rios M, and Barros-Dios JM. Population-based versus hospital-based controls: are they comparable. Gac Sanit. 2008;22(6):609-13.
7. Philippine Statistics Authority. Annual Poverty Indicators Survey 2017; final report. 2018.
8. Foster PJ, Buhrmann R, Quigley HA, and Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86:238-242.
9. Chakravarti T. The association of socioeconomic status with severity of glaucoma and the impacts of both factors on the costs of glaucoma medications: a cross-sectional study in West Bengal, India. J Ocul Pharmacol Ther. 2018;Jul/Aug;34(6):442-451.
10. Kim C, Seong G, Lee N, and Song K. Prevalence of primary open angle glaucoma in central South Korea: The Namil study. Ophthalmology. 2011;118:1024-1030.
11. Iwase A, Suzuki Y, Araie M, et al. The prevalence of primary open angle glaucoma in Japanese: The Tajimi study. Ophthalmology. 2004;111:1641-1648.
12. Liao N, Li C, Jiang H, et al. Neovascular glaucoma: a retrospective review from a tertiary center in China. BMC Ophthalmology. 2016;16:14.
13. Lazcano-Gomez G, Soohoo JR, Lynch A, et al. Neovascular glaucoma: a retrospective review from a tertiary eye care center in Mexico. J Curr Glaucoma Pract. 2017;11(2):48-51.
14. Nayak B, Gupta S. Kumar G, et al. Socioeconomics of long-term glaucoma therapy in India. Indian J Ophthalmol. 2015;63:20-4.
15. Das J, Bhomaj S, Chaudhuri Z, et al. Profile of glaucoma in a major eye hospital in North India. Indian Journal of Ophthalmology. 2001;49(1):25-30.
16. Etikan I, Musa SA, and Alkassim RS. Comparison of convenience sampling and purposive sampling. American Journal of Theoretical and Applied Statistics. 2016;5(1):1-4.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.com) for the English language editing.

